
Malignancy risk in Bethesda class IV thyroid nodules in an iodine deficient region
Highlight box
Key findings
• Increasing size correlated with an increasing malignancy rate (P<0.01), and follicular carcinomas were found to be larger than papillary carcinomas (P<0.001).
What is known and what is new?
• In patients with Bethesda IV thyroid nodules, diagnostic lobectomy should be the preferable surgical approach in absence of factors that suggest total thyroidectomy. In our opinion, total thyroidectomy remains the first choice in large nodules (≥4 cm) as these nodules have a high malignancy rate, greater local/lymphovascular invasion and a consequent frequent indication for post-operative radiometabolic treatment.
What is the implication, and what should change now?
• An accurate preoperative study is essential to decide, in accordance with the patient, the best surgical approach.
Introduction
Thyroid cancer is the most frequent neoplasm of the endocrine system and accounts for approximately 3.8% of all neoplasms (1).
It is well established that iodine is essential for thyroid homeostasis. In addition to the known effects on glandular function, chronic iodine deficiency can favor the development of goiter or an increase in the incidence and prevalence of benign nodularities (2). The relationship with thyroid cancer remains controversial and the different studies that have investigated this correlation are not in agreement. A study has shown an increased risk of developing thyroid carcinoma in populations living in iodic-deficient areas, with a higher prevalence of follicular carcinoma (3).
American Thyroid Association (ATA) and most European guidelines consider cytological examination by needle aspiration the gold standard for the evaluation and management of thyroid nodular pathology (1,4,5).
For thyroid nodules cytological evaluation, the Bethesda System for Reporting Thyroid Cytopathology (BSRTC) is one of the most used classifications. The BSRTC defines six diagnostic categories with increasing suspicious characteristics for malignancy: nondiagnostic (Class I), benign (Class II), atypia of indeterminate meaning/follicular lesion of indeterminate meaning (Class III), follicular neoplasm/Oxifilics neoplasm (Class IV), suspicious for malignancy (Class V), malignant (Class VI) (6).
The lesions included in Bethesda class IV are characterized by high cellularity, poor or absent colloid and absolute prevalence of microfollicular/trabecular structures, with characteristics suggestive of “follicular neoplasia”. Lesions with some nuclear alterations suggestive of papillary carcinoma but too mild or focal to include them in the category V are also included in this category.
The 2015 ATA guidelines suggest the following surgical management for nodules with indeterminate cytology:
- In patients with solitary indeterminate nodule candidated for surgery, thyroid lobectomy is the initial recommended surgical approach. This approach can be modified according to clinical or ultrasound nodule characteristics, patient’s preferences, or molecular test outcomes.
- In patients with cytologically indeterminate nodules suspicious for malignancy, with a positive finding for specific mutations for carcinoma, with suspicious ultrasound patterns, with size greater than 4 cm, or in patients with familial thyroid cancer or a history of radiation exposure, total thyroidectomy should be preferred.
- In patients with bilateral nodules, with important comorbidities or in case the patient prefers to undergo total thyroidectomy, to avoid the possibility of further surgery on the contralateral lobe, total thyroidectomy is indicated (4).
Total thyroidectomy is a more riskful procedure than thyroid lobectomy and has a higher complication rate. A recent meta-analysis describes a higher relative risk (RR) of major complications: recurrent laryngeal nerve injury (transient RR =1.7, permanent RR =1.9), hypocalcemia (transient RR =10.7, permanent RR =3.2) and haemorrhage/hematoma (RR =2.6) (7).
According to most guidelines the possible risks and benefits of the various surgical procedures must be exposed to the patient to decide the best therapeutic option (1,4).
The main aim of our study is the evaluation of the cases that underwent surgery for Bethesda class IV nodules in an iodocarent geographical area, such as the province of Parma, with particular attention to: carcinoma incidence, preoperative nodule size, histological characteristics of the neoplasm, surgical approach and eventual need of radiometabolic treatment. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-491/rc).
