
Boomerang latissimus dorsi flap in immediate or delayed breast reconstruction
Highlight box
Key findings
• Breast reconstruction using the boomerang latissimus dorsi flap may be a suitable alternative technique for patients who desire an autologous tissue transfer (rather than an implant) but are contraindicated for abdominal-based flaps and do not mind long postoperative scars.
What is known and what is new?
• Breast reconstruction using the latissimus dorsi flap is a popular breast reconstruction technique among Asian patients. The boomerang latissimus dorsi flap technique is an alternative to the conventional extended latissimus dorsi flap technique.
• Flap weight, operative time, mean admission duration, and drain indwelling duration were statistically higher in patients that underwent the boomerang latissimus dorsi flap technique.
What is the implication, and what should change now?
• The boomerang latissimus dorsi flap is a viable alternative to the latissimus dorsi flap with implant in some cases; however further work is needed to develop an optimal technique.
Introduction
Background
Breast reconstruction using the latissimus dorsi (LD) flap is one of the most popular breast reconstruction techniques and is the most commonly used technique for Asian patients, who often have small to moderate breast sizes. However, the Asian population has developed relatively larger breast volumes; as a result, there is a growing number of cases in which breasts need to be reconstructed to moderate to large sizes. Most reconstructive surgeons use abdominal-based flaps, such as the deep inferior epigastric perforator (DIEP) and transverse rectus abdominis myocutaneous (TRAM) or use the LD flap with an implant to supplement the volume with small implants. However, there has been a growing sentiment toward refusing implants since the recognition of breast implant-associated-anaplastic large cell lymphoma (BIA-ALCL) in 2019, and many patients prefer to avoid implantations of foreign bodies (silicone implants) during the process of breast reconstruction following surgical mastectomy for breast cancer. In addition, the demand for reconstruction of the removed breasts has been rising, given the increasing life expectancy of patients who prefer delayed breast reconstruction after receiving confirmation of oncological safety following radical mastectomy. There is thus an increasing need for autologous tissue reconstruction without using implants to minimize patient burden and distress.
Rationale and knowledge gap
As a result of evolving patient preferences and requirements along with higher education and social positions, patients’ needs regarding the esthetic aspects of their physiques and shapes are also increasing. In the past, the first objective of breast reconstruction was to achieve symmetry with the contralateral breast and to restore the preoperative breast. However, with an increasing rate of early diagnosis and treatment in recent years, a growing number of patients additionally desire to attain their preoperative breast shape and size through correction or aesthetic breast surgery (e.g., augmentation, reduction, mastopexy, fat injection). An increasing number of patients must undergo radical mastectomy for breast cancer and consider attaining aesthetic outcomes through breast augmentation or lifting through mastopexy or breast reduction as a positive gain, instead of aiming to simply restore their breasts to preoperative states. The ability to comprehensively address these needs and provide patients with an opportunity to select from various techniques may boost the satisfaction of both surgeons and patients.
Objective
In this study, we aimed to report the usefulness of the boomerang LD (bLD) flap, a technique developed by modifying the design of the conventional extended LD flap, compared with the extended LD flap with implant (LDi) technique for patients with moderate to large breasts who require radical mastectomy or who had a radical mastectomy and wish to avoid a second stage surgery with tissue expander as well as an implant, patients who refuse the abdominal-based flap due to a history of abdominal surgery or severe concerns for long operation (OP) time or complications, young patients who have small to moderate breast volume and slim body shape [low body mass index (BMI)] but are contraindicated for an abdominal-based flap due to pregnancy considerations in the future, and patients who prefer an autologous tissue and are reluctant to use an implant but do not mind long scars. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-664/rc).
Methods
Study design
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Kyungpook National University Chilgok Hospital (No. 2021-08-001), and all patients provided informed consent to have their data (including de-identified photographs) recorded, analyzed, and published for research purposes.
