
Preoperative dexamethasone administration in reducing the incidence of nausea and vomiting after thyroidectomy: a systematic review and meta-analysis of drug dosage
Highlight box
Key findings
• The study found that a preoperative single dose of 8–10 mg of dexamethasone significantly reduces postoperative nausea and vomiting (PONV) and the need for additional antiemetic medications while additionally alleviating postoperative pain after thyroidectomy.
What is known and what is new?
• Dexamethasone has a positive impact on PONV and pain.
• The meta-analysis confirmed a specific dosage range of 8–10 mg for dexamethasone as an effective preoperative treatment.
What is the implication, and what should change now?
• Healthcare providers should consider using 8–10 mg of dexamethasone preoperatively to reduce PONV and pain in patients undergoing thyroidectomy.
• There is need for further randomized controlled trials to investigate the effects of varied dosages (e.g., 4–5 mg) of dexamethasone on postoperative pain, which could potentially refine treatment protocols.
IntroductionOther Section
Thyroid cancer, as one of the most common endocrine diseases affecting the thyroid gland, has been a global healthcare concern over recent years. Although the incidence of thyroid cancer varies according to region and period, interest in this disease has remained relatively high (1-3). In the United States, thyroid cancer has become more prevalent in both men and women, with rates rising from 4.9 cases per 100,000 in 1975 to 14.3 cases per 100,000 in 2014 (4). Surgical resection is the most common treatment for this type of cancer, but patients frequently experience postoperative nausea and vomiting (PONV), which are unavoidable sequelae of the procedure (5,6). Additionally, patients may experience other significant postoperative problems that adversely affect their comfort (7).
Numerous types of medication have been applied to prevent PONV before thyroid cancer surgery, such as 5-HT3 receptor antagonists, droperidol, and metoclopramide (8). However, these all share common side effects, including headaches, constipation, elevated liver enzyme levels, restlessness, anxiety, and irregular heartbeat, among others (9-11). Studies have suggested that dexamethasone, a cost-effective medication with minimal side effects, may be beneficial for reducing PONV (12-14). However, the effectiveness of dexamethasone in alleviating PONV and pain in patients undergoing thyroidectomy remains controversial (15-17). Chen et al.’s review indicated that dexamethasone can significantly decrease the incidence of PONV, 24-hour visual analog pain scores (VAS), and analgesic use (18). Additionally, Li et al. reviewed seven relevant studies and reported that a single preoperative application of dexamethasone can reduce the incidence and severity of PONV in patients undergoing thyroidectomy, but it may not have an effect on pain or analgesic consumption (19). De Oliveira et al. found that using a dose of 8–10 mg of dexamethasone did not have any clinical advantage over a dose of 4–5 mg in reducing the incidence of PONV (20). However, a study conducted by Barros et al. found that a single low dose of 4 mg of dexamethasone had limited effects on postoperative pain and tramadol demand after thyroidectomy (21). Another meta-analysis has affirmed the safety and efficacy of intravenously administering prophylactic dexamethasone (8–10 mg) before anesthesia induction (22).
We conducted meta-analysis to offer a more precise and comprehensive understanding of the benefits of dexamethasone usage in clinical practice. The findings may be useful for clinicians who are considering the use of dexamethasone for reducing the incidence of PONV and improving pain relief in their patients. We present this article in accordance with the PRISMA reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-23-260/rc).
MethodsOther Section
Search strategies
The PubMed, Web of Science, EMBASE, and Cochrane Library databased were searched for randomized controlled trials (RCTs) conducted prior to December 30, 2022, in both the English and Chinese languages, and a similar search for unpublished data was also performed. The retrieval strategy was determined based on a combination of subject words and free words, which was adjusted according to the specific database. English database search terms included “dexamethasone”, “thyroidectomy”, “surgery”, “randomized controlled trial”, and “random”. The optimal combination of the above phrases was applied to search for relevant articles.
Inclusion and exclusion criteria
Inclusion criteria
The inclusion criteria for the trials were as follows: (I) RCTs, (II) enrollment of patients undergoing thyroidectomy without any other surgical intervention, (III) absence of any prior intake of analgesic or antiemetic medications by patients before the operation, and (IV) administration of intravenous dexamethasone to the experimental group and 0.9% normal saline placebo to the control group.
