Ishith Seth1, Jin Ye Yeo2
1Department of Surgery, Peninsula Health, Victoria, Australia; 2GS Editorial Office, AME Publishing Company
Correspondence to: Jin Ye Yeo. GS Editorial Office, AME Publishing Company. Email: editor@glandsurgery.org
This interview can be cited as: Seth I, Yeo JY. Meeting the Editorial Board Member of GS: Dr. Ishith Seth. Gland Surg. 2024. https://gs.amegroups.org/post/view/meeting-the-editorial-board-member-of-gs-dr-ishith-seth.
Expert Introduction
Dr. Ishith Seth (Figure 1) is a Senior Resident in the Plastic Surgery Department at Peninsula Health in Victoria, Australia, and holds honorary senior researcher affiliations with Murdoch Children’s Research Institute, The Royal Children's Hospital, and The University of Melbourne. An accomplished educator, Dr. Seth serves as a Clinical Tutor and Adjunct Lecturer at Monash University.
Dr. Seth earned a Master of Surgery degree, during which he led groundbreaking research on the use of 3D-printed trapezium implants as a novel treatment for thumb-base arthritis. A prolific scholar, Dr. Seth has authored over 120 peer-reviewed publications, many focusing on the innovative use of Artificial Intelligence in surgical procedures and its potential integration into healthcare systems. As a recognized expert, he has been an invited speaker at over 50 national and international conferences, sharing insights into the future intersections of medicine and technology.
Dr. Seth is an active Editorial Board Member for several prestigious journals including the Journal of Clinical Medicine, AME Surgical Journal, Scientific Reports, Precision Surgery, and the Annals of Joint. He has also served as a guest editor for other medical journals like Lancet, Aesthetic Surgery Journal, and Plastic and Reconstructive Surgery, where his expertise is highly regarded. His multidisciplinary research interests, innovative surgical approaches, and significant contributions to medical literature establish Dr. Ishith Seth as a distinguished figure in the rapidly evolving fields of medical science and education.
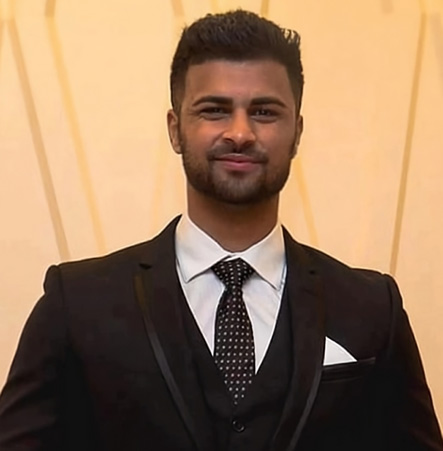
Figure 1 Dr. Ishith Seth
Interview
GS: What drove you into the field of surgery?
Dr. Seth: My journey into the field of surgery, specifically plastic and reconstructive surgery, is driven by a deep-seated passion for the complexities of human anatomy and a profound commitment to enhancing patient care through innovative medical practices. From my early academic pursuits to my current surgical training, each phase of my career has been carefully aligned with a singular focus: to excel in the surgical field and contribute significantly to its advancement.
It all started when I delved into laboratory-based research, particularly focusing on oncology, where I learned the critical aspects of scientific inquiry and experimental design. This exposure to the complexities of cellular mechanisms and disease processes ignited my interest in the intricacies of human biology, steering me towards a career in medicine. I pursued a Doctor of Medicine where my commitment to surgery began to take a definitive shape. The transformative experiences during my internships and subsequent residency at Peninsula Health were pivotal where I was drawn into the world of plastic and reconstructive surgery, a specialty that not only demands precision but also a deep understanding of aesthetics and function. Witnessing the profound impact of reconstructive surgery on restoring not only physical appearance but also functionality and psychological well-being of patients was deeply inspiring. These experiences solidified my resolve to specialize in this transformative field. My academic pursuits continued with a Master of Surgery, focusing on the cutting-edge area of 3D-printed implants for base of thumb arthritis and use of Artificial Intelligence in Surgery. This research was not just about enhancing my surgical skills; it represented the fusion of clinical practice with technological innovation, offering new solutions to complex surgical problems. It highlighted how surgical practice could evolve with advancements in technology, enhancing patient outcomes and surgical precision.