Of 85 patients, 63 were assigned to the group undergoing immediate or delayed breast reconstruction using the LDi flap, and 25 were assigned to the group undergoing immediate or delayed breast reconstruction using the bLD flap. The corresponding surgeries were conducted between May 2014 and April 2022. Patient characteristics included age, BMI, preoperative breast volume, specimen weight, cancer staging, radiotherapy, chemotherapy, flap weight, total OP time, flap elevation time, negative drain indwelling duration, and total drain volume. Patient photometry follow-up was conducted using pre-, intra-, and postoperative month (POM)1, POM3, and POM6. Total OP time was defined as the time from patient entry to leaving time registered in an electronic medical record (EMR). Flap elevation time was calculated between intraoperative flap design and elevated flap photo time. Major complications such as hematoma, seroma, flap loss, and necrosis, and minor complications including dehiscence, swelling, and sloughing were recorded.
Patient selection
This was a prospective cohort study. Patient inclusion criteria were as follows: breast cancer patients between the age of 25 and 60 years undergoing unilateral total or skin/nipple-sparing mastectomy (NSM), as well as postmastectomy. The following patients were excluded from the study: (I) advanced breast cancer (stages 3 and 4) patients, (II) patients with a history of cognitive impairment who could not complete the self-reported questionnaire, (III) patients with a history of any neurologic and musculoskeletal disorder, and (IV) patients with a history of alcohol or drug abuse.
We adequately explained the consequent long donor-site scar and potential complications, and we obtained informed consent from patients with moderate to large breasts. We excluded patients who refused implants, thin patients for whom an implant could not be used due to small breast size, and those who only desired an autologous tissue transfer. If the breast volume was insufficient even after the flap reconstruction, we focused on maintaining symmetry with the contralateral breast by performing reduction of the contralateral breast or augmentation, should the patient desire.
Statistical analysis
Statistical analysis was conducted by means of regression analysis using SPSS software (SPSS 22.0, IBM, Armonk, NY, USA). The correlations between OP time, flap elevation time, admission duration, adjuvant treatment (radiotherapy, chemotherapy) drain indwelling duration, and drain total sum volume according to the two technique types (LDi vs. bLD), age, BMI, and breast preoperative volume were analyzed.
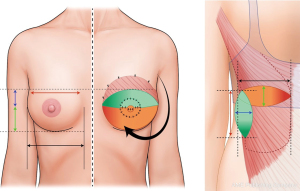
Preoperative design of bLD flap
The patient was asked to stand in an upright position wearing a bra, and the ipsilateral margin was marked. After removing the bra, the breast surgeon determined the incision line in consideration of the breast skin or nipple-areolar complex (NAC) excision. Then, the breast width, height, and projection were measured. To ensure that the transverse scar was hidden along the bra line, an ellipse with a length of 2 cm greater than the breast width length was designed. We checked the area hidden by the patient’s arm when standing upright with arms relaxed on the sides, and a vertical ellipse was designed with half of the length of the upper pole of the breast such that the vertical scar occurred at the midpoint of the covered area. We designed the ellipses such that the sum of the width of the transverse ellipse and width of the vertical ellipse was equal to the breast height. For patients undergoing delayed breast reconstruction, the bLD flap was designed with reference to the contralateral breast profile, and we obtained consent for performance of concurrent mastopexy of the contralateral breast (if the patient wished) or concurrent reduction of the contralateral breast if breast volumes were asymmetrical even after bLD flap. If the NAC had to be excised, we performed simultaneous nipple reconstruction (SNR) to enhance patient satisfaction (Figure 1).
