
A clinical practice review on process efficiency in autologous breast reconstruction
Introduction
Background
Breast reconstruction with autologous tissue is considered the gold standard method to restore breast shape after cancer because of the higher patient satisfaction and superior long-term outcomes (1-4). Constant improvements in surgical technique and better understanding of anatomy has allowed an increase in the complement of patient options. In fact, surgeons can tailor the reconstruction based on each individual’s needs and donor site availability with a complication rate comparable to prosthetic breast reconstruction (5,6). Ancillary diagnostic procedures such as computed tomographic angiography (CTA) images and indocyanine green angiography has shown to reduce significantly donor-site complications and fat necrosis improving perforator selection and flap inset (7-9). In addition, enhanced recovery pathways have considerably improved the post-operative course reducing the length of stay, opioid requirement, and costs (10,11). For these reasons, in recent years, the focus of breast reconstructive microsurgeons has progressively shifted from flap success to aesthetics and efficiency (12).
Rationale and knowledge gap the need for increased efficiency
Prolonged operative time remains one of the main limits of autologous breast reconstruction procedures, which is made of multiple complex and potentially time-consuming steps. In a typical bilateral breast reconstruction, there can be four surgical sites. Globally, the procedure requires flap harvest, recipient site preparation, microsurgical anastomoses and flap inset, which can take from 8 to 12 hours to be completed in many surgical practices. Thus, surgeons’ and patients’ choice can be influenced towards prosthetic breast reconstruction, even in patients in which prostheses are typically contraindicated (13,14).
Prolonged operative time is associated with increased surgical and medical complications in many surgical fields (15). Specific to autologous breast reconstruction there is a significant raise in surgical (including flap failure rates), medical, wound complications and length of stay with increasing operative time (16-18). Additionally, with an increasing number of patients undergoing mastectomy and requiring autologous breast reconstruction there is an increasing need to be able to accommodate these patients. The safety and feasibility of performing multiple free flaps within the hours of a single working day has been previously demonstrated (19). Even if surgeon experience is considered a significant factor influencing the duration of the surgery together with other technical aspects (20) and extra-operative factors (21), a systematic approach to surgery with process mapping can significantly reduce operative time.
Process mapping is a technique initially used in industries to expedite production based on the partition of a complex process into multiple steps in order to analyze and optimize each step. It consists of a graphic diagram showing the sequence of activities and tasks performed by each individual involved in the overall process. Once the individual elements are visually represented any waste of time or errors becomes readily apparent. This analysis helps with optimization of every step resulting in improved productivity.
A multidisciplinary discussion should be utilized to create a map for the process. This should involve a clear definition of each step and the boundaries of the process to be analyzed. Specific symbols and colors should be used to identify the step and the involved team member. Once completed the map should be tested and approved (22,23). The application of this strategy in the healthcare systems is part of the quality improvement strategy recommended by The World Health Organization to increase efficiency and safety in medicine. In surgery it can be applied to the entire perioperative period, even though many authors mainly focus on intraoperative steps for the impact of operative room utilization and operative costs. Process mapping of the intraoperative period results in increased efficiency in different fields of surgery (24).
Objective: process efficiency in microsurgical breast reconstruction
General improvements and increased efficiency in autologous breast reconstruction is the aim of many plastic surgeons that desire to make these procedures more practical by minimizing time waste. The aim of the paper was to review the existing literature dealing with process efficiency evaluating its impact in improving autologous breast reconstruction.
Methods
Literature in NCBI database (PubMed) was reviewed using combinations of key words (efficiency, autologous breast reconstruction, process mapping, DIEP flap, operative time). All English papers were included.
