
Transoral endoscopic vestibular approach Sistrunk procedure (TEVAS)—case report and scoping review
Highlight box
Key findings
• Transoral endoscopic vestibular approach Sistrunk procedure (TEVAS) is an alternative technique to treat a thyroglossal duct cyst (TGDC) in selected patients who are motivated to avoid a visible neck scar.
• Robust studies regarding the safety profile and long-term follow-up are not available, therefore case selection should be performed carefully. The most important aspects that should be considered before performing this novel approach are patient motivation, cyst volume, previous infection of the TGDC, current or previous cyst fistulization, previous neck radiotherapy and suspicion for malignancy.
What was recommended and what is new?
• Before TEVAS, only the traditional open approach was recommended to treat TGDC.
• After the popularization of transoral neck surgery, the open Sistrunk technique was adapted to the endoscopic approach, making it possible to remove the TGDC attached to the hyoid bone body and its tract without a visible neck scar.
What is the implication, and what should change now?
• This novel approach has shown good results with an evident cosmetic improvement, leaving hidden scars inside the oral cavity.
• This review should lead to wider adoption and standardization of the technique.
• As this novel approach provides improved visualization with endoscopic image magnification, other technical benefits besides cosmesis may become evident with larger series.
• More studies are needed to confirm the safety profile as well as long-term outcomes such as recurrence rate.
Introduction
Background
The thyroglossal duct cyst (TGDC) is a congenital malformation that develops by the persistence of the thyroglossal duct, an embryonic tract whose function is to permit the migration of the thyroid gland from its origin on the base of the tongue to the lower central neck. As a congenital malformation, it presents in childhood in more than 90% of cases. The most common clinical manifestation is a central lump in the upper anterior neck at the level of the hyoid bone that moves with deglutination and swallowing (1,2). A smaller number of cases present themselves in adulthood. The differential diagnosis of adults presenting with a central neck mass includes dermoid cyst, epidermoid cyst, lipoma, lymphadenopathy and goiter. Imaging with ultrasound, computed tomography (CT) scan or magnetic resonance imaging (MRI) can confirm the diagnosis (2-6).
The definitive treatment of TGDC is surgical removal, and the gold standard technique is the Sistrunk procedure (1,5,6). Before this technique, TGDC was a challenging diagnosis to treat. At that time, a simple excision was the only proposed treatment and the recurrence rates were around 40% due to the friability of the portion of the thyroglossal duct above the hyoid bone (5,6). Sistrunk published the description of his technique in 1920 (1), which involves the complete excision of the TGDC attached to the central portion of the hyoid bone through a conventional transverse cervicotomy, avoiding the isolation of the friable portion of the duct. After the widespread adoption of this technique, recurrence rates decreased to less than 3% (7).
Rationale and knowledge gap
While the Sistrunk procedure was revolutionary in the treatment of TGDC, the technique has not changed or evolved in the years since. Conventionally this procedure involves a traditional open transverse cervicotomy at the level of the cyst which creates a visible cutaneous scar (1). The transoral vestibular approach as a means of access to the central neck has gained visibility in recent years due to the favorable results for thyroid and parathyroid removal [transoral endoscopic thyroidectomy vestibular approach (TOETVA) and transoral endoscopic parathyroidectomy vestibular approach (TOEPVA)] (8-10). The knowledge that such glands are located at the same field as the TGDC has led to extrapolation of the technique to treat TGDC. Authors have published two case reports (3,4) and the first case series (2) detailing the successful excision of TGDC with transoral access. This novel technique has gained the acronym of TEVAS (transoral endoscopic vestibular approach Sistrunk procedure). More recently, two publications described the technique step by step (11,12).
Objective
The aim of this report is to describe our own experience and outcomes with TEVAS and review the current literature on this topic. We present this article in accordance with the PRISMA-ScR and CARE reporting checklists (available at https://gs.amegroups.com/article/view/10.21037/gs-23-357/rc).
Methods
We describe a case of an endoscopic Sistrunk procedure performed by the transoral vestibular approach (TEVAS) for the first time in Brazil along with a scoping review of the literature.
The literature search was done between April 16th and June 6th 2023 in the PubMed, Cochrane, Lilacs, Scielo, Mary Ann Libert and Scopus databases. The entry terms were: “Thyroglossal Cyst”Mesh AND “Thyroglossal Cyst/congenital”Mesh OR “Thyroglossal Cyst/surgery”Mesh OR “Thyroglossal cyst”Mesh AND “Minimally Invasive Surgical Procedures”Mesh OR TEVAS OR Sistrunk OR TOETVA.
