
Lateral neck dissection surgeon volume and complications in head and neck endocrine malignancy
Highlight box
Key findings
• One subgroup from two databases demonstrated a significant increase in complications with increasing surgeon volume among intermediate volume surgeons performing lateral neck dissection for thyroid or parathyroid malignancy.
What is known and what is new?
• Prior literature demonstrates decreasing complication rates with increasing surgeon volume for thyroidectomy, and increased risk for complications when a neck dissection is performed with a thyroidectomy. No study has evaluated for an association between neck dissection surgeon volume and complication rates in thyroidectomy patients requiring a lateral neck dissection.
• This multi-database analysis focuses on the relationship between lateral neck dissection surgeon volume and complications.
What is the implication, and what should change now?
• Increased complications with increasing surgeon volumes in one subgroup raises awareness of the nuanced complexity with the treatment of metastatic thyroid and parathyroid cancer.
Introduction
Improved patient outcomes are correlated with increased surgical experience in various surgical procedures and subspecialties (1-7), including thyroidectomy (8). Involvement of lateral cervical lymph nodes occurs in approximately 20–30% of thyroid cancer cases (9). While such regional metastasis may not adversely affect survival (10,11), there may be an association between mortality and lymph node metastasis in certain patient populations (11-13). With nearly 53,000 new thyroid cancer cases per year in the United States (14), that leaves many endocrine malignancy patients in need of lateral neck dissection. In the face of this high volume of surgical procedures, the increased risk of complications that comes with performing a lateral neck dissection (15,16), and the lack of existing research on the subject, we sought to examine the relationship between surgeon volume (SV) and complication rates for lateral neck dissection in patients with thyroid and parathyroid malignancy.
In order to provide data for research regarding improved healthcare delivery and informed medical decision making, the Health Care Utilization Project (HCUP) created the State Inpatient Databases (SID) and the Nationwide Inpatient Sample (NIS). The SID consists of all inpatient discharge records for patients of all payors from community hospitals in a given state (17). The NIS is a publicly available data set sourced from the SID, involving most states in the US, and encompassing 5 million to 8 million inpatient discharges from about 20% of US hospitals prior to a 2012 overhaul (18). The NIS has been utilized to consider the effects of SV on outcomes in other procedures (8,19,20), as has the SID (21-23). We included the NIS because it represents a national sample, and the SID was included for comparison. While our SID cohort was only drawn from 3 states, the surgeon tracking methodology is more stable in this data set, and it gathered data from all discharges in a state, not just a sample of those discharges as seen in the NIS. The principle aim of this study was to use these databases as a retrospective, cross-sectional cohort to assess the relationship between SV and complications for patients undergoing lateral neck dissection for thyroid and parathyroid cancer. We hypothesized that increased SV would be associated with decreased complication rates. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-385/rc).
Methods
The Duke University Health System Institutional Review Board assigned a human subjects research exemption. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Individual consent for this retrospective analysis was waived. A retrospective review of the NIS hospital discharge data from 2000 to 2009 including states with documentation of reliable surgeon tracking (Table S1) and the SID data from New York, Florida, and Iowa spanning 2013–2014 was performed. We queried the NIS prior to 2010 because it ceased to track surgeon identifiers from 2010 and beyond, making it impossible to calculate SV. We utilized the specific SID data set because it was already available at our institution. First, we sought to calculate an annual SV of all lateral neck dissection for each surgeon identifier in the data sets, regardless of principle diagnosis [e.g., a surgeon with 5 neck dissections for squamous cell carcinoma (SCC) and 4 for thyroid cancer would have an overall SV of 9]. Lateral neck dissection cases were identified with International Classification of Diseases, Ninth Revision (ICD-9) procedure codes (ICD-9 40.40, 40.41, 40.42, 40.3). Cases with the procedure code for general lymph node excision (ICD-9 40.3) were included if they also had a code for SCC of the head and neck, cutaneous malignancy, other head and neck malignancy, or salivary gland malignancy. Tables S2,S3 list all utilized codes. Thus, all lateral neck dissection cases, irrespective of the principal diagnoses, were used to calculate the number of lateral neck dissection cases a surgeon performed per year. Encounters with missing surgeon identifiers were excluded from the study, because SV could not be assessed for these encounters. Second, we formed our study cohort by identifying discharges that involved lateral neck dissection with a principal diagnosis of thyroid or parathyroid malignancy (ICD-9 193, 194, 239.7). Therefore, all lateral neck dissections were used to calculate SV for surgeon identifiers, but complications rates were only analyzed in discharges for patients undergoing lateral neck dissection for thyroid or parathyroid malignancy.
