
Individual treatment strategy of thyroglossal duct cyst carcinoma: a case report
Highlight box
Key findings
• We report an extremely rare case of thyroglossal duct cyst carcinoma.
What is known and what is new?
• Thyroglossal duct cyst carcinoma is usually an accidental result of histopathological evaluation after Sistrunk surgery.
• For further treatment after full resection of the cyst, especially total thyroidectomy, cervical lymph node dissection and postoperative radioactive iodine therapy, it is recommended to adjust the treatment strategy according to the prognostic risk.
What is the implication, and what should change now?
• Uniform treatment guidelines of management after Sistrunk surgery are lacking, so we recommend tailoring individualized treatment based on individual risk stratification.
Introduction
The thyroid originates from the 3rd to 4th week of embryonic development, and the median primordium is formed by endodermal hyperplasia between the 1st and 2nd pharyngeal sacs. When the primordium descends, it is still connected to the pharyngeal fundus by the thyroglossal duct. At the 7th embryonic week, normal thyroid tissue has developed before the trachea (1). Ectopic thyroid is a rare embryological abnormality, existing outside the pretracheal area. It is caused by the abnormal descent of thyroid primordial tissue during embryogenesis. It can occur in any part of the thyroid’s descent, from the foramen cecum linguae to the sternal notch. Ectopic thyroid is relatively rare, with an incidence of 1:100,000 to 300,000; in patients with thyroid disease, the incidence is 1:4,000 to 8,000 (2).
Thyroglossal duct cyst is caused by incomplete degeneration and atresia and incomplete disappearance of the epithelium of the thyroglossal duct during embryonic development. It is the most common cause of midline neck swelling, and the incidence rate in the general adult population is ~0.5–3% (3). In 1891, His (4) was the first to report thyroglossal duct remnants progressing to thyroglossal duct cysts, and 1.5–45% of cases show ectopic thyroid tissue in the cyst (5,6). In most cases, the cause of ectopic thyroid tissue remains unclear, but mutation of thyroid transcription factor (TTF)-2, which is required for thyroid descent, is considered to be a possible mechanism (7). The occurrence of carcinoma in a thyroglossal duct cyst is extremely rare, and there are few reports in the literature. The first case was reported by Brentano in 1911 (8). Here, we report a case of histopathologically confirmed papillary thyroid carcinoma in a thyroglossal duct cyst. Through the analysis of the clinical data, we discuss the clinical characteristics, and provide reference for diagnosis and treatment. We present the following article in accordance with the CARE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-23-102/rc).
Case presentation
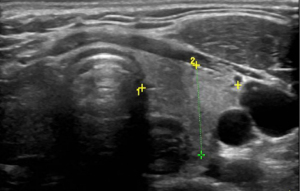
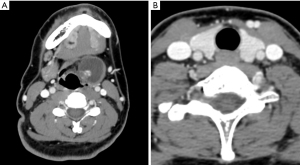
The patient was a 25-year-old woman who visited the Department of Otorhinolaryngology-Head and Neck Surgery because of a tumor in her neck for 6 mouths. The tumor had gradually increased over the past 2 months, and she had a foreign body sensation in the pharynx, without dysphagia, pain or other symptoms. Specialist physical examination detected a 3.0 cm × 3.0 cm sub-round, tough mass slightly to the left side of the anterior median of the neck (below the hyoid bone), with a smooth surface and clear boundary, which could move with swallowing. Laryngoscopy showed no abnormality in the throat. Blood routine and thyroid function were normal [i.e., free T3 and T4, thyroid stimulating hormone (TSH) and thyroglobulin levels were within their normal ranges]. Cervical ultrasound showed a left-sided cystic-solid mass in the middle of the neck, ~3.8 cm × 2.6 cm, with the solid part ~1.8 cm × 1.2 cm, with multiple point-like strong echoes visible inside. Thyroid echogenicity was normal, and no obvious mass was seen (Figure 1). There were no obvious enlarged lymph nodes on either side of the neck. Enhanced computed tomography (CT) showed the cystic-solid structure located between the left hyoid bone and thyroid cartilage, with high-density nodules locally, which were enhanced (Figure 2A). There was no obvious abnormality in the thyroid and cervical lymph nodes (Figure 2B).
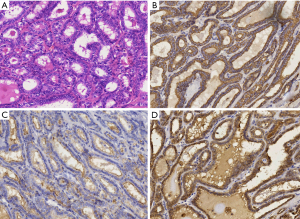
Due to the appearance and location of the mass, preoperative diagnosis was considered to be thyroglossal duct cyst. However, the solid part in the cyst suggested intracystic neoplasia. We performed Sistrunk surgical resection and postoperative histopathology showed thyroglossal duct cyst (3.0 cm × 3.0 cm), and papillary thyroid carcinoma (1.5 cm × 1 cm × 0.6 cm) in the cyst wall (Figure 3A). Immunohistochemical results were cytokeratin 19 (CK19) (+), Hector Battifora mesothelial-1 (HBME1) (+), galectin 3 (+), cluster of differentiation 56 (CD56) (−), p53 (−), TTF-1 (+), Ki-67 (5%+) (Figure 3B-3D).