My dedication to surgical excellence is continually demonstrated through my ongoing educational endeavors. I have successfully completed numerous courses accredited by the College of Surgeons, as well as certifications from prestigious Ivy League institutions, arming me with a diverse and comprehensive set of surgical skills. These qualifications are far from just procedural necessities; they are indispensable tools that equip me to navigate the complex and varied challenges encountered in surgical settings. My aspiration to excel in surgery is deeply anchored in a solid academic foundation, augmented by practical clinical experience and a passionate commitment to medical innovation. Each phase of my career is strategically designed not only to refine my competencies as a surgeon but also to position me as a pioneer in the field, dedicated to pushing the boundaries of medical science and enhancing patient care. In pursuing this path, I am guided by the enduring words of Sushruta, the father of plastic and reconstructive surgery, who said: “A person who possesses courage and presence of mind, a hand free from perspiration, a tremorless grip of sharp and good instruments, and who carries his operations to the success and advantage of his patient who has entrusted his life to the surgeon, should treat his patient with the utmost respect and care, as if they were his own child.” This profound insight from Sushruta Samhita continues to inspire and steer my professional journey, reinforcing my commitment to uphold the highest standards of ethical and compassionate care in the practice of surgery.
GS: Since you have a solid research background on artificial intelligence in surgery, what do you think are some of the greatest benefits of using artificial intelligence for surgery?
Dr. Seth: My research background on artificial intelligence in surgery has given me a deep appreciation for the significant benefits that AI can bring to the field. My experiences and studies have highlighted how AI can transform surgical practices by enhancing precision, improving patient outcomes, and fostering innovation in surgical techniques. One of the most significant advantages of AI in surgery is its ability to augment surgical precision. For instance, in my research published in journals such as the Aesthetic Surgery Journal and Journal of Clinical Medicine, I explored how AI can assist in complex decision-making processes (1, 2, 3, 4, 5, 6).
AI algorithms can analyze vast amounts of data quickly, providing surgeons with real-time insights that are not immediately apparent through human analysis alone. This capability is particularly beneficial in preoperative planning, where AI can help determine the most effective surgical approach based on a patient’s unique anatomical and medical profile (7, 8). Moreover, AI's impact on patient outcomes cannot be overstated. In my publication "The Role of Artificial Intelligence Tools on Advancing Scientific Research,"(9) I discussed how AI technologies, such as predictive analytics, can forecast potential complications, enabling preemptive measures that significantly reduce patient risk. Additionally, AI-driven simulations and 3D modeling allow for better preparation and precision, which directly correlate with improved post-surgical results and quicker patient recovery times.
Another area where AI proves invaluable is in surgical education and training (10). The integration of AI into surgical training programs offers a dynamic, interactive learning environment. Trainees can engage with virtual and augmented reality simulations that mimic real-life surgeries, providing an invaluable tool for honing skills without the ethical concerns or risks associated with practicing on live patients. Finally, my ongoing research into AI's applications in plastic surgery underscores its potential to push the boundaries of the field (11, 12). AI's ability to integrate with existing medical technologies and innovate new ones paves the way for groundbreaking advancements in surgical techniques and materials. I believe AI represents a transformative force in surgery, its capacity to enhance surgical accuracy, optimize outcomes, revolutionize training, and drive forward the frontiers of surgical science illustrates the profound impact that intelligent technologies can have on the field.
GS: Would you like to give us a general picture of recent innovations in this area?