Statistical analysis
The primary outcome was incidence of one or more complications during the inpatient stay, which included nerve injury to the head or neck, chyle leak, hematoma, hypoparathyroidism, hypocalcemia, vocal cord paralysis, tracheotomy, and wound complications. The primary exposure was annual SV, defined as the number of total neck dissections performed by a surgeon per year (not just for thyroid or parathyroid disease). Covariates used for evaluating risk included urgent/emergent admission, age, gender, race, payor, hospital size, hospital teaching status, hospital geographic region, and Elixhauser comorbidity score (24). Hospital information is not available in SID and thus not included in the SID analysis.
Two independent analyses were performed using the two data sets. A preliminary analysis utilizing restricted cubic splines (RCS) was performed to assess the potential nonlinear relationship of the SV with the incidence of any complication using in a univariate logistic regression model. By varying the number of knots from 3 to 6 and placing the knots based on Frank Harrell’s recommended percentiles (25), we selected the model with the lowest observed Akaike Information Criterion to represent the functional form and assessed non-linear association of SV with complication using a Wald test. If non-linear association was not detected, SV was included as a linear term in the multivariable analysis. If non-linear association was detected, we plotted SV and the corresponding estimated logarithm of the odds ratio (OR) and identified inflection points to represent SV with a piecewise linear spline using these inflection points. After the functional form of SV was determined, we then fit a multivariable logistic generalized estimating equation (GEE) to examine the association of SV with complications using a compound symmetric correlation structure to account for clustering of discharges within surgeons and clustering of surgeons within hospitals. Covariates included urgent/emergent admission, age, gender, race, payor, hospital size, hospital teaching status, hospital geographic region, and Elixhauser comorbidity score. Hospital information is not available in the SID and thus not included in the SID analysis. In addition, as a sensitivity analysis, the association between SV and complication was assessed by categorizing SV into the volume quartiles defined by all lateral neck dissections in either the NIS or SID cohorts, and the relationship between SV and complication was assessed. All analyses were unweighted and performed using SAS 9.4 (SAS Institute, Cary, NC, USA). A two-sided significance level of 0.05 was used for all statistical tests. Any table data point (e.g., number of nerve injuries) of 10 or less were not reported according to the standard HCUP Data Use Agreement.
Results
The NIS resulted in 1,094 discharges, with the demographics represented in Table 1. There was an overall complication rate of 27.9% (305/1,094), with the specific complications represented in Table 2. The specific complications for both databases are stratified by SV quartile in Table 3. Patients whose neck dissection was performed by a surgeon with volume between 27–92 (last quartile) were more likely to be in large, teaching hospitals. This group also had the highest surgical complication rate of 37.1% (75/202, Table 3).
Table 1
| Demographics | Neck dissection volume (1–2 per year) (n=367) | Neck dissection volume (3–7 per year) (n=311) | Neck dissection volume (8–26 per year) (n=214) | Neck dissection volume (27–92 per year) (n=202) | Total (n=1,094) |
|---|---|---|---|---|---|
| Age (years) | 50 [36–66] | 48 [35–64] | 48 [34–63] | 49 [37–64] | 48 [35–64] |
| Race | |||||
| Missing | 33 | 32 | 16 | 17 | 98 |
| White | 250 (74.9) | 222 (79.6) | 134 (67.7) | 129 (69.7) | 735 (73.8) |
| Female sex | 227 (61.9) | 183 (58.8) | 133 (62.1) | 118 (58.4) | 661 (60.4) |
| Primary expected payer | |||||
| Medicare | 94 (25.6) | 77 (24.8) | 48 (22.4) | 42 (20.8) | 261 (23.9) |
| Medicaid | 21 (5.7) | 17 (5.5) | 20 (9.3) | 15 (7.4) | 73 (6.7) |
| Private insurance | 224 (61.0) | 201 (64.6) | 138 (64.5) | 132 (65.3) | 695 (63.5) |
| Urgent/emergent admission | 38 (10.4) | 32 (10.3) | 17 (8.0) | 21 (10.4) | 108 (9.9) |
| Bed size of hospital | |||||
| Missing | 0 | 3 | 0 | 10 | 13 |
| Large | 218 (59.4) | 213 (69.2) | 151 (70.6) | 153 (79.7) | 735 (68.0) |
| Teaching hospital | |||||
| Missing | 0 | 3 | 0 | 10 | 13 |
| Teaching hospital | 199 (54.2) | 189 (61.4) | 178 (83.2) | 190 (99.0) | 756 (69.9) |
| Geographic region of hospital | |||||
| Northeast | 95 (25.9) | 92 (29.6) | 80 (37.4) | 55 (27.2) | 322 (29.4) |
| South | 206 (56.1) | 158 (50.8) | 117 (54.7) | 118 (58.4) | 599 (54.8) |
| Elixhauser comorbidity score | 13 [9–13] | 13 [3–13] | 12 [0–13] | 13 [8–13] | 13 [7–13] |
Data are presented as median [IQR] or n (%). IQR, interquartile range.