The patient was informed of the pathological findings in detail, and two options for further treatment were discussed with her. The first option was total thyroidectomy, postoperative radioactive iodine ablation, and lifelong thyroxine tablets. The second option was close observation and follow-up without additional surgical treatment. The patient had no high-risk factors and a low risk of recurrence. After full communication, the patient chose the second option and during a 12-month follow-up there were no signs of recurrence through regular postoperative cervical ultrasound and thyroid hormones surveillance every 6 months.
All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Since Brentano reported the first case of carcinoma within a thyroglossal duct cyst in 1911, it has been an extremely rare condition (8). In the low number of cases reported to date combined with the varying total number of thyroglossal duct cysts studied, the incidence of malignancy in thyroglossal duct cysts varies. The reported incidence of thyroid cancer in thyroglossal duct cysts is 1% (9). To date, approximately 300 cases of thyroglossal duct cyst carcinoma have been described in the English literature, mainly single case reports and small case series (10). Common histopathological types are papillary carcinoma (80%), follicular carcinoma (8%), and squamous cell carcinoma (6%), with Hurthle cell adenoma and anaplastic carcinoma as the remaining 6% (11).
There is considerable controversy over origins, which gives rise to different theories for surgical approaches. As possible embryological remnants of thyroid tissue located in thyroglossal duct cysts and possible malignant transformation, the first theory proposes that carcinoma reappears from the cyst and that ectopic thyroid tissue might develop malignancy independently of the native thyroid (8). There is no parafollicular cells in ectopic thyroid tissue. So far, no case of medullary carcinoma in thyroglossal duct cyst has been published, which supports this theory. Based on this theory, Sistrunk surgery may be a satisfactory treatment. The second theory, proposed by Crile in 1947, is that carcinoma forms by metastases from primary occult thyroid tumors (12). If this hypothesis is true, it would prompt thyroidectomy at the time of the Sistrunk procedure, given the embryological mechanism of the thyroid and the remaining unlocked channel as a natural pathway for cancer extension to the cyst (13).
Thyroglossal duct cyst is the most common diagnosis for midline cystic neck swelling; other differential diagnoses include thyroid pyramidal lobes, Delphian lymph node metastatic carcinoma, branchial cleft cyst, epidermoid and dermoid cysts, cervical lymph node tuberculosis, deep cervical hemangioma, cervical lymphangioma, mouth floor dermoid cyst and other diseases. Although uncommon, the initial evaluation should always include the possible presence of ectopic thyroid and thyroglossal duct cyst carcinoma. A survey of preoperative examinations for thyroglossal duct cyst by an expert panel of otolaryngology in the United Kingdom showed that the most commonly requested examination was ultrasonography (95%), thyroid function tests (32%), radioisotope scan (3%), fine needle aspiration (FNA; 2%) and CT (1%) (14). Although thyroglossal duct cyst can usually be diagnosed by ultrasound; preoperative imaging examination can be performed to determine the anatomy, extent of the cyst, identify ectopic thyroid tissue, and evaluate potential malignancy within the cyst. CT and magnetic resonance imaging (MRI) can show solid components, mural nodules, or calcifications within the cystic neck mass, which may help identify cancer within a thyroglossal duct cyst. Approximately 33–62% of patients with ectopic thyroid tissue may develop hypothyroidism with increased TSH levels (15,16). Radionuclide (99mTc, iodine-123 or iodine-131) can be used to identify thyroid tissue, either in the normal or ectopic thyroid bed. However, normal thyroid can capture most of the radionuclide, so it is difficult to identify small ectopic thyroid tissue. FNA diagnosis is not conclusive, as malignant cells are usually relatively few. Due to undersampling, it may only be diagnostically helpful in some situations. FNA reports of thyroglossal duct cyst carcinoma have a true positive rate of 53% and a false negative rate of 47% (17). Thyroglossal duct carcinoma often arises in the absence of obvious abnormalities within the thyroid or cervical lymph nodes. Intracystic carcinoma is usually an accidental result of histopathological evaluation of the resected cyst.