Results
In the literature nine papers dealt with efficiency in autologous breast reconstruction. Two papers retrospectively evaluated the impact of different steps in autologous breast reconstruction without a proper process mapping approach (25,26). Process mapping was specifically utilized in seven papers dealing with unilateral or bilateral deep inferior epigastric perforator (DIEP) flap breast reconstruction. A retrospective review of data was performed in three papers, while four papers were based on prospectively acquired data. Two studies specifically compared the impact of process mapping between a mapped cohort/group and a non-mapped one (Table 1). Only one paper focused on optimizing efficiency in a non-DIEP flap breast reconstruction through a retrospective analysis of bilateral muscle-sparing TRAM flaps.
Table 1
| Authors | Flap type and number of flaps | Country | Duration | Study design | Intervention stated | Number of process segments | Steps | Comparison of training level | Co-surgery attending model | Outcome considered | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Elliott et al. 2007 (26) | 111 muscle sparing free TRAM flaps: 91 unilateral, 10 bilateral | United States | 3 years | Retrospective review | Standardization of operative sequence | No process mapping | N/A | N/A | N/A Complication | Operative time | |
| Lee et al. 2008 (27) | 225 DIEP flaps: 50 unilateral and 50 bilateral before pathway, 25 unilateral and 25 bilateral after pathway | United States | 4 years | Prospectively acquired database | Intraoperative pathway based on “relational coordination” teamwork. Comparison between mapped and non-mapped group | 9 steps: - Mastectomy - Perforator dissection - Flap harvest - Recipient vessel harvest - Division of vessels - Flap transfer - Microsurgery - Flap inset - Closure |
N/A | N/A | N/A | Operative time Complications Operating room and hospital costs Administration of prophylactic antibiotics and heparin Operating room staff satisfaction surveys |
|
| Canizares et al. 2015 (25) | 104 DIEP flaps: 32 unilateral, 36 bilateral | United States | 6 months | Retrospective review | Standardization of operative sequence | - No process mapping | N/A | N/A | N/A | Operative time | |
| Marsh et al. 2016 (28) | 163 immediate, delayed, unilateral or bilateral DIEP flaps | United Kingdom | 12 months | Retrospective review | Process mapping | - Mastectomy | - Simultaneous flap elevation, harvest and abdominal closure | N/A | N/A | N/A | Operative time Complications |
| - Prep recipient vessels | - Simultaneous flap shaping | ||||||||||
| - Anastomosis | |||||||||||
| - Hemostasis | |||||||||||
| - Flap inset | |||||||||||
| - Wound closure | |||||||||||
| Sharma et al. 2019 (29) | 20 unilateral DIEP flaps: process mapped 6 delayed and 4 immediate, control 3 delayed and 7 immediate | United Kingdom | N/A | Prospective cohort study comparing two groups | Process mapping | 100 | N/A | N/A | Operative time | ||
| Comparison between mapped and control group | - Preparation and draping | ||||||||||
| - Initial flap raise | |||||||||||
| - Perforator dissection | |||||||||||
| - Vessel preparation and Flap inset | |||||||||||
| - Abdominal closure | |||||||||||
| - Microsurgery | |||||||||||
| - Breast/Flap closure | |||||||||||
| - Final transfer | |||||||||||
| Haddock and Teotia 2020 (30) | 147 unilateral DIEP flaps | United States | 9 months | Prospective process analysis | Process mapping | - Flap harvest | 8 | Yes | Yes | Operative time | |
| - Microsurgery | 3/4-person team | Complications | |||||||||
| Haddock and Teotia 2021 (12) | 50 consecutive bilateral DIEP flaps | United States | 8 months | Prospective process analysis | Process mapping | - Recipient site preparation | 23 | Yes | Yes | Operative time | |
| - Flap harvest | 3/4-person team | Complications | |||||||||
| - Microsurgery | |||||||||||
| - Breast inset | |||||||||||
| - Abdominal closure | |||||||||||
| Easton et al. 2022 (32) | 32 bilateral autologous breast reconstruction with DIEP, TRAM, flaps | United States | 5 years | Retrospective cohort study | 4DX business Model (the 4 Disciplines of Execution) | - Preoperative and intraoperative interventions | N/A | No | Yes | Operative time | |
| - Timing of presurgical steps | Length of stay | ||||||||||
| - Timing of intraoperative steps (chest dissection, perforator dissection, anastomosis | Complications | ||||||||||
| - Procedure duration | |||||||||||
| Haddock et al. 2023 (31) | 375 bilateral DIEP flaps | United States | - 9 months for flap harvest and microsurgery- 8 months for entire operation | Prospective process analysis | Process mapping | - Recipient site preparation - Flap harvest - Microsurgery -Breast inset -Abdominal closure |
8 23 |
Yes | Yes 3/4-person team |
Operative time Complications |
|
N/A, not available; DIEP, deep inferior epigastric perforator; TRAM, transverse rectus abdominal muscle.