bLD flap technique in total breast reconstruction (Video 1)
After total mastectomy (TM) by the breast surgery team, the patient was moved to the decubitus position, and the drape was carefully conducted to maintain the preoperative design. The length of the transverse flap was designed to be 2 cm larger than the patient’s breast width, and the length of the vertical flap was designed to be about half of the width from the breast upper pole. One important aspect is to perform a pinch test to prevent postoperative complications in the donor site because the overlap between the transverse flap and vertical flap is the area with the highest tension when suturing the donor site. After designing the flaps, 1:10,000 lidocaine with epinephrine was injected subcutaneously in all bLD flap margins (20 cc), and an incision was made with a No. 10 blade. Hemostasis and dissection were performed using the Bovie device (Bovie® Medical Corporation, Clearwater, FL, USA). Subcutaneous undermining was performed toward the axillar area and then in the order of the anterior margin and lower margin. The inferior aspect of the LD muscle was cut using the LigaSure device (LigaSure™, Minneapolis, MN, USA). Then, the medical margin was followed up to elevate the bLD flap, and once the axillary area was reached, dissection was performed while carefully avoiding injury of the main pedicle, the thoracodorsal artery, and the vein. Because volume is secured in general, the flaps were cut such that complications, such as postoperative jerking movement, were prevented with the thoracodorsal nerve. After the bLD flap was fully elevated, the flap was weighed on a spring balance to compare with the weight of the breast specimen. Then, the bLD flap was shaped into that of the reconstructed breast. De-epithelization was performed for NSM after sparing skin needed to perform SNR for TM. In the distal part of the vertical flap, the subcutaneous fat and LD muscle were separated and sutured with 2-0 vicryl, such that the tip of the vertical flap touched the tip of the transverse flap. A subcutaneous suture was performed at the subcutaneous level, and the dermis was continuously sutured using 2-0 vicryl to minimize disruption during transfer due to breast defects. The area to be placed at the lower margin of the reconstructed breast was trimmed into a round shape, and the point of contact between the vertical flap and LD muscle was sutured with 2-0 vicryl to reduce gaps in the level, ensuring the natural appearance of the reconstructed breast upper pole. After shaping the flap into the appropriate shape, it was transferred to the breast. Massive irrigation and bleeding control were performed, and two lines of a negative drain (800 cc) were applied. To minimize seroma formation, quilting sutures were performed at four to five sites with 2-0 vicryl, and the donor site was sutured layer-by-layer, using 0, 2-0, or 4-0 vicryl or 5-0 prolene, depending on the tension. Then, the patient was moved back to the supine position, and the muscles of the bLD flap were sutured into the upper margin of the breast using 2-0 vicryl. The flap was arranged in a round shape, aligning with the breast, and was trimmed to achieve symmetry. One line of a negative drain (400 cc) was applied to the upper and lower parts, and 4 cc of fibrin glue was sprayed, followed by suturing to conclude the surgery.
If the breast skin was excised, the skin of the bLD flap was placed appropriately to cover the excised area. If the NAC area was partially or totally excised, SNR was performed to achieve maximal reconstruction in one surgery. If performed in two stages, the surgeries were performed concurrently in consideration of the advantage of minimizing distortions of breast shape.
Results
A total of 88 patients, including 63 and 25 patients who underwent immediate breast construction through LDi and bLD, respectively, after TM from January 2015 to June 2022, were analyzed. The mean ages of patients in the LDi and bLD groups were 46±7.7 and 45.6±7.8 years, respectively. BMI was 23.8±3.4 in the LDi group and 23.7±4.2 in the bLD group. Additionally, 33 (52.4%), 25 (39.7%), 2 (3.2%), 2 (3.2%), and 1 (1.6%) patients in the LDi group were diagnosed with IDC, DCIS, and ILC, mucinous carcinoma, and phyllodes tumor, respectively, while 12 (48.0%), 11 (44.0%), and 2 (8.0%) patients in the bLD group were diagnosed with IDC, DCIS, and ILC, respectively.