Exclusion criteria
The following material was excluded from the analysis: (I) duplicate trials; (II) studies with an imprecise definition of the evaluation index for research outcomes that could have led to classification errors; (III) studies that did not include original data in their findings; and (IV) literature such as case studies, case analyses, reviews, and other types of nonoriginal research.
Literature quality evaluation and data
Two independent reviewers conducted literature screening and data extraction for the meta-analysis. This involved collecting information related to the title, author, basic data of the research participants, sample size, outcome indicators, research results, and other relevant data. In cases where there was disagreement about the literature’s inclusion, the researchers discussed the study and sought the input of a third reviewer before making a final decision. Additionally, each researcher individually assessed the quality of the included literature using the Jadad Scale, a tool designed to evaluate RCTs.
Statistical analysis
A meta-analysis was conducted using RevMan 5.3 software (Cochrane). The mean difference (MD) was calculated for continuous data, the odds ratio (OR) was calculated for binary data, and the Cochrane Q test was used to assess heterogeneity between studies. The 95% confidence interval (CI) was calculated for all analyses. If studies were statistically heterogeneous (P>0.01 and I2<50%), a fixed-effects model was used. If studies were heterogeneous (P<0.01 and I2≥50%), but there was no clinical heterogeneity in the results, a random-effects model was used. If the source of heterogeneity could not be determined, a descriptive analysis was performed. TSA v. 0.9.5.10 Beta software (Copenhagen Clinical Trial Center), was used to perform trial sequential analysis (TSA) on the main outcome indicators to assess the accuracy of the evidence. The TSA-adjusted target sample size is referred to as the “expected sample size”, which is determined based on detecting a predetermined clinically meaningful effect. The traditional significance level (ɑ=0.05) was used to construct the TSA monitoring boundary and calculate the Z statistic for each trial. A cumulative Z curve was then constructed based on the included studies.
ResultsOther Section
Basic information of the included literature
After searches were conducted up to December 30, 2022, a total of 337 articles were identified. After the titles and abstracts were screened, 163 articles were identified as potentially eligible for inclusion. We retrieved the full-text articles and analyzed them, with 11 RCTs ultimately being deemed eligible (11,21,23-31) (Figure 1).
Basic features of the included literature
A total of 1,544 participants who had undergone thyroid surgery were finally included among the 11 eligible RCTs conducted in the following countries: Italy, Japan, Switzerland, China, Korea, and Portugal. Among these studies, ten reported on the effectiveness of dexamethasone in preventing PONV in patients undergoing thyroidectomy while nine reported on its pain-relief effects. Ten trials scored 5 or higher on the Jadad scale. More basic characteristics of the included literature are presented in Table 1.
Table 1
| First author | Journal | Country/region | Experimental | Control | Result (effective) | Jadad score |
|---|---|---|---|---|---|---|
| Ahmad, R (23) | Cureus | Pakistan | Dexamethasone 8 mg/2 mL | Saline (0.9%) | PONV and pain | 4 |
| Lee, Y (24) | Acta anaesthesiologica Sinica | Taipei | Dexamethasone 5 mg/8 mg | Saline (0.9%) | PONV and pain | 5 |
| Worni, M (25) | Annals of Surgery | Switzerland | Dexamethasone 8 mg/2 mL | Saline (0.9%) | PONV and pain | 7 |
| Doksrod, S (26) | Acta Anaesthesiologica Scandinavica | Norway | Dexamethasone 0.15 mg/kg | Saline (0.9%) 2 mL | PONV and pain | 6 |
| Feroci, F (27) | Head & Neck | Italy | Dexamethasone 8 mg/2 mL | Saline (0.9%) 10 mL | PONV and pain | 7 |
| Fujii, Y (28) | Otolaryngology–Head and Neck Surgery | Japan | Dexamethasone 4 mg/8 mg | Placebo | PONV | 5 |
| Tarantino, I (29) | Annals of Surgery | Switzerland | Dexamethasone 8 mg/2 mL | Placebo | PONV | 5 |
| Wang, JJ (11) | Anesthesia & Analgesia | Taipei | Dexamethasone 10 mg/2 mL | Saline (0.9%) 2 mL | PONV and pain | 5 |
| Chen, W (30) | Journal of the American College of Surgeons | China | Dexamethasone 10 mg/2 mL | Saline (0.9%) 2 mL | PONV and pain | 7 |
| Barros, A (21) | Pharmacology | Portugal | Dexamethasone 4 mg/2 mL | Saline (0.9%) 2 mL | PONV and pain | 5 |
| Song, YK (31) | Journal of Anesthesia | Korea | Dexamethasone 4 mg/2 mL | Saline (0.9%) 2 mL | PONV and pain | 6 |
PONV, postoperative nausea and vomiting.