Lee et al. used a multidisciplinary team discussion based on “relational coordination” teamwork, similar in design to a Harvard Business School model to identify each step (27). Marsh et al. used a personal approach to process mapping, without stating the method used to select different steps (28). Sharma et al. based the process mapping on the observation of senior author’s experience (29). Haddock and Teotia mapped exclusively the surgical procedure and based the selection of different steps on their experience discussing the map with the team before surgery (30).
Even if the number, type, and order of steps differ among papers, the main categories were in common. All authors analyzed the steps involving flap harvest and microsurgery. Lee et al. and Marsh et al. included the mastectomy in the process mapping in the immediate breast reconstruction group (27,28). All surgeons suggested to perform different steps in sequence and in parallel with simultaneous execution of multiple steps concurrently (i.e., mastectomy and flap elevation, anastomosis, and abdominal closure etc.).
The primary outcome measured in all papers was operative time. Elliott et al. reported an average operative time of 185 minutes (3 hours and 5 minutes) for unilateral free TRAM flap breast reconstruction (26). Lee et al. compared outcomes before and after implementation of the mapping protocol. They reported a significant reduction of operative time both in unilateral (from 8.2 to 6.9 hours) and bilateral reconstruction (from 12.8 to 10.6 hours). Additional outcomes considered were the rate of complication, which remained the same, the cost of the surgery, which decreased. The intraoperative administration of antibiotic and heparin became more consistent in the mapped group. The satisfaction survey showed increased staff satisfaction (27). Canizares et al. reported an average operative time of 201 minutes (3 hours and 21 minutes) for unilateral cases and 346 minutes (5 hours and 46 minutes) for bilateral cases (25). Marsh et al. reported a mean operative time including unilateral and bilateral cases of 248 minutes (4 hours and 8 minutes) (28).
Sharma et al. compared a process-mapped group with a non-mapped group of unilateral DIEP flaps showing a significant reduction of operative time, 163.1 minutes (2 hours and 43 minutes) vs. 219.2 minutes (3 hours and 39 minutes) respectively. Differences in techniques used, pedicle length and used of barbed sutures with comparable complication rate were reported (29). In 2020, Haddock and Teotia reported an average total procedure time for bilateral autologous breast reconstruction with DIEP flaps of 340.3 minutes (5 hours and 40 minutes) with 73.1 minutes improvement compared to historical data (30). In this series the authors mapped only a portion of the operation. The same authors, in 2021, reported a mean operative time from skin to skin of 238 min (3 hours and 58 minutes) for bilateral cases. The number of complications remained comparable to non-mapped surgery (12). In a most recent paper a decrease in risk of morbidity was associated to the process mapping group (31). The impact of different level of expertise on each step was considered for training purposes in each study. Easton et al. evaluated the impact of the application of a business model called the Four Disciplines of Execution in increasing efficiency in autologous breast reconstruction. They retrospectively compared a pre (15 cases of bilateral breast reconstruction) and a post (17 cases of bilateral breast reconstruction) intervention cohort aiming in performing the surgery in less than nine hours. Even if comparing cohorts with different types of autologous breast reconstruction, they were able to show a significant reduction of operative time and length of stay without an increase of complications (32).