Table 2
| Variables | NIS sample (n=1,094) | SID sample (n=1,235) |
|---|---|---|
| Any complication | 305 (27.9) | 258 (20.9) |
| Chyle leak | * | 18 (1.5) |
| Wound complications | 23 (2.1) | 12 (1.0) |
| Nerve injury | * | * |
| Hematoma | 28 (2.6) | 27 (2.2) |
| Hypoparathyroidism | 48 (4.4) | 35 (2.8) |
| Hypocalcemia | 187 (17.1) | 150 (12.1) |
| Vocal cord paralysis | 55 (5.0) | 54 (4.4) |
| Tracheotomy | 35 (3.2) | 26 (2.1) |
Data are presented n (%). *, cell sizes ≤10 patients are not reported according to HCUP Data Use Agreement. NIS, Nationwide Inpatient Sample; SID, State Inpatient Database; HCUP, the Health Care Utilization Project.
Table 3
| Data sources | First SV quartile | Second SV quartile | Third SV quartile | Fourth SV quartile | P value |
|---|---|---|---|---|---|
| Nationwide Inpatient Sample | 1–2 per year (n=367) | 3–7 per year (n=311) | 8–26 per year (n=214) | 27–92 per year (n=202) | – |
| Any complication | 88 (24.0) | 80 (25.7) | 62 (29.0) | 75 (37.1) | 0.007 |
| Hypocalcemia | 50 (13.6) | 48 (15.4) | 42 (19.6) | 47 (23.3) | 0.018 |
| Vocal cord paralysis | 12 (3.3) | 18 (5.8) | 12 (5.6) | 13 (6.4) | 0.29 |
| State Inpatient Database | 1–8 per year (n=348) | 9–26 per year (n=378) | 27–45 per year (n=214) | 46–100 per year (n=295) | – |
| Any complication | 87 (25.0) | 69 (18.3) | 43 (20.1) | 59 (20.0) | 0.147 |
| Hypocalcemia | 56 (16.1) | 39 (10.3) | 22 (10.3) | 33 (11.2) | 0.07 |
Data are presented as n (%). SV, surgeon volume.
The SID resulted in 1,235 discharges (863 discharges from New York, 332 discharges from Florida, and 40 discharges from Iowa) with the demographics represented in Table 4. There was an overall complication rate of 20.9% (258/1,235), with specific complications represented in Table 2. Patients whose neck dissection was performed by a surgeon with volume between 46–100 (last quartile) were more likely to be white, have private insurance, and have a higher Elixhauser comorbidity score. The surgeons with volume between 1–8 (the first quartile) had the highest complication rate of 25.0% (87/348, Table 3).