Methods
This retrospective observational study has as its main aim the evaluation of the cases that underwent surgery, for Bethesda class IV nodules in our iodocarent geographical area. Particular attention was paid to: carcinoma incidence, preoperative nodule size, histological characteristics of the neoplasm, surgical approach and eventual need of radiometabolic treatment.
We analyzed data of patients that underwent thyroid surgery for nodules with high-risk indeterminate cytology, Bethesda class IV, in the period between January 2010 and December 2020 at the Operative Unit of the General Surgical Clinic of the University Hospital of Parma, Italy.
Exclusion criteria were: preoperative evidence of malignancy; missing essential clinical data; residence in a non-iodine-deficient region.
We analyzed the following variables: age; gender; date of surgery (pre/post introduction of ATA 2015 guidelines); type of surgery (lobectomy vs. total thyroidectomy); possible need for thyroid totalization surgery; cytological diagnosis: Bethesda class IV (TIR 3B cases according to SIAPEC-IAP, Italian Society for Anatomic Pathology joint with the Italian Division of the International Academy of Pathology, have been reclassified as class IV according to Bethesda System 2017); nodule size found during preoperative investigations; multinodularity; presence of bilateral nodules; postoperative histological report; postoperative size of the nodules that resulted carcinoma; histopathological characteristics (local or vascular invasion, multifocality, lymph node metastasis); eventual execution of radioiodiometabolic therapy.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of University Hospital of Parma (No. 84/2022/OSS*/AOUPR), and informed consent was taken from all individual participants.
Statistical analysis
Data analysis was performed with the Jamovi v. Statistical package. 2.0 [The jamovi project (2021). Jamovi. (Version 2.0) (Computer Software). Retrieved from https://www.jamovi.org].
For the descriptive analysis of the continuous variables, main position, dispersion, and shape indices were calculated, including mean, median, mode, trimmed mean at 5%, variance, standard deviation, interquartile difference, minimum, maximum. Where relevant, standard errors and related 95% confidence intervals have also been reported. Qualitative characters were reported in frequency tables and expressed as absolute frequencies, relative frequencies, and percentages. Fisher’s exact test and Pearson’s Chi-square test were used for categorical variables. Cramer’s V Index was used to evaluate the association between the variables. Other analyzes were performed considering nodule size as a continuous variable. We used Student’s t-test, Welch’s test, Mann-Whitney’s U-test, analysis of variance (ANOVA), and Kruskal-Wallis test. We used Fisher, Pearson’s Chi-Square test and binary logistic regression to evaluate the association between preoperative nodule size and malignancy rate, and to evaluate the association between nodule size and local/lymphovascular invasion, multifolocality or presence of lymph node metastases. For both continuous and categorical mutable variables, P values lower than 5% (P<0.05) were considered statistically significant.
Results
In this study we included 320 patients. In our sample we found 244 females (76%) and 76 males (24%), with an average age of 53.1±13.8 years (range, 19–83 years). Considering 55 years as age cut off, 152 patients (47.5%) were older than 55 years and 168 patients (52.5%) were younger.
Preoperative study localized nodules in the right thyroid lobe in 165 cases (51.6%), in the left one in 136 cases (42.5%), in the isthmus in 14 cases (4.4%), bilaterally in 5 cases (1.5%).
Mean preoperative nodules size was 19.1 mm, with a maximum of 80 mm and a minimum of 6 mm. In 59 cases (18.4%) we found nodules smaller or equal to 1 cm, while in 22 cases (6.9%) we found nodules larger or equal to 4 cm. 239 nodules (74.7%) resulted to be between 1 and 4 cm (Figure 1).

For the treatment of these nodules, 230 total thyroidectomies were performed (71.9%), 188 with the traditional technique and 42 with minimally invasive video-assisted thyroidectomy (MIVAT), and 90 hemithyroidectomies (28.1%), 52 with the traditional technique and 38 with minimally invasive video-assisted thyroidectomy (MIVAT). In 15 of the patients who underwent lobectomy (16.6% of all lobectomies performed) a totalization of thyroidectomy was required. From this analysis it emerged that in general a more demolitive surgical approach was preferred over a conservative one.