Articles involving other remote access surgery for TGDC which do not employ the transoral endoscopic vestibular approach such as transaxillary, transthoracic, retroareolar and retroauricular were excluded. Studies which addressed gasless techniques were also excluded. Only articles in English, Spanish or Portuguese were selected to be fully read. The selection of papers followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (13).
All sources of evidence were accepted in this review. The extracted variables were number of cases, age of the patients, cyst dimension, previous infection of the cyst, operative time, antibiotics used during surgery, antibiotics used in the postoperative period, duration of antibiotic therapy, hospital length of stay, incidence of complications, recurrence, and duration of follow-up.
All data were compiled using REDCap.
This study has IRB approval from Santa Casa de São Paulo School of Medical Sciences (Number: 5.446.616; CAAE: 58637322.0.0000.5479) in accordance with the ethical standards of the committee on human experimentation of the Helsinki Declaration (revised in 2013). The patient enrolled in the case report gave written informed consent to participate in this study. A patient perspective letter is added as Appendix 1. In the attached file, the patient explains how she experienced her disease from the time of the diagnosis until the surgical treatment and follow-up.
Results
Case report
A 35-year-old female presented with a painless midline neck mass. She denied dysphagia and dysphonia, and did not have local changes such as hyperemia or drainage. She was healthy and denied any past medical history. The physical examination showed a 2 cm spheric mass at the level of the hyoid bone, to the left of midline. The CT scan showed a left paramedian cystic formation with a thin capsule at the level of the hyoid bone measuring 1.8 cm in diameter (Figure 1). There were no inflammatory signs. The image findings suggested the diagnosis of a TGDC. After discussing the treatment options, the transoral endoscopic vestibular approach was chosen as the patient expressed a strong preference to avoid a visible neck scar. Informed consent for this case report was provided by the patient.

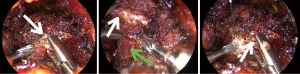
At the time of surgery, the patient underwent general anesthesia with oral intubation and was positioned supine with slight cervical extension. Amoxicillin-clavulanate was given as antibiotic prophylaxis. A 2% lidocaine with epinephrine mixture was injected at the site of the planned incisions in the oral vestibule. Ten mL was injected to the central port, taking care to infiltrate underneath the mentum to separate muscle off the bone and create a small pouch, and 5 mL to each lateral commissure port. The mucosal incisions were made and a Halsted hemostat was used through the central port to locate the periosteal plane of the mandible. Then, a Kelly hemostat was used to open the subplatysmal plane and to perform the first dilation of the tract. This step was followed by progressive dilation with Hegar dilators and placement of a Foley catheter through the central port to assist in creating a working space. The 11 mm central trocar was then placed and the carbon dioxide (CO2) insufflation initiated, with a pressure of 6 mmHg and flow of 10 L/min. Superficial dilation of the lateral ports was performed and 5 mm trocars were placed under direct visualization (Figure 2). A 10 mm/0º endoscope was introduced into the working space pocket created by the foley catheter dilation. This pocket was further developed by utilizing a Maryland dissector (in the surgeon’s left hand) to suspend the skin flap while the right hand utilized an advanced bipolar scalpel dissector to further develop the subplatysmal plane. After creating a satisfactory working space, the assistant switched to a 10 mm/30º endoscope and the surgeon performed the midline opening of the strap muscles. Once the midline was opened, the TGDC was visualized. Soft tissue dissection was performed with the advanced bipolar scalpel in order to circumferentially release the surface of the TGDC. We carefully left some soft tissue above the cyst to facilitate grasping and mobilization (Figure 3).

After releasing the entire cyst, the hyoid bone was fully exposed with monopolar energy using a hook. Grasping the hyoid bone was a challenging step due to the acute working angle, so once the hyoid bone body was clean an open Alligator grasper was used to push the bone towards the external notch, in order to expose the sites of planned osteotomies. The hyoid bone was cut with a 2.4 mm diamond drill, with the lead surgeon switching instruments between her two hands to perform each osteotomy (Figure 4). A puncture was made with a regular peripheral vein catheter through the skin to irrigate the drill bit. Any remaining soft tissue attachments below the cyst were divided with the advanced bipolar scalpel. Once the cyst remained attached only to the thyroglossal duct, the tract was then ligated with a hemolock clip and divided, releasing the specimen (Figures 5,6).