Table 4
| Demographics | Neck dissection volume (1–8 per year) (n=348) | Neck dissection volume (9–26 per year) (n=378) | Neck dissection volume (27–45 per year) (n=214) | Neck dissection volume (46–100 per year) (n=295) | Total (n=1,235) |
|---|---|---|---|---|---|
| Age (years) | 48 [36–62] | 50 [37–61] | 47 [34–65] | 48 [36–59] | 48 [36–62] |
| Race | |||||
| White | 208 (59.8) | 166 (43.9) | 126 (58.9) | 212 (71.9) | 712 (57.7) |
| Female sex | 217 (62.4) | 246 (65.1) | 123 (57.5) | 183 (62.0) | 769 (62.3) |
| Urgent/emergent admission | 66 (19.0) | 81 (21.4) | 24 (11.2) | 58 (19.7) | 229 (18.5) |
| Primary expected payor | |||||
| Medicare | 73 (21.0) | 77 (20.4) | 55 (25.7) | 46 (15.6) | 251 (20.3) |
| Medicaid | 66 (19.0) | 72 (19.0) | 16 (7.5) | 25 (8.5) | 179 (14.5) |
| Private insurance | 192 (55.2) | 214 (56.6) | 134 (62.6) | 210 (71.2) | 750 (60.7) |
| Elixhauser comorbidity score | 12 [0–13] | 12 [0–13] | 12 [8–13] | 13 [11–13] | 12 [3–13] |
Data are presented as median [IQR] or n (%). IQR, interquartile range.
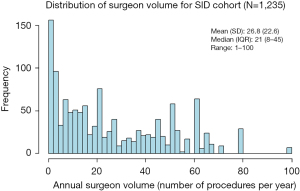
The NIS contained 666 unique surgeon identifiers with an SV range of 1–92, mean of 14.3 (SD 20.1), and median of 5. The SID contained 398 unique surgeon identifiers with an SV range of 1–100, mean of 26.8 (SD 22.6), and median of 21. The distributions of the SV of the NIS and SID cohorts can be found in Figures 1,2, respectively.

Using an SV of 1 case/year as the reference, Figures 3,4 demonstrate the relationship of SV, represented by RCS, with the OR of complication for the NIS and SID, respectively. The results of the univariate regression with RCS showed a non-linear relationship between SV and complication of the NIS sample (P=0.024), with the relationship changing at SVs of 3 and 34. There was no significant non-linear or overall relationship between SV and complications upon univariate regression with RCS of the SID sample (P=0.12 and P=0.25, respectively).

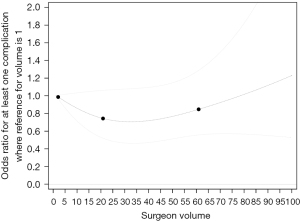
We used piecewise linear splines to represent SV in the multivariable regression, with results demonstrated in Table 5. For the NIS, as SV increased from 1 to 3 surgeries per year, the odds of complication did not change significantly [OR: 1.04; 95% confidence interval (CI): 0.84–1.29; P=0.72]. As SV increased from 3 to 34, one-unit increase in SV was associated with a 3% increase in the odds of at least one surgical complication (OR: 1.03; 95% CI: 1.01–1.05; P=0.004). The odds of complication did not change with volume when volume was above 34 (OR: 0.99; 95% CI: 0.96–1.01; P=0.20). Urgent admission status, Elixhauser comorbidity and female sex were also associated with increased odds of complications in the NIS. As SV in the SID increased by 1 surgery per year, the odds of complication did not change significantly after accounting for covariates and clustering of surgeons and hospitals (OR: 1.00; 95% CI: 1.00–1.01; P=0.32). Medicaid and insurance other than private insurance or Medicare, as well as Elixhauser comorbidity were associated with increased odds of complications in the SID.