Dr. Seth: My involvement in the application of artificial intelligence in surgery has given me a unique vantage point from which to observe and engage with the cutting-edge innovations transforming this field. These advancements leverage AI's robust analytical capabilities to elevate surgical precision, optimize patient outcomes, and redefine surgical education. One of the most notable innovations in this space is the advancement of machine learning (ML) algorithms that enhance the diagnostic and predictive capabilities in surgical settings (11). For example, the integration of AI in surgical diagnostics has significantly improved the ability to identify and differentiate between subtypes of skin cancer through detailed image analysis. These AI systems employ deep learning algorithms to scrutinize dermatological images, achieving a level of precision and accuracy that surpasses even experienced dermatologists. This advanced diagnostic capability allows for earlier detection of skin cancer types, leading to more accurate and timely treatment plans and potentially better patient outcomes. This advancement highlights the growing importance of AI in enhancing diagnostic accuracy in surgical fields (13). Moreover, predictive analytics in AI are revolutionizing postoperative care. AI models are now capable of predicting potential complications with high accuracy, thereby enabling proactive medical interventions. This application is critical in high-stakes environments like cardiothoracic and vascular surgery, where AI tools may predict outcomes such as the likelihood of aneurysm rupture or postoperative recovery trajectories. By integrating patient-specific data, AI systems can tailor these predictions, significantly improving patient safety and reducing the rate of postoperative complications.
The role of AI in surgical training and education is also undergoing significant transformation. Through virtual reality (VR) and augmented reality (AR) platforms powered by AI, surgical trainees can experience immersive, realistic surgical simulations (14,15). These tools offer a hands-on learning experience without the risk associated with live procedures. AI enhances these simulations with real-time feedback and adaptive learning paths, which are tailored to the proficiency level and learning pace of individual trainees. Looking towards the future, the horizon of AI in surgery includes the development of more autonomous surgical robots. These systems are expected to handle routine surgical tasks autonomously, allowing surgeons to focus on more complex aspects of surgical procedures. The integration of AI with robotic surgery promises not only enhanced precision but also the potential for remote surgery, which could revolutionize medical care in underserved regions. In patient education, AI is set to play a transformative role by offering personalized, interactive tools that explain surgical risks, procedures, and expected outcomes in a user-friendly manner. This approach not only enhances patient understanding and consent processes but also aligns with the broader trend towards patient-centered healthcare.
GS: How have the innovations impacted you as a plastic surgeon? Can you share any examples or case studies where these innovations significantly improved your surgical procedures or research?
Dr. Seth: As a plastic surgery senior resident deeply engaged with the latest advancements in technology, I have had the invaluable opportunity to witness and utilize innovations such as Augmented Reality in enhancing surgical precision and outcomes (15). My experience with AR, particularly in the realm of breast reconstruction using the Deep Inferior Epigastric Perforator (DIEP) flap technique, has significantly shaped my approach to complex reconstructive surgeries. In a recent study I was involved in, we utilized AR headsets for the identification and visualization of perforator vessels during DIEP flap breast reconstructions. This technology allowed for a sophisticated overlay of a three-dimensional map directly onto the patient's surgical field, improving our ability to accurately identify and preserve vital vascular structures. The use of AR in this context not only enhanced the precision of perforator identification but also contributed to a decrease in operative times and an improvement in overall surgical outcomes. For example, in a series of cases documented in our research, the AR technology enabled us to precisely map out the course of perforators, which are crucial for the viability of the flap. This was particularly beneficial in a complex case where traditional imaging techniques had limitations. The AR system provided a dynamic and real-time view that traditional static images could not, allowing for adjustments during the surgery based on the most current anatomical presentation. This technology's impact extends beyond just operational assistance; it also offers substantial educational benefits. As a resident, using AR has deepened my understanding of anatomical structures and enhanced my ability to perform precise dissections and reconstructions. The immersive nature of AR helps bridge the gap between theoretical knowledge and practical application, a pivotal aspect of surgical training.
