
Ascending colon metastasis after breast cancer surgery: a case report and literature review
Highlight box
Key findings
• Gastrointestinal metastasis of breast cancer is rare, but it still needs clinicians’ attention.
What is known and what is new?
• Digestive tract metastasis from breast cancer is lack of specificity of clinical manifestations and endoscopic examination.
• Immunohistochemical staining is helpful to differentiate digestive tract metastasis of breast cancer.
What is the implication, and what should change now?
• In the follow-up after breast cancer surgery, if alimentary tract space occupying lesions are found, relevant immunohistochemical staining should be performed to exclude the possibility of breast cancer metastasis.
Introduction
Breast cancer is the malignant tumor with the highest incidence rate in women, and it is increasing year by year (1,2). The most common organ for distant metastasis are the bones (59.9%), lung (47.8%), liver (40.9%), and brain (38.8%) (3). However, metastasis to the gastrointestinal tract (GIT) is uncommon in breast cancer (4,5), Mclemore’s retrospective review of 12,001 cases of metastatic breast cancer between 1985 and 2000, the result confirmed 73 patients (0.6%) with a pathological affirmation of metastasis to GIT and/or peritoneum. Only 24 out of 12,001 patients (0.2%) had colonic metastasis (6). Montagna and colleagues’ review of 2,588 patients with breast cancer revealed that 40 patients (1.55%) had GIT metastasis, with only 2 having colonic metastasis (0.07%) (7). Those studies show that GIT metastasis is extremely rare in breast cancer.
We report the case of a patient with “ascending colon metastasis”, after breast cancer surgery ten years ago. We also conducted a retrospective analysis of relevant case reports and analyses. We found that because breast cancer with gastrointestinal metastasis rarely occurs, it is easily misdiagnosed, and because of the lack of specificity of its clinical manifestations, it is easily missed, both of which have a great effect on the survival and prognosis of patients.
Colon metastasis of breast cancer is relatively rare, and the prognosis of such patients is very poor, and most of them die within 2 years of their diagnosis, which may be related to other distant organ metastasis and/or delayed diagnosis.
At present, there is no definite consensus or guidelines to the treatment of digestive tract metastasis after breast cancer surgery. Chemotherapy, targeted therapy, and endocrine therapy are the main treatment measures for patients with digestive tract metastasis of breast cancer, and surgical treatment cannot improve the overall survival and prognosis of patients. Only a few patients are eligible for palliative surgery if they have symptoms of digestive tract obstruction (8,9).
Thus, early detection and effective systemic treatment may help to avoid unnecessary surgery and improve prognosis. We present the following article in accordance with the CARE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-642/rc).
Case presentation
The 67-year-old patient first came to our hospital 10 years ago. She had an operation at the local hospital because of “progressive enlargement of a right breast tumor for 1 year”, and underwent “resection of the right breast tumor”. The postoperative pathological return was “invasive ductal carcinoma”, and she was transferred to our hospital for “modified radical mastectomy for right breast cancer”. The postoperative pathology was “(modified radical mastectomy specimen of the right breast) no tumor residue was found around the original surgical incision of the right breast, and no tumor was involved in the papillary skin, epidermis, and basal connective tissue. No cancer metastasis was found in 23 lymph nodes. The results were as follows: right armpit 0/18, subclavian 0/2, and tip group 0/3”. The immunohistochemistry (IHC) results were as follows: estrogen receptor (ER) (+++), progesterone receptor (PR) (±), human epidermal growth factor receptor 2 (HER-2) (–). After the operation, a chemotherapy regimen of epirubicin + cyclophosphamide (EC) was administered for 6 cycles. Tamoxifen endocrine therapy was administered after chemotherapy.
The patient had a regular follow-up, with all surveillance scans being negative for distant metastasis and local recurrence. The patient went to outpatient department in 2020-08-21, and endoscopic examination found no suspicious lesion (Figure 1A,1B).

The patient visited our hospital on May 5, 2021 because of “acute pain in the right lower abdomen”. A physical examination revealed pain in the right lower abdomen. After an abdominal plain scan CT examination (patients in emergency room usually only receive plain CT examination, unless suspected of vascular disease), the patient was diagnosed with acute appendicitis and underwent laparoscopic appendectomy (LA). There was no abdominal and pelvic cavity contamination due to tumor rupture during operation. Simple inflammatory changes were observed in the appendix (Figure 2), and the ileocecal part and the visible part of the abdominal cavity had no obvious abnormalities. A LA was performed.