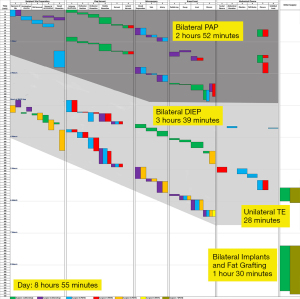
In all included studies the surgeons were aware of the process mapping and the increased awareness of tracking operative time. While the Hawthorne effect very likely plays a roll (33), one study evaluated the sustained impact of process analysis. Haddock and Teotia evaluated the sustained impact of their two process analysis studies before, between and after the study periods (31). The findings were significant in that the benefits were sustained in both operative efficiency and decreased morbidity following the process analysis time periods (see Figure 1).
Discussion
Autologous breast reconstruction is an ideal field for process mapping: each procedure can be long, made of multiple complex surgical steps requiring coordination and a precise sequence. In addition, the number of patients requiring, or electing, autologous breast reconstruction continues to increase. In current times the DIEP flap is the most common autologous option, and for these reasons, several authors have focused on improving efficiency of the procedure. A comprehensive study of the impact of process mapping on alternative flaps has yet to be performed.
The process mapping produced a reduction in operative time in all studies analyzed, even if the steps and categories considered were different among different facilities. This confirms the role of process mapping as a valuable tool to optimize efficiency in autologous breast reconstruction (24). A validated template shared by the international community of breast reconstructive microsurgeons would allow for comparisons and improvement in different centers worldwide. Further studies following the Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines could scientifically validate results obtained (34). Improved communication between team members and coordinated work between them are reported as the main advantages of process mapping with improvements in operative time, cost, quality measures, and staff satisfaction with a comparable complication rate (24). The use of different techniques and devices among mapped and non-mapped groups to reduce operative time can be considered a confounding variable.
Aside from intraoperative mapping, additional factors involving the preoperative and postoperative phases are known to improve autologous breast reconstruction efficiency and are commonly applied. Preoperative strategies proposed include a two-stage breast reconstruction approach, preoperative planning, and a multiple surgeon operating team. The reconstruction in 2 stages, initially proposed to manage the impact of post mastectomy radiotherapy in autologous breast reconstruction (35), has been shown to reduce operative time and improve efficiency in unilateral and bilateral DIEP flap breast reconstruction (36). Preoperative planning and selection of perforators guided by computed tomographic angiography imaging is associated with a significant reduction in overall operative time and flap harvest (7). The operating team is made up of at least two surgeons that usually work simultaneously in different steps of the surgery allowing different procedures to be performed at the same time (such as recipient site preparation and flaps harvesting or microsurgery and donor site closure). The co-surgery model, based on two expert microsurgeons working together has been shown to further optimize surgical efficiency and outcomes in DIEP breast reconstruction (37). Furthermore, flap perfusion evaluation, postoperative monitoring, and enhanced recovery after surgery (ERAS) protocols have optimized post-operative care (10,11).
The great benefits in terms of efficiency and outcomes offered by process mapping applied to DIEP flap breast reconstruction support its application also to secondary options for autologous breast reconstruction (i.e., Profunda Artery Perforator Flap, Lumbar Artery Perforator Flap, etc.). In addition, multiple donor sites and position changes can be needed with increased complexity of surgical flow (38-40).
Easton et al. (32) did include in their retrospective review several different types of flaps [i.e., DIEP, TRAM, profunda artery perforator (PAP), transverse upper gracilis (TUG)]. However, the different steps of the process did not apply equally to all flaps thus quantitative analysis were performed only with DIEP/TRAM flaps.
Utilization of process mapping is ideal for these procedures and should be implemented as they become more common at centers of excellence.