Meta-analysis results on the efficacy of dexamethasone in preventing PONV
A total of 1,475 patients were included in the meta-analysis, and 772 cases were placed in a dexamethasone treatment group and 703 cases in a placebo group. The analysis showed significant heterogeneity among studies. Specifically, ten studies indicated that dexamethasone at a dose of 8–10 mg significantly reduced the 24-hour incidence of PONV (OR: 0.27; 95% CI: 0.15–0.50; I2=82%; P<0.0001), as depicted in Figure 2. However, in a subgroup analysis of two studies, dexamethasone at a dose of 4–5 mg did not significantly reduce PONV incidence (OR 0.22; 95% CI: 0.03–1.33; I2=80%; P=0.1).
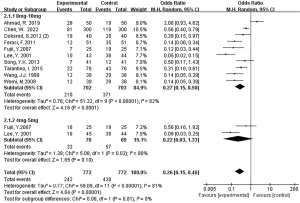
Further analyses revealed that dexamethasone at a dose of 8–10 mg had a significantly greater effect in reducing the incidence of PONV than did dexamethasone at a dose of 4–5 mg (OR 0.39; 95% CI: 0.19–0.80; I2=29%; P=0.01), as illustrated in Figure 3. Additionally, three studies reported antiemetic usage, and dexamethasone was found to be significantly effective in reducing the use of rescue antiemetics compared to placebo (OR 0.59; 95% CI: 0.38–0.92; I2=25%; P=0.02), as shown in Figure 4.

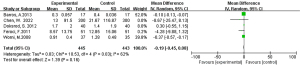
Efficacy of dexamethasone’s in postoperative pain management
The meta-analysis included a total of 722 patients with postoperative pain, with 362 being placed in the dexamethasone treatment group and 360 in a placebo group. The results indicated that administering dexamethasone at a dosage of 8–10 mg can significantly reduce pain VAS score in patients undergoing thyroidectomy (MD: –1.19; 95% CI: –1.97 to –0.41; I2=96%; P=0.003). However, subgroup analysis for a dosage of 4–5 mg did not demonstrate a significant reduction in pain score (MD: –0.27; 95% CI: –1.00 to 0.45; I2=0%; P=0.46) (Figure 5).

The consumption of analgesics was reported in five studies, but it did not show a significant effect on postoperative pain in the dexamethasone group (MD: –0.19, 95% CI: –0.45 to 0.08; I2=62%; P=0.16) (Figure 6).
Sensitivity analysis and publication bias
Regarding the analysis on sensitivity and publication bias, we observed asymmetry in the funnel plot (Figure 7), indicating potential publication bias in assessing the treatment effectiveness for PONV. To further evaluate this, we conducted TSA with α and β error thresholds set at 0.05 and 0.2, respectively, to assess the adequacy of the sample size for evaluating the effect of the intervention. Our TSA analysis showed that the cumulative Z curve crossed both the traditional and the monitoring boundaries at each time point, indicating that the available evidence was sufficient to establish the intervention effect of dexamethasone in preventing PONV. Additionally, TSA analysis indicated that the required sample size was 544 cases, and the cumulative Z curve did exceed the expected sample size (Figure 8).
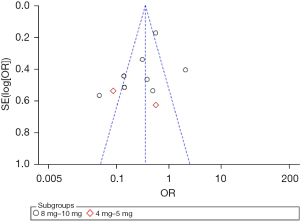

The points indicating the effectiveness of treatments for pain in the funnel plot suggested the presence of publication bias (Figure S1). In our TSA analysis, the cumulative Z curve crossed the traditional boundary, but did not cross the monitoring boundary and thus did not exceed the expected sample size (Figure S2).