In my studies on the application of Artificial Intelligence using Large Language Models (LLMs) in surgery (3, 8, 9, 16, 17), I explored how these advanced technologies can revolutionize surgical education and preoperative management. The study particularly focused on the capabilities of LLMs to process and synthesize vast amounts of medical literature and patient data, providing real-time, evidence-based insights to surgeons. This AI-driven approach is poised to dramatically enhance the educational landscape by offering personalized learning experiences and simulating complex surgical scenarios that residents can interact with. For preoperative management, the integration of LLMs allows for more precise surgical planning by predicting potential complications and suggesting the best procedural strategies tailored to individual patient profiles. This not only improves the safety and efficiency of surgeries but also enhances patient outcomes by ensuring that each surgical approach is optimally planned with the support of comprehensive data analysis. Such innovations mark a significant step forward in the integration of AI in medicine, promising to transform traditional surgical training and planning with data-driven precision and intelligence.
GS: What inspired you to explore the use of 3D-printed trapezium implants as a novel treatment modality for thumb-base arthritis?
Dr. Seth: My inspiration to explore the use of 3D-printed trapezium implants for thumb-base arthritis stemmed from the prevalence and impact of trapeziometacarpal (base of thumb) osteoarthritis, which affects a significant portion of the population, particularly the elderly. This condition severely limits hand function, impacting daily activities and overall quality of life due to pain and loss of thumb mobility. The standard treatment options, while effective to a degree, often don't restore full function or entirely alleviate symptoms, prompting the need for more tailored and effective solutions. This gap led me to investigate the potential of 3D-printed implants, which offer a novel approach through customization to individual patient anatomy, potentially improving surgical outcomes significantly (18).
In my Masters, I detailed the process of designing and fabricating custom trapezium implants using 3D printing technology. This innovative approach enabled the creation of anatomically accurate models of the trapezium bone, the ability to customize each implant to the specific contours and requirements of individual patient anatomy allowed for unprecedented precision in fit and functionality. By practicing with models that closely mimic actual surgical scenarios, trainees could gain valuable experience in handling complex procedures, thereby enhancing their skills in a risk-free environment. Furthermore, my research explored the biomechanical compatibility of these implants with human tissue, focusing on minimizing the risk of rejection and optimizing integration with the surrounding bone structure. The use of biocompatible materials was crucial to ensure that the implants would be accepted by the body and function effectively over time. This groundbreaking work demonstrated potential reductions in post-operative complications, such as improper implant alignment and mobility issues, which are common with standard implants. The future of 3D printing in carpal bone surgery looks promising, with ongoing advancements likely to further enhance the precision of these techniques and expand their application in other areas of reconstructive surgery.
GS: In your research, what were some significant challenges of using artificial intelligence for surgery?
Dr. Seth: In my research exploring the integration of artificial intelligence technologies like Machine Learning (ML), Deep Learning (DL), and Augmented Reality (AR) into surgical practice, I encountered several significant challenges that underscore the complexities of applying AI in clinical settings.
Firstly, one major challenge lies in the referencing outputs of Large Language Models. While these models are adept at processing and synthesizing large volumes of information, discrepancies in their referencing outputs can arise. These inaccuracies are often due to the LLMs' reliance on the data they were trained on, which may not always be updated or peer-reviewed. Such discrepancies can lead to potential misinformation, which is particularly critical in high-stakes environments like surgery where precision and accuracy are paramount. Another challenge is the inherent inaccuracies in machine learning and deep learning models. Despite their advanced capabilities, these AI systems can sometimes generate errors in pattern recognition and predictive analytics. For instance, in surgical applications, these inaccuracies might manifest in the misinterpretation of diagnostic imaging or mispredictions of surgical outcomes, which could adversely affect patient care. Ensuring the reliability of AI predictions is crucial, requiring ongoing training of the models with high-quality, diverse datasets to improve their accuracy and robustness.