The specimen was removed in an endocatch bag through the central port (Figure 7). The midline strap muscles were closed with absorbable sutures with the intention to avoid fibrosis and any unaesthetic appearance of the patient’s neck. Oral incisions were closed with regular 4.0 catgut sutures. The operative time was 180 minutes.
An anterior neck pressure dressing was placed after the surgery and remained in place overnight. The patient was discharged on the first postoperative day (Figure 8). There were no complications during hospitalization. She was discharged on amoxicillin-clavulanate 875 + 125 mg for 5 days with instructions for oral hygiene with chlorhexidine 0.12% solution 3 times a day for 1 week. She maintained a soft diet for 2 days. There were no postoperative complications. She was seen 10 days after surgery, at which time the oral incisions were healed, she was tolerating a regular diet, and had resumed normal activities. She noted submental tenderness but denied mental or submental numbness. During the first 2 weeks after the procedure the patient underwent 5 or 6 physiotherapy sessions in order to treat and prevent fibrosis. She returned for her final evaluation after 4 months without any complaints. There were no signs of recurrence of the mass. At 19 months post-operative she remains without recurrence, complaints, or complications.

Review
This review found 1,488 articles in PubMed, 837 in Cochrane, 1,168 in Lilacs, 14 in Scielo, 1,163 in Mary Ann Liebert and 1,894 in Scopus. The total number was 6,564 articles. A total of 4,567 articles were excluded because they were duplicates between the databases. A total of 932 were excluded because they were out of the scope of our intended topic, and 1,015 articles were excluded because they addressed TGDC or the Sistrunk procedure but not remote access surgery. Forty-five were excluded because they addressed other remote access techniques. A total of 5 articles were included in this review (Figure 9) (13). Three articles are case reports, 1 is a case series and 1 article is an operative technique description.
Ryan et al. (3) reported the first case of TEVAS in a 16-year-old male presenting with a 1.1 cm TGDC with previous infection. A surgeon experienced in the TOETVA technique performed the surgery. An instrument set up similar to that used in TOETVA was utilized in the case with the addition of a 45º degree scope for improved visualization, and an ultrasonic aspirator to perform the hyoid osteotomies. Ampicillin-sulbactam was given as surgical prophylaxis, and a 5-day course of amoxicillin-clavulanate was prescribed post operatively. The hospital length of stay was 1 day. The operative time was not addressed in the article. There were no complications and no signs of recurrence at 3 months. The authors concluded that the technique is safe and effective in selected patients motivated to avoid a visible scar.
A second article by Scott-Wittenborn et al. (12) described the technique step by step and the most important aspects of the technique. Like Ryan et al., they utilized 0°, 30° and 45° scopes and performed the osteotomies using an ultrasonic aspirator. Prophylactic antibiotics, previous cyst infection, and operative time were not addressed. They concluded that the technique is safe and effective but acknowledge that more studies are needed to elucidate if the recurrence rate is comparable to that of the traditional Sistrunk procedure.
Sachs et al. (4) reported a case of TEVAS in a 51-year-old female presenting with a 2.3 cm TGDC. This publication was the first to name the technique with the acronym TEVAS. They recommend using 0°, 30° and 45° scopes, and performing the osteotomies using an ultrasonic aspirator. Antibiotics and operative time were not addressed, although it is mentioned that this kind of procedure takes an average of approximately 5 hours. The hospital length of stay was 1 day. There were no complications and no recurrence, although duration of follow-up was not mentioned. They concluded that the case was completed successfully and risk of recurrence still needs to be established.
Banuchi et al. (2) reported the first case series of 6 patients. The average age was 38 years (range, 16–56 years) and mean body mass index was 24.3 kg/m2 (range, 21–32 kg/m2). Three patients had TGDC infection at some point preoperatively. The mean maximum TGDC dimension as measured by preoperative imaging was 1.8 cm (range, 1.1–2.4 cm). The endoscope angles were not addressed in the article. All patients were discharged on amoxicillin-clavulanate for an average of 6.5 days (range, 5–7 days). Average operative time was 309 minutes (range, 123–495 minutes). No complications or recurrences were reported. The average follow-up duration was 4.5 months (range, 4–7 months). They concluded that the technique is feasible and safe while avoiding an external neck scar.