DiscussionOther Section
PONV are the most common postoperative complications, and early prevention and treatment are crucial for avoiding complications, improving patient satisfaction, and accelerating recovery (32,33). Studies have shown that PONV rates in patients undergoing thyroidectomy exceed 80% (34). Lee et al. conducted a RCT and found that administering 8 mg of dexamethasone was more effective than was 5 mg for relieving PONV in female patients after surgery for thyroid cancer (24). In a recent systematic review, Li et al. concluded that while dexamethasone can reduce the severity of PONV in patients undergoing thyroidectomy, it does not improve patients’ postoperative pain (19). However, research by Ahmad et al. showed that prophylactic use of dexamethasone can significantly reduce pain in patients undergoing thyroidectomy but did not find a statistically significant correlation with PONV (23). Inconsistency in drug dosage and inconsistent effects on pain make it challenging to provide consistent clinical and nursing care guidance. To address this confusion, the meta-analysis was conducted in which 8 to 10-mg and 4 to 5-mg doses of dexamethasone were used as grouping criteria. The aim of this study was to standardize the preoperative dexamethasone dosage for improved prevention of PONV and pain in patients undergoing surgery for thyroid cancer. A random-effects model was employed to assess the effectiveness of dexamethasone in reducing the incidence of PONV with preoperative doses. The results indicated that dexamethasone at 8–10 mg was effective in reducing PONV, which is consistent with Li et al.’s study (19).
The American Society of Anesthesiologists recommends the use of multimodal methods to manage acute pain after surgery, including drugs with various mechanisms of action such as α2 agonists, N-methyl-D-aspartate (NMDA) receptor antagonists, nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and duloxetine (35). Dexamethasone, a corticosteroid, has not been extensively discussed in the scientific literature in relation to its potential to introduce complications in microvascular reconstruction surgeries for patients with head and neck cancer (36). Nevertheless, it is worth highlighting that numerous studies offer substantial evidence supporting its effectiveness in effectively alleviating postoperative pain and reducing overall opioid consumption. For example, it has played a pivotal role in expediting the recovery process following total knee arthroplasty (37). Postthyroidectomy pain may result from several factors, including pain at the surgical site incisions, extensive neck manipulation, general anesthesia during intubation, and throat discomfort (38). Studies conducted by Worni et al. and Feroci et al. indicated that the preoperative use of dexamethasone may effectively reduce postoperative vomiting and pain in patients undergoing thyroid surgery (25,27). However, a systematic review found that it may not affect the pain level or analgesic consumption, while a single preoperative application of dexamethasone can reduce the incidence and severity of PONV after thyroidectomy (19). Our meta-analysis showed that administering dexamethasone at a dosage of 8–10 mg can significantly reduce pain in patients undergoing thyroidectomy. It is worth noting that of the 11 studies, only Tarantino et al.’s study reported that anesthesia combined with a cervical plexus block resulted in a decrease in pain scores, with no differences in postoperative pain observed between the dexamethasone treatment group and the control group (29). Furthermore, this study was not included in our pain analysis, so the analysis results of dexamethasone for pain relief were not affected.
After conducting sequential TSA tests, we believe that there is no need to conduct further trials to clarify the effect of dexamethasone in relieving PONV. However, based on the above analysis, the funnel plot on the effectiveness of treatments for pain suggested the presence of publication bias. Therefore, we can also conclude that the available evidence on the preoperative administration of dexamethasone for pain relief in patients undergoing thyroidectomy is not sufficient.
ConclusionsOther Section
Based on the available evidence, it appears that a single preoperative dose of 8–10 mg of dexamethasone can be effective in reducing the incidence of PONV and pain in patients undergoing thyroidectomy. However, further research is needed to fully understand the effects of dexamethasone on pain relief after thyroidectomy. Large-scale RCTs would be particularly valuable in investigating the potential benefits and drawbacks of this treatment approach.
AcknowledgmentsOther Section
Funding: None.