Table 5
| Comparison | Nationwide Inpatient Sample | State Inpatient Database | |||
|---|---|---|---|---|---|
| Adjusted odds ratio (95% CI) | P value | Adjusted odds ratio (95% CI) | P value | ||
| 1-unit SV increase when volumes ≤3 | 1.04 (0.84–1.29) | 0.72 | – | – | |
| 1-unit SV increase when volumes [4, 33] | 1.03 (1.01–1.05) | 0.004 | – | – | |
| 1-unit SV increase when volumes ≥34 | 0.99 (0.96–1.01) | 0.20 | – | – | |
| 1-unit SV increase for all SV volumes | – | – | 1.00 (1.00–1.01) | 0.32 | |
| Age (1 unit) | 1.01 (1.00–1.02) | 0.23 | 1.00 (0.99–1.02) | 0.37 | |
| Male vs. female | 0.66 (0.49–0.89) | 0.007 | 1.01 (0.77–1.32) | 0.95 | |
| Race | |||||
| Black vs. White | 1.56 (0.81–3.02) | 0.18 | 1.23 (0.62–2.45) | 0.55 | |
| Hispanic vs. White | 0.96 (0.64–1.42) | 0.82 | – | – | |
| Other races vs. White | 1.00 (0.61–1.63) | >0.99 | 0.86 (0.63–1.17) | 0.33 | |
| Payor | |||||
| Medicaid vs. private insurance | 0.68 (0.36–1.28) | 0.23 | 0.59 (0.39–0.89) | 0.013 | |
| Medicare vs. private insurance | 0.78 (0.48–1.26) | 0.30 | 0.91 (0.60–1.37) | 0.65 | |
| Other insurance vs. private insurance | 0.92 (0.50–1.68) | 0.78 | 0.46 (0.26–0.81) | 0.007 | |
| Hospital size | |||||
| Large vs. small bed size hospital | 0.88 (0.55–1.40) | 0.59 | – | – | |
| Medium vs. small bed size hospital | 0.78 (0.44–1.37) | 0.38 | – | – | |
| Teaching vs. non-teaching hospital | 0.81 (0.57–1.15) | 0.24 | – | – | |
| Hospital geographic region | |||||
| Midwest vs. south | 0.84 (0.43–1.64) | 0.61 | – | – | |
| Northeast vs. south | 0.77 (0.52–1.13) | 0.18 | – | – | |
| West vs. south | 0.79 (0.37–1.7) | 0.54 | – | – | |
| Urgent vs. not urgent admission | 1.61 (1.02–2.56) | 0.042 | 1.15 (0.81–1.63) | 0.45 | |
| Elixhauser comorbidity (1 unit) | 1.03 (1.00–1.05) | 0.02 | 0.94 (0.92–0.96) | <0.0001 | |
GEE, generalized estimating equation; CI, confidence interval; SV, surgeon volume.
In the sensitivity analysis in which SV was represented by quartiles, we observed that the last SV quartile had an increased odds of surgical complications compared to lower SV quartile groups in the NIS sample. Compared to discharges with SV of 1–2 cases per year, discharges with SV 27–92 cases per year had a 142% increased odds of surgical complications (OR: 2.42; 95% CI: 1.47–3.97; P=0.001). The last SV quartile group also showed increased odds of surgical complications compared to SV of 3–7 cases per year (OR: 2.00; 95% CI: 1.20–3.31; P=0.007) and 8–26 cases per year (OR: 1.72; 95% CI: 1.00–2.94; P=0.049). In contrast, we did not observe any significant association of SV quartiles with surgical complications in the SID sample (P=0.50).
Discussion
This study examining 2,329 discharges is the first database analysis of the relationship between SV and complications in lateral neck dissection for thyroid and parathyroid malignancy. The NIS had an overall complication rate of 27.9%, which is higher than the 20.9% complication rate found in the SID cohort. When looking at these complications separately (Table 2), the rates in our analysis are comparable to what is found in the literature for total thyroidectomy. The NIS and SID had hematoma rates of 2.6% and 2.2% respectively, which are comparable to the hematoma rates of 0.2–2.7% reported in the literature (26-29). The NIS’s 2.1% wound infection rate was double what is reported in the literature at <1% (26-29), while the SID’s 1% wound infection rate falls in line with that reported trend. The NIS and SID had similar rates of vocal cord paralysis of 5% and 4.4%, respectively, which fall within the reported range of 0–15.4% (30). Finally, the rates of hypocalcemia are comparable to the literature’s reported rate of 5.8–20.5% (26), with a rate of 17.1% in the NIS and 12% in the SID.
When analyzing the raw data separated by SV quartile (Table 3), there are different patterns between the NIS and the SID. The last quartile of surgeons had the highest complication rate (37.1%) in the NIS cohort, while the first SV quartile had the highest complication rate (25%) in the SID cohort. This complication rate difference by SV quartile was only statistically significant in the NIS. Delving into the raw complication rates further by looking at each separate complication, there was only a significant difference between SV groups when assessing hypocalcemia in the NIS cohort, with the highest SV quartile demonstrating the highest rate for this complication. Within the SID, the rate of hypocalcemia by SV quartile did not differ significantly, with the first quartile for SV demonstrating the highest complication rate. We discuss below the differences in the NIS and SID cohorts that could lead to their disparate findings, however these opposite patterns were not expected. We suspect that the NIS analysis showing that higher volume surgeons had higher rates of hypocalcemia is secondary to a higher case complexity on average in patients operated on by high volume surgeons (e.g., higher volume of nodal disease or more aggressive thyroid cancer subtypes). There could also be differences in inpatient assessment of laboratory values by SV that could lead to a variance in coded complications that would be found in the discharge data analyzed [i.e., SV is associated with differences in rates of inpatient, post-operative calcium and parathyroid hormone (PTH) lab orders].