Nakai et al. (11) published a video report of a successful TEVAS case in a 47-year-old female who presented with a 4.5 cm TGDC without previous infection. This article is the most recent publication on this topic and presented modifications to the technique. There was also a reduction in operative time (mean 150 minutes) compared to previously published cases. The authors demonstrate an alternative way to perform hyoid osteotomies using an ultrasonic scalpel with open jaw. Only 0° and 30° endoscopes were used in the case. After surgery the patient received amoxicillin-clavulanate for 5 days. The hospital length of stay was 1 day. There were no complications and no recurrence after a 4-month follow-up period. They concluded that TEVAS is feasible and previous experience with TOETVA/TOEPVA is an operative advantage in the performance of this surgery.
Table 1 summarizes these data.
Table 1
| Study | Cases | Age (years), sex | Bigger dimension of the cyst (cm) | Operative time (min) | Device used to the osteotomies | Antibiotics | Antibiotics-postoperative [days] | Hospital length of staying (days) | Complications | Recurrence | Preoperative infection | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ryan et al., 2020 | 1 | 16, M | 1.1 | Not informed | Sonopet ultrasonic aspirator | Ampicillin-sulbactam | Amoxicillin-clavulanate [5] | 1 | None | No | Yes | 3 |
| Sachs et al., 2022 | 1 | 51, F | 2.1 | Not informed | Sonopet ultrasonic aspirator | Not informed | Not informed | 1 | None | No | Yes | Not informed |
| Banuchi et al., 2022 | 6 | 51, F | 2.1 | 495 | Sonopet ultrasonic aspirator | Not informed | Amoxicillin-clavulanate [7] | 1 | None | No | Yes | 4 |
| 56, F | 2.4 | 471 | Amoxicillin-clavulanate [7] | Outpatient | No | 4 | ||||||
| 37, F | 2.2 | 123 | Amoxicillin-clavulanate [5] | Not informed | Yes | 4 | ||||||
| 43, F | 1.2 | 220 | Amoxicillin-clavulanate [5] | Not informed | No | 7 | ||||||
| 16, M | 1.1 | 150 | Amoxicillin-clavulanate [5] | Not informed | Yes | 5 | ||||||
| 29, F | 1.7 | 394 | Amoxicillin-clavulanate [5] | Not informed | No | 3 | ||||||
| Nakai et al., 2022 | 1 | 47, F | 4.5 | 150 | Ultrasonic scalpel | Amoxicillin-clavulanate | Amoxicillin-clavulanate [5] | 1 | None | No | No | 4 |
| Nakai et al., 2023* | 1 | 35, F | 1.8 | 180 | Diamond drill bit | Amoxicillin-clavulanate | Amoxicillin-clavulanate [5] | 1 | None | No | No | 19 |
*, case described in this article. M, male; F, female; min, minute.
Discussion
While the Sistrunk procedure is a reliable method to treat a TGDC, the TEVAS technique adds the benefits of endoscopic surgery such as image magnification, ability for data recording, and lack of a visible cutaneous scar (8-10). The technique of transoral neck surgery (TNS) has been shown to be reproducible in different health centers around the world, as it requires only regular laparoscopic instruments without adding excessive costs (8-10). Moreover, the learning curve for TNS is relatively short and the additional operative time is acceptable (10,14,15). The transoral vestibular approach has been applied successfully for thyroidectomies (TOETVA), parathyroidectomies (TOEPVA) and chondrolaryngoplasty (8-10,16).
Prior to TEVAS, a similarly intentioned approach to treat TGDC that involved access to the anterior neck through the floor of the mouth was published in 2011 (17). This was followed by a series of 30 cases with no complications or recurrence after 2 years of follow-up, but with a more prolonged hospitalization (18). This technique was met with criticism among Western surgeons due to the risk of impairment of nerves such as the hypoglossal and lingual. In 2018, Han et al. (19) reported a successful case series of TGDC excision by gasless transoral vestibular approach. In 2020, Ryan et al. (3) published the first case of TEVAS which was discussed earlier in this paper.