We analyzed the impact of guideline changes on the surgical approach, evaluating separately surgeries performed before and after 2015, the year of publication of the latest ATA guidelines.
From 2010 to 2015, 125 surgical procedures were performed: 116 (92.8%) total thyroidectomies and 9 lobectomies (7.2%). From 2016 to 2020, 195 surgical procedures were performed: 114 (58.5%) total thyroidectomies and 81 lobectomies (41.5%). From our data analysis, we found an increased rate of lobectomies in the period after 2015, with a statistically significant difference (P<0.001) (Table 1).
Table 1
| Surgeries before or after 2015 | Total thyroidectomy, n (%) | Lobectomy, n (%) | Total |
|---|---|---|---|
| Before 2015 | 116 (92.8) | 9 (7.2) | 125 |
| After 2015 | 114 (58.5) | 81 (41.5) | 195 |
| Total | 230 (71.9) | 90 (28.1) | 320 |
We assessed the presence or absence of bilateral nodules emerged during preoperative study. Bilateral nodules were found in 127 patients (39.7%), while in 193 patients (60.3%) there weren’t bilateral nodules. We therefore analyzed the type of surgical procedure in patients with or without bilateral nodules. In patient with bilateral nodules, 113 total thyroidectomies (89%) and 14 lobectomies (11%) were performed; in the absence of bilateral nodules, 117 total thyroidectomies (60.6%) and 76 lobectomies (39.4%) were performed. We found a statistically significant correlation between the presence or absence of bilateral nodules and the type of surgical procedure performed, with a significant increase of hemithyroidectomies in absence of bilateral thyroid nodules (P<0.001). Also in this case, we evaluated the surgical procedures performed before and after 2015, year of publication of the latest ATA guidelines. From 2010 to 2015, in presence of bilateral nodules, 52 total thyroidectomies (100%) and 0 lobectomies (0%) were performed; in the absence of bilateral nodules, on the other hand, 64 total thyroidectomies (87.7%) and 9 lobectomies (12.3%) were performed.
From 2016 to 2020, in presence of bilateral nodules, 61 total thyroidectomies (81.3%) and 14 lobectomies (18.7%) were performed; while in absence of bilateral nodules, 53 total thyroidectomies (44.2%) and 67 lobectomies (55.8%) were performed. Also in this case we found an increase of lobectomies in the period after 2015, with a statistically significant difference (P<0.001) (Table 2).
Table 2
| Surgeries before-after 2015 | Bilateral nodules | Total thyroidectomy, n (%) | Lobectomy, n (%) | Total |
|---|---|---|---|---|
| Before 2015 | No | 64 (87.7) | 9 (12.3) | 73 |
| Yes | 52 (100.0) | 0 (0.0) | 52 | |
| After 2015 | No | 53 (44.2) | 67 (55.8) | 120 |
| Yes | 61 (81.3) | 14 (18.7) | 75 | |
| Total | No | 117 (60.6) | 76 (39.4) | 193 |
| Yes | 113 (89.0) | 14 (11.0) | 127 |
The presence of single or multiple nodularities was also evaluated, regardless of bilateralism. Multiple nodularities emerged in 182 cases (56.9%), single nodularities in 138 cases (43.1%).
The postoperative histological diagnoses were divided into six groups (Table 3).
Table 3
| Preoperative diagnosis | N (%) |
|---|---|
| Benign neoplasm | 191 (59.7) |
| Papillary carcinoma | 71 (22.2) |
| Follicular carcinoma | 21 (6.6) |
| Incidental microcarcinoma | 20 (6.3) |
| NIFTP | 6 (1.8) |
NIFTP, non-invasive follicular thyroid neoplasm with papillarylike nuclear features.