The classic Sistrunk surgery began to be performed in 1920, and comprises resection of the thyroglossal duct cyst, fistula tract, middle segment of the hyoid bone and surrounding tissue of the tongue muscle (18). At present, Sistrunk surgery has become the standard surgical treatment for thyroglossal duct cyst and can reduce the recurrence rate to 3% (19). As malignancies in thyroglossal duct cysts are rarely identified preoperatively, most thyroglossal duct carcinomas are initially treated surgically as benign tumor. There is no clear consensus on the further management after initial resection, particularly the role of total thyroidectomy and postoperative radioactive iodine therapy. There are proponents of aggressive treatment in this situation, but this strategy will cause patients (usually young people) to suffer lifelong sequelae. Consistent with differentiated carcinomas of the thyroid itself, the concept of prognostic risk group (20) is equally relevant for thyroglossal duct cyst carcinoma, and treatment decisions can be adjusted accordingly.
For low-risk patients, only Sistrunk surgery is recommended: (I) <45 years old and no history of low-dose neck irradiation in childhood; (II) clinically or radiologically normal thyroid; and (III) small tumors (<1–1.5 or <4 cm, depending on the different study series), without histologically positive margins, cyst wall invasion, or metastatic lymph node spread (21). For high-risk patients (>45 years old, tumors >4 cm, soft tissue extension, distant metastases) and those with clinically or radiologically abnormal regional lymph nodes, more aggressive management is needed, including excision of thyroglossal duct cyst, total thyroidectomy and selective radioactive iodine therapy. Patel et al. analyzed 57 cases of well-differentiated thyroid cancer within thyroglossal duct cysts, and showed that the only significant predictor of overall survival was the completeness of thyroglossal duct cyst resection, and additional thyroidectomy after Sistrunk procedure had no significant effect on the prognosis of papillary thyroid carcinoma (22). De Sousa Machado et al. performed Sistrunk surgery for the similar low-risk thyroglossal duct cyst carcinoma with no other surgical procedures, and the patient also did not relapse during the 1-year follow-up (23).
Another controversial issue in management is regional lymph node metastasis and its treatment. It has been reported that cervical lymph node metastasis of papillary thyroid carcinoma in thyroglossal duct cyst is ~7–15%. Prophylactic lateral neck dissection is not routinely recommended in the absence of detectable lymph node metastases (24). However, Choi et al. (25) analyzed 163 cases of thyroglossal duct cyst carcinomas reported from 1990 to 2012 and found that 36% had papillary thyroid cancer in the thyroid. Of the 52 patients who underwent neck dissection, 69% had cervical lymph node involvement. Although the reported follow-up period was short (median 12 years) and the number of patients was small, the prognosis of papillary thyroid carcinoma in the thyroglossal duct appears to be similar to that of in thyroid. Mortality of the disease is low, with only a few disease-related deaths reported (26). The overall prognosis of papillary thyroid carcinoma in the thyroglossal duct is good, and the 5- and 10-year Kaplan-Meier overall survival rates are 100% and 95.6% respectively (22). Suresh et al. (27) analyzed 30 cases of thyroglossal duct cyst carcinoma, found that prognostic factors such as extracapsular expansion or lymph node metastasis did not affect overall survival. Nevertheless, thyroidectomy and neck dissection are still required for high-risk patients.
The Sistrunk operation was performed in this case, and the postoperative pathology confirmed that the capsule was intact and the papillary thyroid carcinoma showed no external invasion. Cervical ultrasound and enhanced CT showed no obvious space-occupying lesions in the thyroid, and no obvious enlarged lymph nodes on both sides of the neck. Because this case was judged to be low-risk according to the classification of papillary thyroid carcinoma, and combined with the patient’s personal preferences, no secondary operation was performed (thyroidectomy or radioactive iodine treatment), and only close follow-up was performed. By reporting this case, we hope to inform surgeons of the various abnormalities that may occur in ectopic thyroid malignancies, thereby improving the efficiency of diagnosis and treatment. Because the disease is relatively uncommon and uniform treatment guidelines are lacking, we recommend tailoring individualized treatment based on individual risk stratification.
Conclusions
We report a case of papillary thyroid carcinoma arising from a thyroglossal duct cyst, a rare disease with few cases published in the literature. There are many controversies about the origin of the tumor and the scope of surgery required, which makes many aspects related to its management and follow-up difficult. Individualized treatment is the best option to improve the prognosis of patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-23-102/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-102/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-23-102/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gordini L, Podda F, Medas F, et al. Tall cell carcinoma arising in a thyroglossal duct cyst: A case report. Ann Med Surg (Lond) 2015;4:129-32. [Crossref] [PubMed]
- Naik K. Redefining anatomy in a case of midline subhyoid ectopic thyroid. Indian J Surg 2014;76:333-5. [Crossref] [PubMed]
- Murali S, Nagasundaram J, Raghunandhan S, et al. Papillary carcinoma in a supra hyoid thyroglossal duct cyst - an unusual presentation. Indian J Otolaryngol Head Neck Surg 2009;61:82-5. [Crossref] [PubMed]
- His W. Der Tructus thyroglossus und seinen Beziehungen zum Zungenbein. Arch Anatomie Physiolog (Anatomische Abteilung) 1891:26-32.