The indications for TEVAS includes patients motivated to avoid a visible neck scar, including those with a past history of hypertrophic scarring or keloids (2-4). Significant skin involvement and fistulization of the TGDC as well as previous neck radiotherapy should be formal contraindications for TEVAS (2-4,11,12). The presence of any synthetic material in front of the arch of the mandible such as metallic plaques or chin prosthesis should be contraindications as well. The presence of a visible neck scar should be evaluated individually, as the preference of the patient should be considered (11). One of the most common reasons for an existing neck scar is from previous thyroidectomy or parathyroidectomy. Many of these procedures were performed with a low incision for improved cosmesis, and would not provide adequate access to remove a TGDC should the surgeon attempt to use the previous incision. In these cases, an additional higher incision is commonly necessary in order to remove the TGDC (11). Challenging cases such as TGDC presenting with extensive contact with lingual musculature should be avoided at the beginning of the learning curve, but it is not a formal contraindication (11). If there is any suspicion for malignancy, fine needle aspiration biopsy is recommended prior to the procedure, as a known TGDC malignancy would not be recommended to be treated with TEVAS (2-4,11,12).
The published series by Banuchi et al. show that there is a significant increase in length of operative time over the traditional Sistrunk procedure (2). This should be considered when evaluating elderly patients as well individuals with medical comorbidities for TEVAS (2,3). Until we have more data available regarding the safety profile and long-term outcomes, we recommend avoiding this procedure in patients over 75 years old or ASA score III or greater. Overall, our operative time was shorter than the cases described previously (2-4). We believe that our previous experience with other TNS was preponderant to performing a faster procedure.
The volume of the cyst should also be considered before offering the procedure. In large cysts, an ultrasound guided needle aspiration can be performed to reduce the cyst volume after induction of anesthesia (2,11). The cyst can also be aspirated endoscopically during surgery to reduce volume, making it easier to mobilize and grasp the tissue. Even with the possibility of aspiration, larger cysts can be more challenging due to redundant tissue in front of the scope. Therefore, we recommend cysts smaller than 5 cm for the first cases.
As seen at the beginning of TOETVA’s implementation, one concern among surgeons is the possibility of surgical site infection, as the access creates a communication between the mouth and the neck (8-10). As this is a novel technique, there are no long-term prospective studies which compare infection rates between TEVAS and the open Sistrunk procedure. However, seeing that TEVAS uses the same surgical access of other transoral neck surgeries, the infection rates would be presumably be comparable between both procedures. The published literature on TOETVA and TOEPVA show similar infection rates when compared to open surgery (8-10). We recommend the use of antibiotics to cover mouth microbiota such as amoxicillin-clavulanate or ampicillin-sulbactam (2,11).
Although rare, a major concern during TNS is CO2 embolism (19,20), as it can be a lethal complication. It is a very rare occurrence and usually associated with injuring large vessels (such as the anterior jugular veins) while running CO2 insufflation (21,22). At this time, there is no existing specific data regarding TEVAS and CO2 embolism. To avoid CO2 embolism, it is recommended to always perform delicate dissection and agile ligation of large bleeding vessels, and to stop CO2 insufflation in the case of suspected injury or bleeding from these large vessels. The anesthesia team should be made aware of the risk as they have a crucial role in management of this complication (21,22).
Other concerns such as skin tears and burns, zygoma and lip bruising, and mental nerve injury may occur in the beginning of the learning curve, but we don’t believe that an experienced surgeon in TNS technique should have these problems routinely. Zygoma bruises should be avoided by protecting the face of the patient with soft material such as specific face protection or foam sponges. Lip bruises occur when the lateral ports are placed too close to the commissures combined with abrupt movements with the instruments. The support of a more experienced surgeon as a proctor in the first cases may avoid such complications. Neck adhesions or fibrotic scar tissue may occur after TEVAS, similar to the open approach. Should fibrosis occur, it would be expected in the upper dissection plane descending from the mentum compared to directly over the area of TGDC such as seen in the open procedure. Neck exercises, physical therapy and lower frequency laser may be used to ease these complaints. Mental nerve injury clinically presents itself as numbness in the mental or submental area. This complication has decreased in incidence in TOETVA patients after the modifications made in the placement of the lateral trocars to a position closer to the lip commissures (9). When a patient presents with clinical signs of mental nerve injury, it is usually a temporary hypoesthesia that recovers within 30 days. Permanent mental numbness is rare (9,10).