Lastly, the practical application of augmented reality in surgery, while promising, faces significant hurdles. In my experience, using AR glasses in an operative environment proved challenging due to issues such as limited field of view, image instability, and the interference of ambient light affecting the visibility of AR projections. These technical limitations can hinder the effective use of AR for precision tasks such as guiding surgical interventions or training surgical residents.
GS: Do you think these challenges can be overcome by human intelligence, or would it require artificial intelligence as well?
Dr. Seth: I believe that the challenges associated with integrating artificial intelligence into surgical practices require a synergistic approach that leverages both human intelligence and further advancements in AI. Human intelligence plays a crucial role in overseeing AI operations, particularly in interpreting and verifying AI-generated data and making critical clinical decisions. Surgeons and healthcare professionals bring indispensable clinical insights, ethical considerations, and experiential knowledge that AI currently cannot replicate.
For instance, discrepancies in LLM outputs and inaccuracies in ML/DL predictions can be mitigated by clinicians who can interpret AI suggestions within the broader context of individual patient histories and clinical nuances. Additionally, human oversight ensures that AI tools adhere to ethical standards and remain aligned with patient-centric care. However, overcoming some technical challenges, such as the operational limitations of AR in surgical settings, would benefit significantly from advancements in AI and related technologies. Improvements in AR interface design, image stability, and integration with real-time surgical environments require technological innovation that goes beyond what human intelligence can compensate for on its own.
Thus, while human expertise is indispensable for contextualizing and guiding AI applications in surgery, the evolution and integration of AI tools themselves are crucial for addressing the technical limitations currently faced. This dual approach will harness the strengths of both human and artificial intelligence to advance surgical practices safely and effectively.
GS: How has your experience been as an Editorial Board Member of GS?
Dr. Seth: Serving as an Editorial Board Member for GS has been a profoundly enriching experience that aligns closely with my professional aims and the journal's goals. My involvement has offered me the opportunity to contribute to and shape the discourse around cutting-edge findings in the diagnosis, prevention, and treatment of gland diseases specifically in the breast, head, and neck. My work, particularly in the realms of advanced diagnostics and surgical interventions, dovetails with the journal’s commitment to disseminating practical information and transformative research. The interdisciplinary nature of GS, which encompasses fields such as biomarkers, imaging, pathology, and interventional radiology, complements my own focus on integrating innovative technologies like artificial intelligence and 3D printing into surgical practice. This integration is crucial for enhancing diagnostic accuracy and surgical outcomes, which are core aspects of the journal's scope.
Moreover, the opportunity to review and contribute to articles that address both basic and clinical research aspects of gland diseases has allowed me to stay at the forefront of emerging trends and breakthroughs in glandular surgery. It also enables me to apply these insights to improve patient care protocols and outcomes in my own practice. Overall, my role as an Editorial Board Member has not only been a platform for contributing to the scientific community but also a significant avenue for professional growth and learning. It has been rewarding to help advance our understanding and treatment of gland diseases through such a respected multidisciplinary periodical.
GS: As an Editorial Board Member of GS, what are your expectations for GS?
Dr. Seth: As an Editorial Board Member of GS, my expectations for the journal are centered around its continued growth as a leading forum for innovative and impactful research in gland diseases. I anticipate that GS will further its reputation by consistently publishing high-quality, peer-reviewed articles that not only advance the scientific understanding of gland-related conditions but also significantly influence clinical practices globally. I expect that GS will expand its multidisciplinary approach, drawing contributions from an even broader array of fields such as molecular biology, genetics, and advanced imaging techniques. This will enrich the journal's content and provide a more holistic view of gland diseases, facilitating comprehensive approaches to diagnosis, treatment, and prevention. Additionally, I look forward to seeing GS enhance its digital presence and accessibility, making research findings available and digestible to a wider audience, including clinicians, researchers, and even patients seeking the latest information on glandular diseases.
Reference
- Seth I, Bulloch G, Joseph K, et al. Use of artificial intelligence in the advancement of breast surgery and implications for breast reconstruction: a narrative review. Journal of Clinical Medicine. 2023;12(15):5143.