The malignancy rate of the nodules classified as Bethesda class IV was 28.8%. In 3.4% of all cases, we found a neoplasm in a nodule different from the one subjected to fine needle aspiration. Out of the 71 papillary carcinomas, 9 (12.6%) were found to have local and/or lymphovascular invasion, while out of the 21 follicular carcinomas, 17 (80.9%) were found to have local and/or lymphovascular invasion. Out of the 71 papillary carcinomas, 22 (30.9%) were multifocal, while out of the 21 follicular carcinomas, 2 (9.5%) were multifocal.
Follicular carcinomas were found to have more aggressive features than papillary carcinomas but resulted less frequently multifocal.
The average preoperative size, obtained after ultrasonography, of the nodules that resulted carcinoma on histological examination were compared with the postoperative size emerged from the anatomopathological analysis. The mean preoperative size of the carcinomas was 20.4 mm, while the postoperative one resulted 18.9 mm (Figure 2). We searched a possible correlation between the preoperative size of malignant nodules and the histotype (papillary carcinoma vs. follicular carcinoma). In our sample, follicular carcinomas were found to have an average larger size than papillary carcinomas (31.6 vs. 17.1 mm), with a statistically significant difference (P<0.001) (Figure 3). The size criterion was also related to the incidence of carcinoma. Considering the 59 nodules smaller/equal to 1 cm, in 14 cases (23.7%) a diagnosis of carcinoma was made. Among the 239 cases larger than 1 cm but less than 4 cm, 69 (28.9%) resulted carcinomas.


Analyzing the 22 nodules larger/equal to 4 cm, the diagnosis of carcinoma was made in 9 cases (40.9%) (Table 4).
Table 4
| Preoperative size | Carcinoma, n (%) | Total | |
|---|---|---|---|
| Yes | No | ||
| ≤1 cm | 14 (23.7) | 45 (76.3) | 59 |
| >1 to <4 cm | 69 (28.9) | 170 (71.1) | 239 |
| ≥4 cm | 9 (40.9) | 13 (59.1) | 22 |
Nodule size was considered as a continuous variable, and it was found that with increasing size there was an increased malignancy rate (P<0.01).
Among the nodules that resulted malignant on post-operative histological examination, we analyzed the anatomopathological malignancy features, searching for a correlation between nodule size and neoplastic aggressiveness. We assessed local/vascular invasion, multifocality and presence of lymph node metastasis.
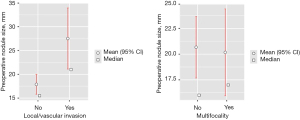
Our analysis revealed a statistically significant correlation between increased nodule size and local/lymphovascular invasion (P<0.05). On the other hand, no statistically significant correlation between nodule size and multifocality was found (Figure 4).
After postoperative histological examination, lymph node metastases were found in two patients, but our data did not show a statistically significant correlation between preoperative size and incidence of lymph node metastases. This finding may have been influenced by the small number of patients with lymph node metastases (Figure 5).

Considering 55 years as a cut-off, we found that patients younger/equal to 55 have a higher risk of cancer than those older than 55 (P=0.004). In the younger group, a malignancy rate of 35% (60 out of 168) was found, significantly higher than the older group, which showed a rate of 21% (32 out of 152 patients). On the other hand, in our study sex did not seem to influence the malignancy risk.
Finally, we analyzed the number of patients that underwent radioimetabolic therapy after surgery. We found those data only on 53 patients, 39 diagnosed with papillary carcinoma and 14 diagnosed with follicular carcinoma. Out of the 39 patients with papillary carcinoma, 23 (59%) underwent radiometabolic treatment, while out of the 14 patients with follicular carcinoma, 12 (86%) underwent radiometabolic treatment. A total of 35 patients (66%) resulted to need this treatment (Table 5).