- Allard RH. The thyroglossal cyst. Head Neck Surg 1982;5:134-46. [Crossref] [PubMed]
- Organ GM, Organ CH Jr. Thyroid gland and surgery of the thyroglossal duct: exercise in applied embryology. World J Surg 2000;24:886-90. [Crossref] [PubMed]
- Jain A, Pathak S. Rare developmental abnormalities of thyroid gland, especially multiple ectopia: A review and our experience. Indian J Nucl Med 2010;25:143-6. [PubMed]
- Brentano H. Struma aberrata lingual mit druzen metastasen. Dtsch Med Wochenschr 1911;37:665-6.
- Chow TL, Lee CKL. Be wary about occult metastasis to cervical level I lymph node from a case of thyroglossal duct cyst carcinoma. Surg Pract 2022;26:211-3. [Crossref]
- Alqahtani SM, Rayzah M, Al Mutairi A, et al. Papillary carcinoma arising from a thyroglossal duct cyst: A case report and literature review. Int J Surg Case Rep 2022;94:107106. [Crossref] [PubMed]
- Hebbar K A. Papillary carcinoma in median aberrant thyroid (ectopic) - case report. J Clin Diagn Res 2014;8:QD01-3. [Crossref]
- Crile G Jr. Papillary carcinoma of the thyroid and lateral cervical region; so called lateral aberrant thyroid. Surg Gynecol Obstet 1947;85:757-66. [PubMed]
- Sistrunk WE. Technique of removal of the cysts and sinuses of the thyroglossal duct. Surg Gynecol Obst 1928;46:109-12.
- Joseph J, Lim K, Ramsden J. Investigation prior to thyroglossal duct cyst excision. Ann R Coll Surg Engl 2012;94:181-4. [Crossref] [PubMed]
- Toso A, Colombani F, Averono G, et al. Lingual thyroid causing dysphagia and dyspnoea. Case reports and review of the literature. Acta Otorhinolaryngol Ital 2009;29:213-7. [PubMed]
- Di Benedetto V. Ectopic thyroid gland in the submandibular region simulating a thyroglossal duct cyst: a case report. J Pediatr Surg 1997;32:1745-6. [Crossref] [PubMed]
- Thompson LDR, Herrera HB, Lau SK. Thyroglossal Duct Cyst Carcinomas: A Clinicopathologic Series of 22 Cases with Staging Recommendations. Head Neck Pathol 2017;11:175-85. [Crossref] [PubMed]
- Sistrunk WE. The surgical treatment of cysts of the thyroglossal tract. Ann Surg 1920;71:121-2.2.
- Peres C, Rombo N, Guia Lopes L, et al. Thyroglossal Duct Cyst Carcinoma With Synchronous Thyroid Papillary Carcinoma: A Case Report and Literature Review. Cureus 2022;14:e28570. [Crossref] [PubMed]
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Plaza CP, López ME, Carrasco CE, et al. Management of well-differentiated thyroglossal remnant thyroid carcinoma: time to close the debate? Report of five new cases and proposal of a definitive algorithm for treatment. Ann Surg Oncol 2006;13:745-52. [Crossref] [PubMed]
- Patel SG, Escrig M, Shaha AR, et al. Management of well-differentiated thyroid carcinoma presenting within a thyroglossal duct cyst. J Surg Oncol 2002;79:134-9; discussion 140-1. [Crossref] [PubMed]
- De Sousa Machado A, Dias D, Silva A, et al. Papillary carcinoma within thyroglossal duct cyst: A rare midline coexistence. Cureus 2022;14:e31906. [Crossref] [PubMed]
- Tharmabala M, Kanthan R. Incidental thyroid papillary carcinoma in a thyroglossal duct cyst - management dilemmas. Int J Surg Case Rep 2013;4:58-61. [Crossref] [PubMed]
- Choi YM, Kim TY, Song DE, et al. Papillary thyroid carcinoma arising from a thyroglossal duct cyst: a single institution experience. Endocr J 2013;60:665-70. [Crossref] [PubMed]
- Vassilatou E, Proikas K, Margari N, et al. An adolescent with a rare midline neck tumor: thyroid carcinoma in a thyroglossal duct cyst. J Pediatr Hematol Oncol 2014;36:407-9. [Crossref] [PubMed]
- Suresh S, Vm P, Thomas S, et al. Papillary thyroid carcinoma arising from thyroglossal cyst-an institutional experience over a decade. Indian J Surg Oncol 2023;14:155-9. [Crossref] [PubMed]
(English Language Editor: K. Brown)