Preoperative breast volume was 367.9±148.1 cc in the LDi group and 324.1±135.2 cc in the bLD group. Specimen and flap weight were 449.6±170.9 g/354.2±120.1 g in the LDi group and 468.3±233.5 g/444.4±101.0 g in the bLD group, respectively (flap weight, P<0.05). For axillary surgery, sentinel lymph node biopsy (SLNB) was conducted in 54 (85.7%) patients of the LDi flap group and 20 (80%) patients of the bLD flap group, and axillary lymph node dissection (ALND) was conducted in 9 (14.3%) patients of the LDi group and 5 (20.0%) patients of the bLD group. The total mean OP time was 429.0±104.1 min in the LDi group and 368.0±82.3 min in the bLD group. Flap elevation time was 263.6±83.3 min in the LDi group and 255.7±85.7 min in the bLD group. Mean admission duration was 17.3±3.5 and 13.3±3.6 days in the LDi flap and bLD groups, respectively (P<0.001). Mean donor site drain indwelling duration was 14.3±3.5 days in the LDi group and 10.0±3.3 days in the bLD group; patients underwent drain removal (P<0.001) when subsequent daily drain measurements were <20 cc. Drain total volume was 1,163.2±413.1 cc and 1,237.8±799.8 cc in the LDi and bLD groups, respectively (Table 1). In the bLD flap group, flap weight, OP time, admission duration, and drain indwelling duration were statistically significant (P<0.05) (Table 1).
Table 1
| Characteristics | LDi (n=63) | bLD (n=25) | P value |
|---|---|---|---|
| Age (years), mean ± SD | 46±7.7 | 45.6±7.8 | 0.9097 |
| BMI (kg/m2), mean ± SD | 23.8±3.4 | 23.7±4.2 | 0.9417 |
| Diagnosis, n (%) | |||
| IDC | 33 (52.4) | 12 (48.0) | |
| DCIS | 25 (39.7) | 11 (44.0) | |
| ILC | 2 (3.2) | 2 (8.0) | |
| Mucinous carcinoma | 2 (3.2) | – | |
| Phyllodes tumor | 1 (1.7) | – | |
| Breast volume (cc), mean ± SD | 367.9±148.1 | 324.1±135.2 | 0.2274 |
| Specimen weight (g), mean ± SD | 449.6±170.9 | 468.3±233.5 | 0.6993 |
| Flap weight (g), mean ± SD | 354.2±120.1 | 444.4±101.0 | 0.0072 |
| Axillar surgery, n (%) | |||
| SLNB | 54 (85.7) | 20 (80.0) | |
| ALND | 9 (14.3) | 5 (20.0) | |
| Total OP time (min), mean ± SD | 429.0±104.1 | 368.0±82.3 | 0.0126 |
| Flap elevation time (min), mean ± SD | 263.6±83.3 | 255.7±85.7 | 0.6988 |
| Admission duration (days), mean ± SD | 17.3±3.5 | 13.3±3.6 | <0.001 |
| Drain indwelling duration (days), mean ± SD | 14.3±3.5 | 10.0±3.3 | <0.001 |
| Drain total volume (cc), mean ± SD | 1,163.2±413.1 | 1,237.8±799.8 | 0.6066 |
LD, latissimus dorsi; LDi, LD flap with implant; bLD, boomerang LD flap; SD, standard deviation; BMI, body mass index; IDC, invasive ductal carcinoma; DCIS, ductal carcinoma in situ; ILC, invasive lobular carcinoma; SLNB, sentinel lymph node biopsy; ALND, axillary lymph node dissection; OP, operation.
The mean follow-up period was 17 and 7.2 months in the LDi and bLD groups, respectively. Regarding postoperative complications, 4 patients in the LDi group and 1 patient in the bLD group had persistent seroma (≥1 month) that was treated by aspiration and was healed at 3 months. Major seromas that persisted for ≥6 months were treated by donor site re-operation in consultation with the patient (2 in the LDi group and 1 in the bLD group), after which it healed. Infection occurred in 1 patient in the LDi group (donor site) and 2 patients in the bLD group (1 at the donor site and 1 at the breast site). Partial NAC necrosis occurred in 5 patients in the LDi group and 2 patients in the bLD group, and total necrosis occurred in 2 patients in each group. Capsular contracture occurred only in 5 patients (7.9%) in the LDi group that used an implant (mild to severe). Hematoma occurred in 2 patients (1 in the donor site and 1 in the breast site) in the LDi group and 1 in the bLD group (breast site) (Table 2).