Table 5
| Postoperative diagnosis | Radiometabolic treatment, n [%] | Total | |
|---|---|---|---|
| Yes | No | ||
| Papillary carcinoma | 23 [59] | 16 [41] | 39 |
| Follicular carcinoma | 12 [86] | 2 [14] | 14 |
| Total | 35 | 18 | 53 |
Discussion
In the treatment of indeterminate thyroid nodules, increasing emphasis is being placed on appropriateness of care and avoidance of over-and under-treatment, since total thyroidectomy gives a complete diagnostic and therapeutic certainty in cases of thyroid carcinoma but an initial total thyroidectomy for benign disease might be considered excessive or unnecessary from an oncologic standpoint (8).
As confirmed by a recent review on the literature by Almquist (9), in patients with nodules with high-risk indeterminate cytology, diagnostic lobectomy should be the preferable surgical approach, in absence of factors that suggest a total thyroidectomy. The 2015 American Thyroid Association guidelines include among these factors also the finding of positivity for specific mutations for carcinoma, the presence of an ultrasound pattern particularly suspicious for malignancy, size greater than 4 cm, the presence of bilateral nodules, a history of radiation exposure or the presence of familial thyroid cancer (4).
From these guidelines, it also emerged that total thyroidectomy is no longer the recommended surgical procedure for all differentiated thyroid carcinomas larger than 1 cm, lobectomy can be a sufficient initial treatment in the case of: differentiated neoplasms smaller than 4 cm, minimally invasive follicular carcinomas, non-invasive follicular thyroid neoplasm with papillarylike nuclear features (NIFTP) of all sizes, and encapsulated and intrathyroidal papillary carcinomas with follicular variant (4,10). This therapeutic approach is supported by the fact that surgery extension does not appear to have a significant effect on survival or on recurrence rate (11,12) and by the fact that lobectomies have an almost halved complication rate compared to total thyroidectomies (11% vs. 20%) (13). Furthermore, a conservative resection allows the preservation of glandular functionality in about 80% of cases (14), and in the need of a thyroidectomy totalization, outcome and complication rates are similar to single step total thyroidectomies (15,16).
From the data of this retrospective study, a strong impact of the 2015 ATA Guidelines emerged on the choice of the surgical approach, with a progressive propensity towards a conservative approach for the treatment of thyroid nodules with indeterminate cytology (17). We found an increase of lobectomies, from 7.2% to 41.5%, after the introduction of the new guidelines. However, in our sample the percentage of lobectomies remains below 50%; this data is certainly influenced by the number of cases of multinodular pathology, often bilateral, in our geographical area. In fact, in the analyzed sample, preoperative ultrasound study found multiple nodularities in 56.9% of cases and bilateral nodularity in 39.7%.
Several studies have shown that rates of goiter, nodular goiter, and papillary thyroid cancer are higher in iodine-insufficient areas than in those that have sufficient iodine (18).
Iodine deficiency has been shown to increase TSH levels determining hyperplasia and hypertrophy of follicular cells (2). Iodine deficiency surely contributes to the frequent finding of multinodular pathology in our patients and often influenced the surgical procedure choice in our sample.
Therapeutic attitude also changed in patients with preoperative findings of bilateral nodularity, in fact, we found 0% of lobectomies in presence of bilateral nodules in the period prior to 2015, and 18.7% in the subsequent period.
In our series, the malignancy rate of Bethesda class IV nodules, was 28.8% as the main literature data (6).
The average preoperative size of the nodules that resulted carcinoma after histological examination was 20.4 mm while postoperative size was 18.9 mm. In our series ultrasound was confirmed as a reliable tool for assessing thyroid nodule size (4,5,19-21).
Although some studies state that there is no correlation between size increase and diagnosis of differentiated carcinoma (22,23), our data showed that preoperative thyroid nodule size, considered as a continuous variable, is correlated with an increase malignancy rate (P<0.01).