Process mapping is one of many quality improvement strategies and instead of being considered an endpoint in efficiency optimization it should be considered one of the multiple tools available (41). Additional active quality improvement strategies such as deliberate practice, Plan-Do-Study-Act—PDSA, and Six Sigma or Lean Six Sigma can be used to further reduce wasted time and implement error recognition strategies, taking advantage of constant feedback systems and information provided by mapped surgeries (31,42).
Although aimed in limiting operative time and complications, quality improvement strategies in breast reconstruction should not distract surgeons from the final aesthetic shape of the breast. In fact, the ultimate goal of the surgery is to obtain the ideal aesthetic result for each patient limiting morbidity and time waste. With proper control of the operating environment there is no need to compromise in any of these goals.
The main limitation of this review is related to the scarce amount of paper available in the literature dealing with process efficiency and to the fact that the majority of papers deal with DIEP flap.
Conclusions
Process mapping is a valid strategy when seeing to implement efficiency in autologous breast reconstruction. Identification of surgical steps and implementation of each phase of surgery are effective in reducing operative time and increasing outcomes. The continuous feedback offered with the constant analysis of surgical procedures represent a valuable source of information for team members to evaluate and improve their practice. Still, autologous breast reconstruction aims to restore and potentially enhance the patient aesthetic outcomes after mastectomy and this goal is of paramount importance. Efficiency does not have to compromise the overall outcome for patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ketan M. Patel and Ara A. Salibian) for the series “Advances in Microsurgical Breast Reconstruction” published in Gland Surgery. The article has undergone external peer review.
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-680/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-680/coif). The series “Advances in Microsurgical Breast Reconstruction” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Eltahir Y, Werners LLCH, Dreise MM, et al. Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg 2013;132:201e-9e. [Crossref] [PubMed]
- Lagendijk M, van Egdom LSE, Richel C, et al. Patient reported outcome measures in breast cancer patients. Eur J Surg Oncol 2018;44:963-8. [Crossref] [PubMed]
- Santosa KB, Qi J, Kim HM, et al. Effect of Patient Age on Outcomes in Breast Reconstruction: Results from a Multicenter Prospective Study. J Am Coll Surg 2016;223:745-54. [Crossref] [PubMed]
- Weichman KE, Broer PN, Thanik VD, et al. Patient-Reported Satisfaction and Quality of Life following Breast Reconstruction in Thin Patients: A Comparison between Microsurgical and Prosthetic Implant Recipients. Plast Reconstr Surg 2015;136:213-20. [Crossref] [PubMed]
- Lagares-Borrego A, Gacto-Sanchez P, Infante-Cossio P, et al. A comparison of long-term cost and clinical outcomes between the two-stage sequence expander/prosthesis and autologous deep inferior epigastric flap methods for breast reconstruction in a public hospital. J Plast Reconstr Aesthet Surg 2016;69:196-205. [Crossref] [PubMed]
- Schmauss D, Machens HG, Harder Y. Breast Reconstruction after Mastectomy. Front Surg 2015;2:71. [PubMed]