FootnoteOther Section
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-23-260/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-260/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-23-260/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Cronin KA, Scott S, Firth AU, et al. Annual report to the nation on the status of cancer, part 1: National cancer statistics. Cancer 2022;128:4251-84. [Crossref] [PubMed]
- Nakata K, Matsuda T, Hori M, et al. Cancer incidence and type of treatment hospital among children, adolescents, and young adults in Japan, 2016-2018. Cancer Sci 2023;114:3770-82. [Crossref] [PubMed]
- Lin Y, Wu Y. Trends in incidence and overdiagnosis of thyroid cancer in China, Japan, and South Korea. Cancer Sci 2023;114:4052-62. [Crossref] [PubMed]
- Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg 2014;140:317-22. [Crossref] [PubMed]
- Gauger PG, Shanks A, Morris M, et al. Propofol decreases early postoperative nausea and vomiting in patients undergoing thyroid and parathyroid operations. World J Surg 2008;32:1525-34. [Crossref] [PubMed]
- Kim MK, Yi MS, Kang H, et al. Effects of remifentanil versus nitrous oxide on postoperative nausea, vomiting, and pain in patients receiving thyroidectomy: Propensity score matching analysis. Medicine (Baltimore) 2016;95:e5135. [Crossref] [PubMed]
- Papaleontiou M, Hughes DT, Guo C, et al. Population-Based Assessment of Complications Following Surgery for Thyroid Cancer. J Clin Endocrinol Metab 2017;102:2543-51. [Crossref] [PubMed]
- Gan TJ, Belani KG, Bergese S, et al. Fourth Consensus Guidelines for the Management of Postoperative Nausea and Vomiting. Anesth Analg 2020;131:411-48. [Crossref] [PubMed]
- Habib AS, Gan TJ. Food and drug administration black box warning on the perioperative use of droperidol: a review of the cases. Anesth Analg 2003;96:1377-9. [Crossref] [PubMed]
- Egerton-Warburton D, Povey K. Administration of metoclopramide by infusion or bolus does not affect the incidence of drug-induced akathisia. Emerg Med Australas 2013;25:207-12.
- Wang JJ, Ho ST, Lee SC, et al. The use of dexamethasone for preventing postoperative nausea and vomiting in females undergoing thyroidectomy: a dose-ranging study. Anesth Analg 2000;91:1404-7. [Crossref] [PubMed]
- Shilpa SN, Shailaja S, Hilda SS. Comparison of Efficacy of Clonidine versus Ondansetron for Prevention of Nausea and Vomiting Post Thyroidectomy: A Double Blind Randomized Controlled Trial. J Clin Diagn Res 2015;9:UC01-3. [Crossref] [PubMed]
- Mutlu V, Ince I. Preemptive intravenous ibuprofen application reduces pain and opioid consumption following thyroid surgery. Am J Otolaryngol 2019;40:70-3. [Crossref] [PubMed]
- Sellami M, Feki S, Triki Z, et al. Bupivacaine wound infiltration reduces postoperative pain and analgesic requirement after thyroid surgery. Eur Arch Otorhinolaryngol 2018;275:1265-70. [Crossref] [PubMed]
- Jeon Y, Kim H, Kwak KH. Comparison of ramosetron, dexamethasone, and a combination of ramosetron and dexamethasone for the prevention of postoperative nausea and vomiting in Korean women undergoing thyroidectomy: A double-blind, randomized, controlled study. Curr Ther Res Clin Exp 2010;71:78-88. [Crossref] [PubMed]
- Golder AM, McSorley ST, Kearns RJ, et al. Attitudes towards the use of perioperative steroids in resectional colorectal cancer surgery in the UK: A qualitative study. Ann Med Surg (Lond) 2019;48:23-8. [Crossref] [PubMed]
- Lee Y, Lai HY, Lin PC, et al. A dose ranging study of dexamethasone for preventing patient-controlled analgesia-related nausea and vomiting: a comparison of droperidol with saline. Anesth Analg 2004;98:1066-71. [Crossref] [PubMed]
- Chen CC, Siddiqui FJ, Chen TL, et al. Dexamethasone for prevention of postoperative nausea and vomiting in patients undergoing thyroidectomy: meta-analysis of randomized controlled trials. World J Surg 2012;36:61-8. [Crossref] [PubMed]
- Li B, Wang H. Dexamethasone reduces nausea and vomiting but not pain after thyroid surgery: a meta-analysis of randomized controlled trials. Med Sci Monit 2014;20:2837-45. [Crossref] [PubMed]
- De Oliveira GS Jr, Castro-Alves LJ, Ahmad S, et al. Dexamethasone to prevent postoperative nausea and vomiting: an updated meta-analysis of randomized controlled trials. Anesth Analg 2013;116:58-74. [Crossref] [PubMed]
- Barros A, Vale CP, Oliveira FC, et al. Dexamethasone effect on postoperative pain and tramadol requirement after thyroidectomy. Pharmacology 2013;91:153-7. [Crossref] [PubMed]
- Zou Z, Jiang Y, Xiao M, et al. The impact of prophylactic dexamethasone on nausea and vomiting after thyroidectomy: a systematic review and meta-analysis. PLoS One 2014;9:e109582. [Crossref] [PubMed]
- Ahmad R, Changeez M, Tameez Ud Din A, et al. Role of Prophylactic Dexamethasone Before Thyroidectomy in Reducing Postoperative Pain, Nausea and Vomiting. Cureus 2019;11:e4735. [Crossref] [PubMed]
- Lee Y, Lin PC, Lai HY, et al. Prevention of PONV with dexamethasone in female patients undergoing desflurane anesthesia for thyroidectomy. Acta Anaesthesiol Sin 2001;39:151-6.