In our study, we found a diagnosis of carcinoma in 23.7% of the nodules with a size less/equal to 1 cm, in 29.9% of the nodules larger than 1 cm but less than 4 cm and in 40.9% of the nodules larger than 1 cm or equal to 4 cm. Therefore, a significantly higher percentage of carcinoma diagnosis emerged in nodules larger than 4 cm, compared to the one smaller than 4 cm. This supports the indication to perform a total thyroidectomy in nodules larger than 4 cm, as recommended by ATA guidelines. This finding seems in contrast with a recent multicentric study published by our group (24) in which we analyzed 761 patients that underwent thyroid surgery with indeterminate cytology nodules in the period between January 2010 and December 2018 at the General Surgery Unit of the University Hospital of Parma and at the Endocrine Surgery Unit of the “Morgagni-Pierantoni” Hospital of Forlì. In this study we found that therapeutic or diagnostic lobectomy should be the treatment of choice for most thyroid nodules with indeterminate cytology, in the absence of other indications for total thyroidectomy, regardless of the nodule size. The different result could be related to the inclusion in the prior study of Bethesda class III nodules that have an average lower malignancy rate than class IV nodules (25).
Our data agree with a meta-analysis published in 2016 by Hammad et al. (26) which states that nodules size correlates with the risk of carcinoma, although according to their analysis this isn’t true for nodules larger than 6 cm which, on the contrary, are more frequently benign.
In agreement with most studies (27,28), also in our analysis follicular carcinomas were found to have a greater average size than papillary carcinomas (31.6 vs. 17.1 mm), with a statistically significant difference (P<0.001).
A statistically significant correlation also emerged between nodule size increase and local/lymphovascular invasion (P<0.05). This finding is in contrast with what was stated in a recent study by Valderrabano et al. (29), in fact in their study they didn’t find a correlation between tumor size and aggressiveness. On the other hand, the lack of correlation between size and presence of multifocality, and between size and presence of lymph node metastases, emerged from our study, was in agreement with the aforementioned work.
In our sample, in line with scientific literature (28,29), a statistically significant correlation was highlighted between age minor than 55 years and increased malignancy rate (30), while the absence of correlation between female sex and higher malignancy rate, emerged from our study, resulted in contrast to literature.
Out of the patients where it was possible to find this data, 66% underwent radiometabolic treatment: 59% of the patients with papillary carcinoma, and 85% of the patients with follicular carcinoma. This data should be analyzed considering that, in our sample, follicular carcinomas were found to have larger size and more aggressive characteristics than papillary carcinomas; in fact, local and/or lymphovascular invasion was found in 80% of cases, compared to 12.6% of papillary carcinomas. It may be that in our sample we found follicular carcinoma in more advanced stage because the more aggressive papillary cancers are not diagnosed as Bethesda class IV on fine needle aspiration but may rather be diagnosed in Bethesda class V or VI. Radioiodiometabolic treatment was assessed only in 53 patients, so this data still has relative reliability.
In agreement with scientific literature in our series minimally invasive video-assisted thyroidectomy (MIVAT) resulted a feasible technique for the treatment of various patients with Bethesda class IV nodules (31-36).
It is now established that the type of surgical approach must be discussed with the patient, considering both malignancy risk emerged from the preoperative study and patient’s will.
This study has some limitations due to the retrospective nature of the study and to the fact that it is a single institution analysis, maybe a bigger sample of patients could enforce the reliability of the results.
Conclusions
As confirmed by the latest guidelines, in patients with Bethesda class IV thyroid nodules, diagnostic lobectomy should be the preferable surgical approach, in the absence of factors that suggest a total thyroidectomy.
In an iodocarent geographical area, such as the province of Parma, the presence of cases of multinodular pathology, often bilateral, is frequent and influences the surgical approach.
Our analysis shows a statistically significant correlation between preoperative size of indeterminate nodules, Bethesda class IV, and increased malignancy rate, in particular for follicular carcinomas. Therefore, in our opinion, total thyroidectomy remains the first choice for the treatment of large nodules (≥4 cm) as these nodules have a high malignancy rate, greater local/lymphovascular invasion and a consequent frequent indication for post-operative radiometabolic treatment.