As a new technique, no standardized approach is yet established. Compared to TOETVA, the working space is smaller and the plane of dissection is shorter. The operating angles of the instruments are more oblique than in TOETVA, which requires the surgeon to work with their arms in a wider position. This could provoke more bruising to the lip commissures due to the lateral torque on the tissues. The assistant who is managing the camera should be aware of the small working space and understand that the scope should have a dynamic movement to avoid smoke plume and the spray of the ultrasonic scalpel. If the team is not prepared for this, it can be an exhausting aspect of this surgery, as the scope could get dirty after every use of the ultrasonic scalpel. In this case we used two scopes, a 0º/10 mm and a 30º/10 mm. Other authors describe the usage of a third 45º/10 mm scope during the hyoid bone dissection, which may improve the visualization of the TGDC and hyoid bone (3).
The most challenging step while performing TEVAS is the hyoid bone osteotomies. In this case we performed the osteotomies using a 2.4 mm diamond drill. Other authors described the usage of an ultrasonic aspirator to cut the bone (2-4). We believe that the best instrument to cut the hyoid is the ultrasonic scalpel, as it easily performs the osteotomies by contacting the hyoid bone on each side with its’ active blade while the jaws are in the open position (11). The ultrasonic scalpel can also then be used as the energy instrument for the case, avoiding the use of additional instruments such as advanced bipolar. After the osteotomies the surgeon should carefully ligate the thyroglossal duct tract using absorbable sutures or hemolocks. Exposing the tract is another challenging step of this surgery once the endoscopes give a two-dimensional view. However, once the team is well experienced in TNS this limitation should not be a barrier to perform proper tract dissection and ligation, once, the 30º scope allows the surgeon to visualize the TGDC and its tract from different perspectives (anterior to posterior, superior to inferior and lateral view)
As TNS for thyroid removal is cosmetically superior when compared to open surgery (23-25), TEVAS may show the same results after comparison. While other benefits beyond improved cosmesis are not yet seen, the safety profile of TEVAS appears similar to the open procedure, based on the currently published data and our own experience. Therefore, we believe that the choice for this novel approach should be made by the appropriately indicated patient after the physician explains both existing techniques.
The present study reviewed the current literature on TEVAS. To date there are only a few publications detailing this technique, and this was the major limitation of this scoping review. It should also be noted that most currently available publications are case reports or case series, which have a low level of evidence. Although more data is necessary, our hope is that this paper concentrating all currently available data on TEVAS may encourage more widespread adoption of the technique, as was seen with TOETVA and TOEPVA.
Conclusions
In this study we have summarized the currently available literature on TEVAS as well as reported our own successful case. The published data shows comparable complication and recurrence rates to the Sistrunk procedure, although further patient studies and longer-term follow-up are needed. Although the operative time is considerably longer than the open approach, our own experience shows that this variable improves with increased operator experience in endoscopic transoral procedures. This novel approach is an efficient technique for treating TGDC in selected patients who are motivated to avoid a visible neck scar.
Acknowledgments
We want to acknowledge the patient, who gave us permission to report her case.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA-ScR and CARE reporting checklists. Available at https://gs.amegroups.com/article/view/10.21037/gs-23-357/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-357/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-23-357/coif). M.Y.N. is a speaker for DMC. J.O.R. is a consultant for Baxter scientific and does expert testimony for Baxter scientific. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study has IRB approval from Santa Casa de São Paulo School of Medical Sciences (Number: 5.446.616; CAAE: 58637322.0.0000.5479) in accordance with the ethical standards of the committee on human experimentation of the Helsinki Declaration (revised in 2013). The patient enrolled in the case report gave written informed consent to participate in this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sistrunk WE. The surgical treatment of cysts of the thyroglossal tract. Ann Surg 1920;71:121-122.2.
- Banuchi VE, Long SM, Sachs BY, et al. Transoral endoscopic vestibular approach Sistrunk procedure: First reported case series. Head Neck 2022;44:E1-5. [Crossref] [PubMed]
- Ryan MA, Russell JO, Schoo DP, et al. Transoral Endoscopic Vestibular Thyroglossal Duct Cyst Excision. Ann Otol Rhinol Laryngol 2020;129:1239-42. [Crossref] [PubMed]
- Sachs BY, Kostas JC, Long SM, et al. Transoral Endoscopic Vestibular Approach to the Sistrunk Procedure. Laryngoscope 2022;132:711-4. [Crossref] [PubMed]
- Anderson JL, Vu K, Haidar YM, et al. Risks and complications of thyroglossal duct cyst removal. Laryngoscope 2020;130:381-4. [Crossref] [PubMed]
- Goldsztein H, Khan A, Pereira KD. Thyroglossal duct cyst excision—The Sistrunk procedure. Oper Tech Otolayngol Head Neck Surg 2009;20:256-9.