Table 2
| Category | LDi (n=63) | bLD (n=25) |
|---|---|---|
| Seroma, n (%) | ||
| Minor | 4 (6.3) | 1 (4.0) |
| Major | 2 (3.2) | 1 (4.0) |
| Infection, n (%) | 1 (1.6) | 2 (8.0) |
| NAC necrosis (partial/total), n (%) | 5 (7.9)/3 (4.8) | 2 (8.0)/2 (8.0) |
| Capsular contracture, n (%) | 5 (7.9) | _ |
| Hematoma, n (%) | 2 (3.2) | 1 (4.0) |
LD, latissimus dorsi; LDi, LD flap with implant; bLD, boomerang LD flap; NAC, nipple-areolar complex.
Discussion
Since establishing that immediate breast reconstruction is oncologically safe for breast cancer, breast reconstruction has become an essential procedure following mastectomy. A number of breast reconstruction surgical techniques have been reported, including autologous tissue transfer, allograft, or a combination of both. Currently, breast reconstruction using the abdominal-based DIEP flap is considered the ideal technique to restore the texture and shape of native breasts (1,2). As an alternative, the pedicled extended LD flap, introduced in the 1970s, can be used without microsurgery and produces reliable outcomes without causing pathologic problems for shoulder function or skeletal posture (3-7). However, westernized diets have led to increasingly westernized body physiques among Asians, along with larger breasts, and as a result, there are cases in which the desired breast volume cannot be achieved solely with the extended LD flap. In such cases, a small implant is placed under the LD flap, such that the LD flap placed immediately under the breast skin flap produces a natural-shaped reconstructed breast while the small implant ensures adequate volume (8). However, foreign body reactions are inevitable around silicone implants, and reoperations are occasionally required due to severe capsular contractures. Further, in response to the recent report of BIA-ALCL that is speculated to be linked to texture implants, although only a small number of cases have been reported, textured implants have been pulled from the market in many countries, leaving only smooth implants as the remaining option. In this context, patients who undergo breast reconstruction after being diagnosed with breast cancer have become reluctant to undergo implantation of foreign bodies and prefer autologous tissue transfers, in addition to preferring surgical approaches that best prevent the recurrence of breast cancer rather than focusing on minimizing the postoperative scar. Fat grafting onto the LD flap can be performed in place of an implant to supplement the inadequate volume. Multilayer fat grafting on the LD muscle did not lead to flap loss or seroma formation (9-13). However, although this method can help increase volume, fat graft survival can be inconsistent. Hence, rich experience is essential, and outcomes can vary depending on the specific situation.
Moreover, the age of patients at diagnosis is declining amid advances in diagnostic tools, which means that future pregnancies should be taken into consideration. In such cases, breast reconstruction using the abdominal-based flap may be contraindicated. In addition, this flap may not be the first choice for patients with a history of abdominal surgery due to the possibility of pedicle injury. From the perspective of the reconstructive surgeon, microsurgery can be challenging for non-expert surgeons, so if other pedicled flap techniques are available, the specific technique should be chosen based on a thorough discussion with the patient, followed by deliberation. In this context, we designed a boomerang-shaped flap by integrating the transverse extended LD flap design and vertical LD flap design used in partial breast reconstruction. In this article, we reported good outcomes of breast reconstruction using the bLD flap in patients who required radical mastectomy or had modified radical mastectomy due to breast cancer and were contraindicated for abdominal-based flaps, such as the DIEP flap. Baumholtz et al. introduced breast reconstruction using the boomerang flap, and although the basic concepts were similar, they introduced a flap design in which the vertical flap was close to the vertebra, unlike that in our study (14). In the present study, we placed the vertical flap on the midaxillary line, not only to hide the scar beneath the arm but also to minimize the possibility of distal flap fat necrosis that can be caused by placing the flap too far from the pedicle proximal; furthermore, the vertical LD flap has been established to produce good outcomes in partial breast reconstruction (Figure 1) (15,16).