An accurate preoperative study is essential to decide, in accordance with the patient, the best surgical approach.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-491/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-491/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-491/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-491/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of University Hospital of Parma (No. 84/2022/OSS*/AOUPR),
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- AIOM. Linee guida tumore della tiroide 2021. Available online: https://www.aiom.it
- Laurberg P, Cerqueira C, Ovesen L, et al. Iodine intake as a determinant of thyroid disorders in populations. Best Pract Res Clin Endocrinol Metab 2010;24:13-27. [Crossref] [PubMed]
- Barrea L, Gallo M, Ruggeri RM, et al. Nutritional status and follicular-derived thyroid cancer: An update. Crit Rev Food Sci Nutr 2021;61:25-59. [Crossref] [PubMed]
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Russ G, Bonnema SJ, Erdogan MF, et al. European Thyroid Association Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules in Adults: The EU-TIRADS. Eur Thyroid J 2017;6:225-37. [Crossref] [PubMed]
- Cibas ES, Ali SZ. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid 2017;27:1341-6. [Crossref] [PubMed]
- Kandil E, Krishnan B, Noureldine SI, et al. Hemithyroidectomy: a meta-analysis of postoperative need for hormone replacement and complications. ORL J Otorhinolaryngol Relat Spec 2013;75:6-17. [Crossref] [PubMed]
- Schneider DF, Cherney Stafford LM, Brys N, et al. Gauging the extent of thyroidectomy for indeterminate thyroid nodules: an oncologic perspective. Endocr Pract 2017;23:442-50. [Crossref] [PubMed]
- Almquist M, Muth A. Surgical management of cytologically indeterminate thyroid nodules. Gland Surg 2019;8:S105-11. [Crossref] [PubMed]
- Haugen BR, Sawka AM, Alexander EK, et al. American Thyroid Association Guidelines on the Management of Thyroid Nodules and Differentiated Thyroid Cancer Task Force Review and Recommendation on the Proposed Renaming of Encapsulated Follicular Variant Papillary Thyroid Carcinoma Without Invasion to Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features. Thyroid 2017;27:481-3. [Crossref] [PubMed]
- Nixon IJ, Ganly I, Patel SG, et al. Thyroid lobectomy for treatment of well differentiated intrathyroid malignancy. Surgery 2012;151:571-9. [Crossref] [PubMed]
- Mendelsohn AH, Elashoff DA, Abemayor E, et al. Surgery for papillary thyroid carcinoma: is lobectomy enough? Arch Otolaryngol Head Neck Surg 2010;136:1055-61. [Crossref] [PubMed]
- Hauch A, Al-Qurayshi Z, Randolph G, et al. Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol 2014;21:3844-52. [Crossref] [PubMed]
- Stoll SJ, Pitt SC, Liu J, et al. Thyroid hormone replacement after thyroid lobectomy. Surgery 2009;146:554-8; discussion 558-60. [Crossref] [PubMed]
- Erdem E, Gülçelik MA, Kuru B, et al. Comparison of completion thyroidectomy and primary surgery for differentiated thyroid carcinoma. Eur J Surg Oncol 2003;29:747-9. [Crossref] [PubMed]
- Canu GL, Medas F, Cappellacci F, et al. Risk of Complications in Patients Undergoing Completion Thyroidectomy after Hemithyroidectomy for Thyroid Nodule with Indeterminate Cytology: An Italian Multicentre Retrospective Study. Cancers (Basel) 2022;14:2472. [Crossref] [PubMed]
- Del Rio P, Pisani P, Montana Montana C, et al. The surgical approach to nodule Thyr 3-4 after the 2.2014 NCCN and 2015 ATA guidelines. Int J Surg 2017;41:S21-5. [Crossref] [PubMed]