- Haddock NT, Dumestre DO, Teotia SS. Efficiency in DIEP Flap Breast Reconstruction: The Real Benefit of Computed Tomographic Angiography Imaging. Plast Reconstr Surg 2020;146:719-23. [Crossref] [PubMed]
- Hembd A, Teotia SS, Zhu H, et al. Optimizing Perforator Selection: A Multivariable Analysis of Predictors for Fat Necrosis and Abdominal Morbidity in DIEP Flap Breast Reconstruction. Plast Reconstr Surg 2018;142:583-92. [Crossref] [PubMed]
- Hembd AS, Yan J, Zhu H, et al. Intraoperative Assessment of DIEP Flap Breast Reconstruction Using Indocyanine Green Angiography: Reduction of Fat Necrosis, Resection Volumes, and Postoperative Surveillance. Plast Reconstr Surg 2020;146:1e-10e. [Crossref] [PubMed]
- Haddock NT, Garza R, Boyle CE, et al. Defining Enhanced Recovery Pathway with or without Liposomal Bupivacaine in DIEP Flap Breast Reconstruction. Plast Reconstr Surg 2021;148:948-57. [Crossref] [PubMed]
- Rodnoi P, Teotia SS, Haddock NT. Economic Impact of Refinements in ERAS Pathways in DIEP Flap Breast Reconstruction. J Reconstr Microsurg 2022;38:524-9. [Crossref] [PubMed]
- Haddock NT, Teotia SS. Efficient DIEP Flap: Bilateral Breast Reconstruction in Less Than Four Hours. Plast Reconstr Surg Glob Open 2021;9:e3801. [Crossref] [PubMed]
- Gopie JP, Hilhorst MT, Kleijne A, et al. Women's motives to opt for either implant or DIEP-flap breast reconstruction. J Plast Reconstr Aesthet Surg 2011;64:1062-7. [Crossref] [PubMed]
- Nelson JA, Cordeiro PG, Polanco T, et al. Association of Radiation Timing with Long-Term Satisfaction and Health-Related Quality of Life in Prosthetic Breast Reconstruction. Plast Reconstr Surg 2022;150:32e-41e. [Crossref] [PubMed]
- Cheng H, Clymer JW, Po-Han Chen B, et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res 2018;229:134-44. [Crossref] [PubMed]
- Allan J, Goltsman D, Moradi P, et al. The effect of operative time on complication profile and length of hospital stay in autologous and implant-based breast reconstruction patients: An analysis of the 2007-2012 ACS-NSQIP database. J Plast Reconstr Aesthet Surg 2020;73:1292-8. [Crossref] [PubMed]
- Fogarty BJ, Khan K, Ashall G, et al. Complications of long operations: a prospective study of morbidity associated with prolonged operative time (> 6 h). Br J Plast Surg 1999;52:33-6. [Crossref] [PubMed]
- Offodile AC 2nd, Aherrera A, Wenger J, et al. Impact of increasing operative time on the incidence of early failure and complications following free tissue transfer? A risk factor analysis of 2,008 patients from the ACS-NSQIP database. Microsurgery 2017;37:12-20. [Crossref] [PubMed]
- Acosta R, Enajat M, Rozen WM, et al. Performing two DIEP flaps in a working day: an achievable and reproducible practice. J Plast Reconstr Aesthet Surg 2010;63:648-54. [Crossref] [PubMed]
- Laporta R, Longo B, Sorotos M, et al. Time-dependent factors in DIEP flap breast reconstruction. Microsurgery 2017;37:793-9. [Crossref] [PubMed]
- Kimbrough CW, McMasters KM, Canary J, et al. Improved Operating Room Efficiency via Constraint Management: Experience of a Tertiary-Care Academic Medical Center. J Am Coll Surg 2015;221:154-62. [Crossref] [PubMed]
- McLaughlin N, Rodstein J, Burke MA, et al. Demystifying process mapping: a key step in neurosurgical quality improvement initiatives. Neurosurgery 2014;75:99-109; discussion 109. [Crossref] [PubMed]
- Trebble TM, Hansi N, Hydes T, et al. Process mapping the patient journey: an introduction. BMJ 2010;341:c4078. [Crossref] [PubMed]
- Chung RD, Hunter-Smith DJ, Spychal RT, et al. A systematic review of intraoperative process mapping in surgery. Gland Surg 2017;6:715-25. [Crossref] [PubMed]