- Worni M, Schudel HH, Seifert E, et al. Randomized controlled trial on single dose steroid before thyroidectomy for benign disease to improve postoperative nausea, pain, and vocal function. Ann Surg 2008;248:1060-6. [Crossref] [PubMed]
- Doksrød S, Sagen Ø, Nøstdahl T, et al. Dexamethasone does not reduce pain or analgesic consumption after thyroid surgery; a prospective, randomized trial. Acta Anaesthesiol Scand 2012;56:513-9. [Crossref] [PubMed]
- Feroci F, Rettori M, Borrelli A, et al. Dexamethasone prophylaxis before thyroidectomy to reduce postoperative nausea, pain, and vocal dysfunction: a randomized clinical controlled trial. Head Neck 2011;33:840-6. [Crossref] [PubMed]
- Fujii Y, Nakayama M. Efficacy of dexamethasone for reducing postoperative nausea and vomiting and analgesic requirements after thyroidectomy. Otolaryngol Head Neck Surg 2007;136:274-7. [Crossref] [PubMed]
- Tarantino I, Warschkow R, Beutner U, et al. Efficacy of a Single Preoperative Dexamethasone Dose to Prevent Nausea and Vomiting After Thyroidectomy (the tPONV Study): A Randomized, Double-blind, Placebo-controlled Clinical Trial. Ann Surg 2015;262:934-40. [Crossref] [PubMed]
- Chen W, Li G, Jiang K, et al. Dexamethasone for Postoperative Nausea and Vomiting in Papillary Thyroid Carcinoma Patients: A Randomized Clinical Trial. J Am Coll Surg 2022;235:454-67. [Crossref] [PubMed]
- Song YK, Lee C. Effects of ramosetron and dexamethasone on postoperative nausea, vomiting, pain, and shivering in female patients undergoing thyroid surgery. J Anesth 2013;27:29-34. [Crossref] [PubMed]
- Veiga-Gil L, Pueyo J, López-Olaondo L. Postoperative nausea and vomiting: physiopathology, risk factors, prophylaxis and treatment. Rev Esp Anestesiol Reanim 2017;64:223-32. [Crossref] [PubMed]
- Finch C, Parkosewich JA, Perrone D, et al. Incidence, Timing, and Factors Associated with Postoperative Nausea and Vomiting in the Ambulatory Surgery Setting. J Perianesth Nurs 2019;34:1146-55. [Crossref] [PubMed]
- Sonner JM, Hynson JM, Clark O, et al. Nausea and vomiting following thyroid and parathyroid surgery. J Clin Anesth 1997;9:398-402. [Crossref] [PubMed]
- Helander EM, Menard BL, Harmon CM, et al. Multimodal Analgesia, Current Concepts, and Acute Pain Considerations. Curr Pain Headache Rep 2017;21:3. [Crossref] [PubMed]
- Kainulainen S, Törnwall J, Koivusalo AM, et al. Dexamethasone in head and neck cancer patients with microvascular reconstruction: No benefit, more complications. Oral Oncol 2017;65:45-50. [Crossref] [PubMed]
- Fan Z, Ma J, Kuang M, et al. The efficacy of dexamethasone reducing postoperative pain and emesis after total knee arthroplasty: A systematic review and meta-analysis. Int J Surg 2018;52:149-55. [Crossref] [PubMed]
- Kim MH, Kim MS, Lee JH, et al. Intravenously Administered Lidocaine and Magnesium During Thyroid Surgery in Female Patients for Better Quality of Recovery After Anesthesia. Anesth Analg 2018;127:635-41.
(English Language Editor: J. Gray)