- Cao LZ, Peng XD, Xie JP, et al. The relationship between iodine intake and the risk of thyroid cancer: A meta-analysis. Medicine (Baltimore) 2017;96:e6734. [Crossref] [PubMed]
- Cosgrove D, Piscaglia F, Bamber J, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med 2013;34:238-53. [Crossref] [PubMed]
- Kwak JY, Han KH, Yoon JH, et al. Thyroid imaging reporting and data system for US features of nodules: a step in establishing better stratification of cancer risk. Radiology 2011;260:892-9. [Crossref] [PubMed]
- Perros P, Boelaert K, Colley S, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf) 2014;81:1-122. [Crossref] [PubMed]
- McHenry CR, Huh ES, Machekano RN. Is nodule size an independent predictor of thyroid malignancy? Surgery 2008;144:1062-8; discussion 1068-9. [Crossref] [PubMed]
- Shrestha M, Crothers BA, Burch HB. The impact of thyroid nodule size on the risk of malignancy and accuracy of fine-needle aspiration: a 10-year study from a single institution. Thyroid 2012;22:1251-6. [Crossref] [PubMed]
- Cozzani F, Bettini D, Rossini M, et al. Thyroid nodules with indeterminate cytology: association between nodule size, histopathological characteristics and clinical outcome in differentiated thyroid carcinomas - a multicenter retrospective cohort study on 761 patients. Updates Surg 2021;73:1923-30. [Crossref] [PubMed]
- Yaprak Bayrak B, Eruyar AT. Malignancy rates for Bethesda III and IV thyroid nodules: a retrospective study of the correlation between fine-needle aspiration cytology and histopathology. BMC Endocr Disord 2020;20:48. [Crossref] [PubMed]
- Hammad AY, Noureldine SI, Hu T, et al. A meta-analysis examining the independent association between thyroid nodule size and malignancy. Gland Surg 2016;5:312-7. [Crossref] [PubMed]
- Sippel RS, Elaraj DM, Khanafshar E, et al. Tumor size predicts malignant potential in Hürthle cell neoplasms of the thyroid. World J Surg 2008;32:702-7. [Crossref] [PubMed]
- Kamran SC, Marqusee E, Kim MI, et al. Thyroid nodule size and prediction of cancer. J Clin Endocrinol Metab 2013;98:564-70. [Crossref] [PubMed]
- Valderrabano P, Khazai L, Thompson ZJ, et al. Association of Tumor Size With Histologic and Clinical Outcomes Among Patients With Cytologically Indeterminate Thyroid Nodules. JAMA Otolaryngol Head Neck Surg 2018;144:788-95. [Crossref] [PubMed]
- Filetti S, Durante C, Hartl D, et al. Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol 2019;30:1856-83. [Crossref] [PubMed]
- Del Rio P, Viani L, Montana CM, et al. Minimally invasive thyroidectomy: a ten years experience. Gland Surg 2016;5:295-9. [Crossref] [PubMed]
- Del Rio P, Maestroni U, Sianesi M, et al. Minimally invasive video-assisted thyroidectomy for papillary thyroid cancer: a prospective 5-year follow-up study. Tumori 2015;101:144-7. [Crossref] [PubMed]
- Miccoli P, Biricotti M, Matteucci V, et al. Minimally invasive video-assisted thyroidectomy: reflections after more than 2400 cases performed. Surg Endosc 2016;30:2489-95. [Crossref] [PubMed]
- Del Rio P, Arcuri MF, Pisani P, et al. Minimally invasive video-assisted thyroidectomy (MIVAT): what is the real advantage? Langenbecks Arch Surg 2010;395:323-6. [Crossref] [PubMed]
- Del Rio P, Arcuri MF, Cataldo S, et al. Are we changing our inclusion criteria for the minimally invasive videoassisted thyroidectomy? Ann Ital Chir 2014;85:28-32. [PubMed]
- Miccoli P, Fregoli L, Rossi L, et al. Minimally invasive video-assisted thyroidectomy (MIVAT). Gland Surg 2020;9:S1-5. [Crossref] [PubMed]