The range of SVs were similar in the two databases, with less of a positive skew in the SID cohort (Figures 1,2). Interestingly, of the 2,329 discharges for lateral neck dissection for endocrine malignancy, more than 500 involved a surgeon with a volume of one lateral neck dissection per year.
Adam et al. performed a similar analysis on the NIS for complications in thyroidectomy and an association with SV (8). Their analysis demonstrated a relatively simple pattern of decreasing complications with increasing SV up to 26 thyroidectomies per year, after which performing more thyroidectomies per year was not associated with a decreasing complication rate. Sharma et al. performed a different statistical analysis on a New York state database demonstrating high-volume lateral neck dissection surgeons being associated with a statistically lower rate of all-cause complications, but not a statistical difference in lateral neck specific complications (31). Our similarly performed multivariable analysis did not find so simple and predictable an outcome (see Table 5). After adjustment for confounders, only the NIS demonstrated a statistically significant relationship between SV and complications for patients undergoing lateral neck dissection for endocrine malignancy, with the SV group of 4–33 lateral neck dissections per year being associated with increasing complications with increasing volumes. This pattern of higher complication rates with increasing SV trends in the opposite direction of what is found in much of the literature for other surgical procedures (1-8). As mentioned above, this unexpected finding may be secondary to higher volume surgeons operating on patients with increased complexity, e.g., bulky disease, salvage after radiation, or a patient with poor nutritional status or history of tobacco use, etc.
The different results from NIS and SID are an important finding. We chose to include both the NIS and SID databases as there are important differences in their data collection, which caused us to question how that may or may not affect the patterns found on analysis. The NIS is a sample of discharges from hospitals in the United States (18,32), while the SID contains all the discharges from any payor to an acute care hospital within the particular state (17). Surgeons working multiple hospitals in the NIS will have separate identifiers. For this reason, and its sampling nature, the NIS may underestimate SV—our study demonstrated a median SV of only 5 in the NIS while the median was 21 for the SID. The SID contains all discharges within a state, and surgeons working multiple hospitals are tracked more accurately, but our 3-state analysis may not reflect the nation at large. The disparate results between the analyses may also be secondary to chronological difference—the NIS was studied from 2000 to 2009 while the SID from 2013 to 2014—or because the NIS includes data from states with a different demographic or surgeon population. It is also important to note that the Healthcare Utilization Project indicates that some states in the NIS do not provide physician numbers (used for tracking a surgeon). We excluded these states from our dataset, but this fact may call into question the quality of surgeon tracking within NIS generally (33). For this reason, we suggest caution before using results from these database analyses to suggest changes in clinical practice, particularly as it relates to SV (8). More research into understanding the appropriate and inappropriate questions to be addressed by these databases is warranted (33-35).
Despite this study’s large sample size and thorough analysis, it has constraints that are inherent to administrative databases. Complications that occurred after the inpatient encounter are not accounted for. Complications such as hypoparathyroidism and vocal cord paralysis may not be assessed for by every physician during the hospital stay, leaving the potential for an under-representation of the true complication rates. Levels of lateral neck dissections were not collected by these databases, nor type of thyroid cancer. It could be the case that higher SV does lead to decreased complication rates, but that higher volume surgeons in this sample were dissecting more levels within the neck, on average. Given that adding a neck dissection with a thyroidectomy remarkably increases the risk of complication (15), the inability to correct for this variable may have confounded our results, leading to the unexpected finding of SV having no association with complications or an inverse relationship (Table 5). The databases are unable to assess the adequacy of nodal and pathological clearance, as higher SV may be associated with a higher nodal yield—which was found to be the case in a single institution study for neck dissection for SCC (36). The coding used for the dataset did not categorize nerve injury into the possible nerves to be damaged in a neck dissection (spinal accessory, hypoglossal, phrenic, etc.), leaving us unable to further parse the data into this specific complication. Our analysis used any neck dissection for any pathology (SCC, papillary thyroid cancer, etc.) to calculate SV before applying this calculated value to the analysis of complications in neck dissection for thyroid cancer only. Given that ICD-9 codes don’t differentiate modified radical neck dissection from radical neck dissection, we could not separate modified radical neck dissection from radical neck dissection in the analysis, which could be a possible confounder for complication as that spinal accessory nerve preservations are not required for a radical neck dissection. Lastly, surgeon characteristics, such as specialty or years in practice, are unavailable in the databases. There may have been factors such as older surgeons with higher volumes in the past now performing fewer neck dissections but with decreased complication rates secondary to their prior experience, which could skew or confound the data. Such limitations add to the argument that these databases may be useful for their sample size and ease of access, but possibly inadequate for accurately assessing clinical relationships and hypotheses like the ones explored in this study.