LDi is a highly useful surgical technique with a low complication rate, even with adjuvant radiotherapy, and good long-term outcomes (Figure 2) (17-19). However, the technique involves a silicone implant, which leaves the risk for implant-related complications, such as capsular contracture, BIA-ALCL, and foreign body reactions (Figure 3). The major indications for the bLD flap include strong refusal of implants and fear of potential complications of abdominal-based flaps (e.g., herniation, scarring, microsurgery, extensive OP time). The methods for delayed breast reconstruction can be broadly divided into single-stage surgery using standard techniques (DIEP, TRAM) or LDi (20) and two-stage surgery, in which the skin envelope is widened with a tissue expander and later replaced with an implant. However, the use of bLD has proven to be very useful for patients with small to moderate-sized breasts (Figures 4-7).






Statistical analyses confirmed that bLD flaps are heavier than LDi flaps and were associated with significantly shorter total OP time, length of hospital stay, and drain indwelling duration (Table 1). The greater weight is due to the larger skin flap design, indicating a substantial amount of autologous tissue being transferred. We speculate that the surgery using the LDi flap is longer due to the time required to select and prepare the implant and the additional time needed to insert the flap below the LD for appropriate positioning and shaping. In addition, patients who underwent bLD reconstruction had a shorter length of stay, presumably because while patients stay in the hospital until the drains are removed, the bLD flap requires a longer and larger donor site incision involving an overlap between the transverse and vertical flap designs that are pulled in the opposite directions during closure. This reduces the risk of creating a dead space in the donor site, even if the bLD flap is transferred. Furthermore, an implant is generally not used for patients who are likely to proceed to adjuvant radiotherapy following surgery, as it is difficult to predict and may be difficult to resolve foreign body-related complications. For these reasons, autologous tissues are preferred for patients who are likely to undergo radiotherapy, and this possibly contributed to the significantly higher rate of postoperative radiotherapy in the bLD patient group. Regarding postoperative complications, no severe complications occurred in either group. However, about 7.9% of the patients in the LDi group had capsular contracture (mild to severe), highlighting the importance of implant placement as well as the thickness and volume of LD muscle that covers the implant (Table 2).
However, bLD is not a viable alternative to LDi in all cases. LDi is the ideal technique with reliable outcomes and low complication risk for patients with large breasts, patients who refuse reduction or mastopexy of the contralateral breast, patients who refuse abdominal-based flap operation, and patients contraindicated for abdominal-based flap operation due to surgical history. Furthermore, the DIEP or TRAM flap or two-stage operation (tissue expander, implant) are good surgical techniques available for delayed reconstruction.
Conclusions
Breast reconstruction using the bLD flap is a good alternative technique for patients who desire an autologous tissue transfer rather than an implant but are contraindicated for the abdominal-based flap and do not mind long postoperative scars.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-664/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-664/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-664/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-664/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved the by Institutional Review Board of Kyungpook National University Chilgok Hospital (No. 2021-08-001), and all patients provided informed consent to have their data (including de-identified photographs) recorded, analyzed, and published for research purposes.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Granzow JW, Levine JL, Chiu ES, et al. Breast reconstruction using perforator flaps. J Surg Oncol 2006;94:441-54. [Crossref] [PubMed]