- Rohof D, Honings J, Theunisse HJ, et al. Recurrences after thyroglossal duct cyst surgery: Results in 207 consecutive cases and review of the literature. Head Neck 2015;37:1699-704. [Crossref] [PubMed]
- Anuwong A, Sasanakietkul T, Jitpratoom P, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): indications, techniques and results. Surg Endosc 2018;32:456-65. [Crossref] [PubMed]
- Russell JO, Clark J, Noureldine SI, et al. Transoral thyroidectomy and parathyroidectomy - A North American series of robotic and endoscopic transoral approaches to the central neck. Oral Oncol 2017;71:75-80. [Crossref] [PubMed]
- Bertelli AAT, Rangel LG, Lira RB, et al. Trans Oral Endoscopic Thyroidectomy Vestibular Approach (TOETVA) in Brazil: Safety and complications during learning curve. Arch Endocrinol Metab 2021;65:259-64. [Crossref] [PubMed]
- Nakai MY, Tenório LR, Menezes MB, et al. Transoral Endoscopic Vestibular Approach Sistrunk Procedure: Surgery Video. VideoEndocrinology 2022;9:76-8.
- Scott-Wittenborn N, Tufano RP, Walsh JM, Russell JO. Transoral sistrunk procedure. Oper Tech Otolayngol Head Neck Surg 202;323:179-82.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372: [Crossref] [PubMed]
- Razavi CR, Vasiliou E, Tufano RP, et al. Learning Curve for Transoral Endoscopic Thyroid Lobectomy. Otolaryngol Head Neck Surg 2018;159:625-9. [Crossref] [PubMed]
- Lira RB, Ramos AT, Nogueira RMR, et al. Transoral thyroidectomy (TOETVA): Complications, surgical time and learning curve. Oral Oncol 2020;110:104871. [Crossref] [PubMed]
- Banuchi VE, Helman SN. Scarless Neck Feminization: Chondrolaryngoplasty Through Endoscopic Transoral Vestibular Approach. Laryngoscope 2023;133:1099-102. [Crossref] [PubMed]
- Kim JP, Park JJ, Lee EJ, et al. Intraoral removal of a thyroglossal duct cyst using a frenotomy incision. Thyroid 2011;21:1381-4. [Crossref] [PubMed]
- Woo SH, Park JJ, Hong JC, et al. Endoscope-assisted transoral removal of a thyroglossal duct cyst using a frenotomy incision: A prospective clinical trial. Laryngoscope 2015;125:2730-5. [Crossref] [PubMed]
- Han P, Liang F, Cai Q, et al. Endoscope-assisted resection of thyroglossal duct cysts via a submaxillary vestibular approach. Head Neck 2018;40:377-83. [Crossref] [PubMed]
- Tae K, Kim HR. Transoral robotic excision of thyroglossal duct cyst using vestibular and sublingual incisions. Head Neck 2022;44:2640-4. [Crossref] [PubMed]
- Russell JO, Vasiliou E, Razavi CR, et al. Letter to the Editor regarding "Carbon dioxide embolism during transoral robotic thyroidectomy: A case report". Head Neck 2019;41:830-1. [Crossref] [PubMed]
- Kim KN, Lee DW, Kim JY, et al. Carbon dioxide embolism during transoral robotic thyroidectomy: A case report. Head Neck 2018;40:E25-8. [Crossref] [PubMed]
- Banuchi VE, Ballakur SS, Russell JO, et al. Benefits and risks of scarless thyroid surgery. Ann Thyroid 2020;5:24.
- Juarez MC, Ishii L, Nellis JC, et al. Objectively measuring social attention of thyroid neck scars and transoral surgery using eye tracking. Laryngoscope 2019;129:2789-94. [Crossref] [PubMed]
- Chen LW, Razavi CR, Hong H, et al. Cosmetic outcomes following transoral versus transcervical thyroidectomy. Head Neck 2020;42:3336-44. [Crossref] [PubMed]