Conclusions
This study—which was bolstered by two large sample sizes—demonstrated after adjustment that no SV and complication rate association was present in one cohort and an increasing odds of complication with increasing SV for intermediate volume surgeons was present in the other cohort. Such findings are unique from the more consistent, dose-dependent response of SV on decreasing complications in other surgical procedures (1-8). This difference may be due to the nuances of lateral neck dissection unable to be assessed using these databases and our methodology, or other etiologies, and merits further investigation. Given these disparate findings, we suggest caution in using administrative databases like NIS and SID in assessing these volume-outcome relationships.
Acknowledgments
Presented Orally: “Multi-Database Analysis of Neck Dissection Surgeon Volume and Complication Rates in Head and Neck Endocrine Malignancy”. American Academy of Otolaryngology—Head and Neck Surgery Foundation 2020 Annual Meeting & OTO Experience; 2020 September 13–16; Boston, MA. Submission # 2092.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-385/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-385/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-385/coif). TYC reports that she receives consulting fees from Cook Medical for lectures on implantable dopplers. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Duke University Health System Institutional Review Board assigned a human subjects research exemption. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sharkey PF, Shastri S, Teloken MA, et al. Relationship between surgical volume and early outcomes of total hip arthroplasty: do results continue to get better? J Arthroplasty 2004;19:694-9. [Crossref] [PubMed]
- Begg CB, Riedel ER, Bach PB, et al. Variations in morbidity after radical prostatectomy. N Engl J Med 2002;346:1138-44. [Crossref] [PubMed]
- Naso WB, Rhea AH, Poole A. Management and outcomes in a low-volume cerebral aneurysm practice. Neurosurgery 2001;48:91-9; discussion 99-100. [PubMed]
- Pearce WH, Parker MA, Feinglass J, et al. The importance of surgeon volume and training in outcomes for vascular surgical procedures. J Vasc Surg 1999;29:768-76; discussion 777-8. [Crossref] [PubMed]
- Wenner J, Zilling T, Bladström A, et al. The influence of surgical volume on hospital mortality and 5-year survival for carcinoma of the oesophagus and gastric cardia. Anticancer Res 2005;25:419-24. [PubMed]
- Rabeneck L, Davila JA, Thompson M, et al. Surgical volume and long-term survival following surgery for colorectal cancer in the Veterans Affairs Health-Care System. Am J Gastroenterol 2004;99:668-75. [Crossref] [PubMed]
- Nomura E, Tsukuma H, Ajiki W, et al. Population-based study of the relationship between hospital surgical volume and 10-year survival of breast cancer patients in Osaka, Japan. Cancer Sci 2006;97:618-22. [Crossref] [PubMed]
- Adam MA, Thomas S, Youngwirth L, et al. Is There a Minimum Number of Thyroidectomies a Surgeon Should Perform to Optimize Patient Outcomes? Ann Surg 2017;265:402-7. [Crossref] [PubMed]
- Machens A, Hinze R, Thomusch O, et al. Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg 2002;26:22-8. [Crossref] [PubMed]
- Kebebew E, Clark OH. Differentiated thyroid cancer: "complete" rational approach. World J Surg 2000;24:942-51. [Crossref] [PubMed]
- Sivanandan R, Soo KC. Pattern of cervical lymph node metastases from papillary carcinoma of the thyroid. Br J Surg 2001;88:1241-4. [Crossref] [PubMed]
- Cheah WK, Arici C, Ituarte PH, et al. Complications of neck dissection for thyroid cancer. World J Surg 2002;26:1013-6. [Crossref] [PubMed]
- Mann B, Buhr HJ. Lymph node dissection in patients with differentiated thyroid carcinoma–who benefits? Langenbeck's Archives of Surgery volume 1998;383:355-8.