- Santanelli F, Longo B, Angelini M, et al. Prospective computerized analyses of sensibility in breast reconstruction with non-reinnervated DIEP flap. Plast Reconstr Surg 2011;127:1790-5. [Crossref] [PubMed]
- Schneider WJ, Hill HL Jr, Brown RG. Latissimus dorsi myocutaneous flap for breast reconstruction. Br J Plast Surg 1977;30:277-81. [Crossref] [PubMed]
- Santanelli F, Longo B, Cagli B, et al. Predictive and protective factors for partial necrosis in DIEP flap breast reconstruction: does nulliparity bias flap viability? Ann Plast Surg 2015;74:47-51. [Crossref] [PubMed]
- Olivari N. The latissimus flap. Br J Plast Surg 1976;29:126-8. [Crossref] [PubMed]
- Lee JS, Park E, Lee JH, et al. Alteration in skeletal posture between breast reconstruction with latissimus dorsi flap and mastectomy: a prospective comparison study. Gland Surg 2021;10:1587-97. [Crossref] [PubMed]
- Yang JD, Huh JS, Min YS, et al. Physical and Functional Ability Recovery Patterns and Quality of Life after Immediate Autologous Latissimus Dorsi Breast Reconstruction: A 1-Year Prospective Observational Study. Plast Reconstr Surg 2015;136:1146-54. [Crossref] [PubMed]
- Ishii N, Ando J, Shimizu Y, et al. A novel technique for large and ptotic breast reconstruction using a latissimus dorsi myocutaneous flap set at the posterior aspect, combined with a silicone implant, following tissue expander surgery. Arch Plast Surg 2018;45:484-9. [Crossref] [PubMed]
- Zhu L, Mohan AT, Vijayasekaran A, et al. Maximizing the Volume of Latissimus Dorsi Flap in Autologous Breast Reconstruction with Simultaneous Multisite Fat Grafting. Aesthet Surg J 2016;36:169-78. [Crossref] [PubMed]
- Santanelli di Pompeo F, Laporta R, Sorotos M, et al. Latissimus dorsi flap for total autologous immediate breast reconstruction without implants. Plast Reconstr Surg 2014;134:871e-9e. [Crossref] [PubMed]
- Johns N, Fairbairn N, Trail M, et al. Autologous breast reconstruction using the immediately lipofilled extended latissimus dorsi flap. J Plast Reconstr Aesthet Surg 2018;71:201-8. [Crossref] [PubMed]
- Demiri EC, Dionyssiou DD, Tsimponis A, et al. Outcomes of Fat-Augmented Latissimus Dorsi (FALD) Flap Versus Implant-Based Latissimus Dorsi Flap for Delayed Post-radiation Breast Reconstruction. Aesthetic Plast Surg 2018;42:692-701. [Crossref] [PubMed]
- Palve J, Luukkaala T, Kääriäinen M. Comparison of Different Techniques in Latissimus Dorsi Breast Reconstruction: Plain, Immediately Lipofilled, and Implant Enhanced. Ann Plast Surg 2022;88:20-4. [Crossref] [PubMed]
- Baumholtz MA, Al-Shunnar BM, Dabb RW. Boomerang flap reconstruction for the breast. Ann Plast Surg 2002;49:44-8; discussion 48-9. [Crossref] [PubMed]
- Kang MJ, Park TH, Ryu JY, et al. Boomerang latissimus dorsi flap in total breast reconstruction: report of three cases. Gland Surg 2022;11:290-9. [Crossref] [PubMed]
- Lee JH, Ryu JY, Choi KY, et al. Useful vertical latissimus dorsi flap for partial breast reconstruction in every tumor location. BMC Surg 2022;22:294. [Crossref] [PubMed]
- Mushin OP, Myers PL, Langstein HN. Indications and Controversies for Complete and Implant-Enhanced Latissimus Dorsi Breast Reconstructions. Clin Plast Surg 2018;45:75-81. [Crossref] [PubMed]
- Garusi C, Lohsiriwat V, Brenelli F, et al. The value of latissimus dorsi flap with implant reconstruction for total mastectomy after conservative breast cancer surgery recurrence. Breast 2011;20:141-4. [Crossref] [PubMed]
- Chang DW, Barnea Y, Robb GL. Effects of an autologous flap combined with an implant for breast reconstruction: an evaluation of 1000 consecutive reconstructions of previously irradiated breasts. Plast Reconstr Surg 2008;122:356-62. [Crossref] [PubMed]
- Agaoglu G, Erol OO. Delayed breast reconstruction with latissimus dorsi flap. Aesthetic Plast Surg 2009;33:413-20. [Crossref] [PubMed]


