Jorn Bo Thomsen1, Jin Ye Yeo2
1Department of Plastic Surgery, Odense University Hospital, Denmark; 2GS Editorial Office, AME Publishing Company
Correspondence to: Jin Ye Yeo. GS Editorial Office, AME Publishing Company. Email: editor@glandsurgery.org
This interview can be cited as: Thomsen JB, Yeo JY. Meeting the Editorial Board Member of GS: Dr. Jorn Bo Thomsen. Gland Surg. 2024. https://gs.amegroups.org/post/view/meeting-the-editorial-board-member-of-gs-dr-jorn-bo-thomsen.
Expert introduction
Dr. Jorn Bo Thomsen (Figure 1) is a consultant plastic surgeon at Odense University Hospital in Denmark. He was educated in Plastic and Reconstructive Surgery at the University of Southern Denmark, as well as at Odense University Hospital and Lillebaelt Hospital in Vejle.
Dr. Thomsen is a Professor of Plastic Surgery at the Department of Clinical Research, University of Southern Denmark. His principal research interest is the refinement and development of new surgical techniques within the field of immediate and delayed breast reconstruction. The main focus has been the refinement of direct-to-implant breast reconstruction and the development and refinement of delayed breast reconstruction using the thoracodorsal artery perforator flap (TDAP) and deep inferior epigastric artery perforator (DIEP) flap reconstruction, as well as lymphedema treatment. Dr. Thomsen also conducts research within the field of general plastic surgery and is especially interested in perforator-based surgery, employing perforator flaps for reconstruction in the breast, face, limbs, and body. Dr. Thomsen is a member of the Editorial Board of Gland Surgery and Annals of Breast Surgery, and is also a member of the board of the Danish Microsurgical Society.
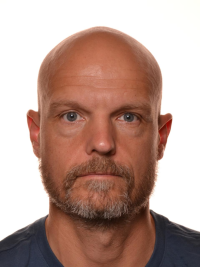
Figure 1 Dr. Jorn Bo Thomsen
Interview
GS: What motivated you to pursue plastic and reconstructive surgery?
Dr. Thomsen: I have always been creative and innovative. I find plastic surgery to be the most innovative and creative surgical specialty and find great joy in working as a plastic surgeon.
GS: Could you provide an overview of the current landscape of publications in breast reconstruction?
Dr. Thomsen: Currently there is a focus on several different topics within breast reconstruction.
1) Immediate breast reconstruction:
There is a focus on pre- and subpectoral breast reconstruction comparing the possible benefits and limitations of the two surgical approaches with a focus on decreasing breast animation deformity, limitation of postoperative pain, and risk of developing rippling over time.
2) Autologous breast reconstruction:
Refinement of autologous breast reconstruction is an ongoing topic currently focusing on improving surgical techniques for the deep inferior epigastric perforator (DIEP) flap and alternative free flaps, decreasing time for surgery and enhancing recovery after surgery. There has also been an increased number of publications regarding muscle sparing or perforator-based pedicled flaps for breast reconstruction with and without implants, which is a sort of hybrid autologous and implant-based breast reconstruction.
3) Sensate breast reconstruction:
The techniques for sensate flaps have developed over time and the techniques for sensate reconstructions for both immediate implant-based breast reconstruction and autologous breast reconstruction are well-described and papers about this subject are currently being published in greater numbers.
4) Robotic surgery:
There is a rapid increase in publications describing the use of robotic-assisted surgery for mastectomy for improving mastectomy flaps prior to reconstruction, dissection of free flaps for reconstruction as well as robotic-assisted microsurgical anastomosis for free flap breast reconstruction. Robotics will likely increase the lifespan of a microsurgeon.
5) Oncoplastic surgery:
Recently there has been an increased focus on oncoplastic surgery compared to immediate breast reconstruction due to better survival in the oncoplastic group. We can foresee that there will be more focus on this subject soon.
GS: Were there any advancements in surgical techniques of breast reconstruction that hold significant promise or impacted your practice?
Dr. Thomsen: I find the use of combined pedicled perforator flaps for breast reconstruction promising in patients who want breast reconstruction without the use of implants. This combined technique is especially interesting in massive weight loss patients who need breast reconstruction in combination with body contouring. This is an exciting topic of our current research.
GS: Your research focuses on refining breast reconstruction. Could you elaborate on the kinds of refinement that you mainly focus on? What is the significance of these refinements?
Dr. Thomsen:
1) Acellular dermal matrixes (ADMs) and meshes:
I have worked with refinements of both immediate implant-based breast reconstruction and autologous breast reconstruction. Over the years, I have refined our approach to immediate implant-based breast reconstruction using different kinds of ADMs and meshes going from mostly skin-sparing mastectomies to more nipple areolar complex (NAC)-sparing mastectomies and reconstructions.
2) Hydrodissection for mastectomy:
More than a decade ago, I introduced the use of hydrodissection for mastectomy prior to breast reconstruction to achieve the best possible mastectomy flaps for breast reconstruction. This is done by thorough removal of the glandular tissue while sparing the subcutaneous fat and vascularity of the skin. The technique has since then been further refined in close collaboration with colleagues and I believe that it made a difference in our published results.
3) Subpectoral to prepectoral:
We have changed our approach from merely subpectoral implant placement in immediate breast reconstruction towards more prepectoral reconstructions depending on patient wishes and the available tissue. In doing so, we have conducted several studies on breast animation deformity.
4) Perforator flaps:
I introduced the use of the propeller thoracodorsal artery perforator (TDAP) flap in combination with an implant and an ADM to replace the musculocutaneous latissimus dorsi (LD) for both immediate and delayed breast reconstruction. Lately, we have combined the TDAP with different pedicled perforator flaps. A pedicled superior epigastric artery perforator (SEAP) flap from the epigastric area and a pedicled internal mammary artery perforator (IMAP) flap from the opposite breast can be stacked for added volume and projection.
GS: What specific aspects of breast reconstruction research do you believe have been overlooked or received insufficient attention?
Dr. Thomsen: The boundaries of angiosomes have been somewhat overlooked due to emphasis on scar placement rather than topographical changes. A wide range of new advances and refinements are continuously being made and tested against previous methods. It is a pendulum that swings back and forth.
GS: Moving forward, what do you think should be the direction of breast reconstruction? Could you share any ongoing projects you are currently involved in?
Dr. Thomsen: The use of autologous flaps for breast reconstruction will develop further in the years to come, both refinements in free flap breast reconstruction as well as in pedicled perforator flap breast reconstruction. I am currently working on a novel combined perforator flap solution that is a promising task for the right indication. There is also increased focus on innervated breast reconstruction, implant-based as well as autologous reconstruction. In regard to implant-based breast reconstruction, the use of smooth implants for breast reconstruction will increase due to breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) and the demand for late explantation with autologous flaps is likely to increase. The use of robotic-assisted surgery and reconstruction will most definitely increase at a rapid pace in the years to come.
GS: Other than being a surgeon, you are also an educator. What are some values and wisdom that you impart to your students? How do you see these values influencing the trajectory of their medical careers?
Dr. Thomsen: The future of surgery resides upon future generations of surgeons. I wish to encourage my future colleagues to achieve their goals by involving them in my research and inspiring them to do great things.
GS: How has your experience been as an Editorial Board Member and Honorary Editor-in-Chief of GS over the past few years?
Dr. Thomsen: I have been fortunate to watch Gland Surgery grow to become an established resource and reference. I am proud to have been involved.
GS: As an Honorary Editor-in-Chief of GS, what are your expectations for GS?
Dr. Thomsen: I hope Gland Surgery can continue to grow towards an even higher impact.