- Cancer Facts & Figures 2020. American Cancer Society; 2020. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf
- Rocke DJ, Mulder H, Cyr D, et al. The effect of lateral neck dissection on complication rate for total thyroidectomy. Am J Otolaryngol 2020;41:102421. [Crossref] [PubMed]
- McMullen C, Rocke D, Freeman J. Complications of Bilateral Neck Dissection in Thyroid Cancer From a Single High-Volume Center. JAMA Otolaryngol Head Neck Surg 2017;143:376-81. [Crossref] [PubMed]
- HCUP State Inpatient Database (SID). 2014. Available online: http://www.hcup-us.ahrq.gov/sidoverview.jsp
- HCUP Nationwide Inpatient Sample (NIS). In: (HCUP) HCaUP, ed. Quality AfHRa, trans. Rockville, MD2011. Available online: https://hcup-us.ahrq.gov/news/exhibit_booth/HCUPFactSheet.pdf
- Konety BR, Dhawan V, Allareddy V, et al. Impact of hospital and surgeon volume on in-hospital mortality from radical cystectomy: data from the health care utilization project. J Urol 2005;173:1695-700. [Crossref] [PubMed]
- Chen K, Cheung K, Sosa JA. Surgeon volume trumps specialty: outcomes from 3596 pediatric cholecystectomies. J Pediatr Surg 2012;47:673-80. [Crossref] [PubMed]
- Nathan H, Cameron JL, Choti MA, et al. The volume-outcomes effect in hepato-pancreato-biliary surgery: hospital versus surgeon contributions and specificity of the relationship. J Am Coll Surg 2009;208:528-38. [Crossref] [PubMed]
- Paul JC, Lonner BS, Goz V, et al. Complication rates are reduced for revision adult spine deformity surgery among high-volume hospitals and surgeons. Spine J 2015;15:1963-72. [Crossref] [PubMed]
- Vogel TR, Dombrovskiy VY, Carson JL, et al. Lower extremity angioplasty: impact of practitioner specialty and volume on practice patterns and healthcare resource utilization. J Vasc Surg 2009;50:1320-4; discussion 1324-5. [Crossref] [PubMed]
- Thompson NR, Fan Y, Dalton JE, et al. A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Med Care 2015;53:374-9. [Crossref] [PubMed]
- Harrell F. Regression Modeling Strategies. 2 edition. Springer International Publishing; 2015.
- Christou N, Mathonnet M. Complications after total thyroidectomy. J Visc Surg 2013;150:249-56. [Crossref] [PubMed]
- Thomusch O, Machens A, Sekulla C, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg 2000;24:1335-41. [Crossref] [PubMed]
- Bellantone R, Lombardi CP, Bossola M, et al. Total thyroidectomy for management of benign thyroid disease: review of 526 cases. World J Surg 2002;26:1468-71. [Crossref] [PubMed]
- Efremidou EI, Papageorgiou MS, Liratzopoulos N, et al. The efficacy and safety of total thyroidectomy in the management of benign thyroid disease: a review of 932 cases. Can J Surg 2009;52:39-44. [PubMed]
- Rulli F, Ambrogi V, Dionigi G, et al. Meta-analysis of recurrent laryngeal nerve injury in thyroid surgery with or without intraoperative nerve monitoring. Acta Otorhinolaryngol Ital 2014;34:223-9. [PubMed]
- Sharma RK, Lee J, Liou R, et al. Optimal surgeon-volume threshold for neck dissections in the setting of primary thyroid malignancies. Surgery 2022;171:172-6. [Crossref] [PubMed]
- Overview of the National (Nationwide) Inpatient Sample (NIS). 2015. Available online: https://www.hcup-us.ahrq.gov/nisoverview.jsp#about
-
NIS Description of Data Elements - Kaiboriboon K, Schiltz N, Koroukian SM, et al. Limitations of NIS database in evaluation of epilepsy surgery morbidity and mortality. Arch Neurol 2011;68:1483-author reply 1483-4. [Crossref] [PubMed]
- Yoshihara H, Yoneoka D. Understanding the statistics and limitations of large database analyses. Spine (Phila Pa 1976) 2014;39:1311-2. [Crossref] [PubMed]
- Morton RP, Gray L, Tandon DA, et al. Efficacy of neck dissection: are surgical volumes important? Laryngoscope 2009;119:1147-52. [Crossref] [PubMed]