- Xie Y, Seth I, Rozen WM, et al. Evaluation of the artificial intelligence chatbot on breast reconstruction and its efficacy in surgical research: a case study. Aesthetic Plastic Surgery. 2023;47(6):2360-9.
- Seth I, Bulloch G, Rozen WM. Applications of artificial intelligence and large language models to plastic surgery research. Aesthetic Surgery Journal. 2023;43(10):NP809-NP10.
- Xie Y, Seth I, Hunter-Smith DJ, et al. Aesthetic surgery advice and counseling from artificial intelligence: a rhinoplasty consultation with ChatGPT. Aesthetic Plastic Surgery. 2023;47(5):1985-93.
- Seth I, Kenney PS, Bulloch G, et al. Artificial or augmented authorship? A conversation with a chatbot on base of thumb arthritis. Plastic and Reconstructive Surgery–Global Open. 2023;11(5):e4999.
- Lim B, Seth I, Bulloch G, et al. Evaluating the efficacy of major language models in providing guidance for hand trauma nerve laceration patients: a case study on Google’s AI BARD, Bing AI, and ChatGPT. Plast Aesthet Res. 2023;10:43.
- Cevik J, Seth I, Rozen WM. Transforming breast reconstruction: the pioneering role of artificial intelligence in preoperative planning. Gland Surgery. 2023;12(9):1271.
- Atkinson CJ, Seth I, Xie Y, et al. Artificial Intelligence Language Model Performance for Rapid Intraoperative Queries in Plastic Surgery: ChatGPT and the Deep Inferior Epigastric Perforator Flap. Journal of Clinical Medicine. 2024;13(3):900.
- Lim B, Seth I, Rozen WM. The Role of Artificial Intelligence Tools on Advancing Scientific Research. Aesthetic Plastic Surgery. 2023:1-3.
- Xie Y, Seth I, Hunter‐Smith DJ, et al. Investigating the impact of innovative AI chatbot on post‐pandemic medical education and clinical assistance: a comprehensive analysis. ANZ Journal of Surgery. 2024;94(1-2):68-77.
- Seth I, Lim B, Joseph K, et al. Use of artificial intelligence in breast surgery: a narrative review. Gland Surgery. 2024;13(3):395.
- Lim B, Seth I, Xie Y, et al. Exploring the Unknown: Evaluating ChatGPT's Performance in Uncovering Novel Aspects of Plastic Surgery and Identifying Areas for Future Innovation. Aesthetic Plastic Surgery. 2024:1-10.
- Strzelecki M, Kociołek M, Strąkowska M, et al. Artificial Intelligence in the detection of skin cancer: state of the art. Clinics in Dermatology. 2024.
- Lim B, Cevik J, Seth I, et al. Evaluating Artificial Intelligence's Role in Teaching the Reporting and Interpretation of Computed Tomographic Angiography for Preoperative Planning of the Deep Inferior Epigastric Artery Perforator Flap. JPRAS Open. 2024.
- Seth I, Lindhardt J, Jakobsen A, et al. Improving Visualization of Intramuscular Perforator Course: Augmented Reality Headsets for DIEP Flap Breast Reconstruction. Plast Reconstr Surg Glob Open. 2023;11(9):e5282.
- Mu X, Lim B, Seth I, et al. Comparison of large language models in management advice for melanoma: Google's AI BARD, BingAI and ChatGPT. Skin Health and Disease. 2024;4(1):e313.
- Sathe A, Seth I, Bulloch G, et al. The role of artificial intelligence language models in dermatology: opportunities, limitations and ethical considerations. Australasian Journal of Dermatology. 2023;64(4):548-52.
- Seth I, Bulloch G, Seth N, et al. Use of Three-dimensional Printed Carpal Bones for Various Carpal Pathologies: A Systematic Review. The Open Orthopaedics Journal. 2023;17(1).