- Canizares O, Mayo J, Soto E, et al. Optimizing Efficiency in Deep Inferior Epigastric Perforator Flap Breast Reconstruction. Ann Plast Surg 2015;75:186-92. [Crossref] [PubMed]
- Elliott LF, Seify H, Bergey P. The 3-hour muscle-sparing free TRAM flap: safe and effective treatment review of 111 consecutive free TRAM flaps in a private practice setting. Plast Reconstr Surg 2007;120:27-34. [Crossref] [PubMed]
- Lee BT, Tobias AM, Yueh JH, et al. Design and impact of an intraoperative pathway: a new operating room model for team-based practice. J Am Coll Surg 2008;207:865-73. [Crossref] [PubMed]
- Marsh D, Patel NG, Rozen WM, et al. Three routine free flaps per day in a single operating theatre: principles of a process mapping approach to improving surgical efficiency. Gland Surg 2016;5:107-14. [PubMed]
- Sharma HR, Rozen WM, Mathur B, et al. 100 Steps of a DIEP Flap-A Prospective Comparative Cohort Series Demonstrating the Successful Implementation of Process Mapping in Microsurgery. Plast Reconstr Surg Glob Open 2019;7:e2016. [Crossref] [PubMed]
- Haddock NT, Teotia SS. Deconstructing the Reconstruction: Evaluation of Process and Efficiency in Deep Inferior Epigastric Perforator Flaps. Plast Reconstr Surg 2020;145:717e-24e. [Crossref] [PubMed]
- Haddock NT, Tycher JT, Teotia SS. Deliberate Practice and Process Analysis in DIEP Flap Breast Reconstruction: An Immediate and Sustained Decrease in Morbidity and Operative Time. Plast Reconstr Surg 2023; Epub ahead of print. [Crossref] [PubMed]
- Easton J, Roberto A, Lax E, et al. Using a Business Model (the 4 Disciplines of Execution) to Improve Consistency, Efficiency, and Length of Stay in Microvascular Autologous Breast Reconstruction. Ann Plast Surg 2022;89:532-7. [Crossref] [PubMed]
- McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol 2014;67:267-77. [Crossref] [PubMed]
- Ogrinc G, Mooney SE, Estrada C, et al. The SQUIRE (Standards for QUality Improvement Reporting Excellence) guidelines for quality improvement reporting: explanation and elaboration. Qual Saf Health Care 2008;17:i13-32. [Crossref] [PubMed]
- Frost MW, Niumsawatt V, Rozen WM, et al. Direct comparison of postoperative monitoring of free flaps with microdialysis, implantable cook-swartz Doppler probe, and clinical monitoring in 20 consecutive patients. Microsurgery 2015;35:262-71. [Crossref] [PubMed]
- Issa CJ, Lu SM, Boudiab EM, et al. Comparing Plastic Surgeon Operative Time for DIEP Flap Breast Reconstruction: 2-stage More Efficient than 1-stage? Plast Reconstr Surg Glob Open 2021;9:e3608. [Crossref] [PubMed]
- Haddock NT, Kayfan S, Pezeshk RA, et al. Co-surgeons in breast reconstructive microsurgery: What do they bring to the table? Microsurgery 2018;38:14-20. [Crossref] [PubMed]
- Haddock NT, Teotia SS. Lumbar Artery Perforator Flap: Initial Experience with Simultaneous Bilateral Flaps for Breast Reconstruction. Plast Reconstr Surg Glob Open 2020;8:e2800. [Crossref] [PubMed]
- Haddock NT, Teotia SS. Consecutive 265 Profunda Artery Perforator Flaps: Refinements, Satisfaction, and Functional Outcomes. Plast Reconstr Surg Glob Open 2020;8:e2682. [Crossref] [PubMed]
- Myers PL, Nelson JA, Allen RJ Jr. Alternative flaps in autologous breast reconstruction. Gland Surg 2021;10:444-59. [Crossref] [PubMed]
- Layton A, Moss F, Morgan G. Mapping out the patient's journey: experiences of developing pathways of care. Qual Health Care 1998;7:S30-6. [PubMed]
- Ericsson KA. Acquisition and maintenance of medical expertise: a perspective from the expert-performance approach with deliberate practice. Acad Med 2015;90:1471-86. [Crossref] [PubMed]