The patient’s postoperative pathological report was as follows: a large number of heterotypic cells were observed in the wall of the appendix and mesangium, arranged in the form of cords and glandular tubes, and tumor thrombi were observed in the vessels. Combined with the immunohistochemistry results and the patient’s history, the pathological results was consistent with non-specific invasive cancer metastasis of the breast, and cancer involvement was observed at the cutting edge. The IHC results were as follows: ER (95% strongly positive), PR (15% strongly positive), HER-2 (+), E-cad (+), p120 (membrane +), GATA-3 (trans-acting T-cell-specific transcription factor) (+), gross cystic disease fluid protein-15 (GCDFP-15) (focus +), mammaglobin (focus +), cytokeratin-7 (CK7) (+), cytokeratin-20 (CK20) (–). The Ki-67 index was about 20% (Figure 3A-3D).

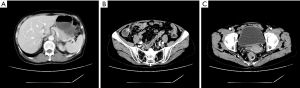
After LA, the patient underwent abdominal enhanced CT, and no abnormal signs, such as the thickening of the colon wall, were observed (Figure 4A-4C). The patient refused an endoscopy and positron emission tomography-CT (PET/CT), and then underwent laparoscopic radical right hemicolectomy.
The patient’s postoperative pathological result of the right hemicolectomy specimen indicated a diagnosis of metastatic non-specific invasive breast cancer. The tumor showed multifocal metastatic invasion. The small foci showed the involvement of the muscularis propria of the intestinal wall. The tumor thrombi in the vessels were visible. The nerve invasion was not obvious. No cancer was found in the bilateral cutting ends of the specimen, and the “upper cutting end” and “lower cutting end”. There were 37 lymph nodes without cancer metastasis. The IHC results were as follows: GATA-3 (+++), GCDFP-15 (focus +), ER (95%, strong +), PR (5%, medium), HER-2 (1+), E-cad (membrane ++), p120 (membrane ++), CK7 (+++), CK20 (–), satb-2 (–), villin (–), syn (–), chromophilic granulin A (CGA) (–), and CD56 (–). The Ki-67 index was about 5%.
The patient recovered well after the right hemicolectomy, but she refused to any kind of further treatment, and regular follow-up. 1 year after operation in patients with reviewing a colonoscopy and CT examinations are not prompted to tumor recurrence (Figure 5A-5F). The patient’s diagnosis and treatment timeline was summarized in Figure 6.

Colon metastasis of breast cancer is relatively rare, and the prognosis of such patients is very poor. The main reasons are the long interval between tumor recurrence, the lack of specific clinical symptoms, and the lack of experience of the receiving doctor. The patients with digestive tract metastasis of breast cancer usually have no specific symptoms, as we summarized in Table 1, the most common symptoms include dyspepsia, nausea, changes of stool frequency (10), vomiting (11), abdominal pain (12), obstruction (13), loss of weight (14), and loss of appetite (20). Some were found during regular follow-up (15-19). Endoscopic findings are non-specific (21-23). It is often difficult for patients to obtain an accurate diagnosis because of these non-specific symptoms.
Table 1
| Case | Time from diagnosis (year) | Treatment | Survival |
|---|---|---|---|
| Higley et al. (10) | 38 | Chemotherapy | Alive |
| Noor et al. (11) | 30 | Surgical resection | Alive |
| Blachman-Braun et al. (12) | 15 | Surgical resection | Alive |
| Katz et al. (13) | 15 | Right hemicolectomy | Unclear |
| Algethami et al. (14) | 1 | Unclear | Unclear |
| Do et al. (15) | 7 | Palliative care | Alive |
| Schellenberg et al. (16) | 2 | Biopsy surgery | Dead |
| Falco et al. (17) | 12 | Right hemicolectomy | Alive |
| Jones et al. (18) | 4 | Laparoscopic appendectomy | Alive |
| Imai et al. (19) | 2 | Unclear | Unclear |
Ambroggi et al. (20) conducted a retrospective analysis of more than 200 cases of breast cancer patients with gastrointestinal metastasis, and found that the most common sites of breast cancer metastasis were the stomach (60%), esophagus (12%), colon (11%), rectum (8%), and oropharynx (1%). A retrospective analysis of 12,000 cases of metastatic breast cancer patients at the Mayo Clinic showed that only 73 of those patients suffered from gastrointestinal metastasis during the follow-up, of whom 8% had esophageal metastasis, 28% had gastric metastasis, 19% had intestinal metastasis, and 45% had colorectal metastasis. Among the breast cancer patients with gastrointestinal metastasis, about 54% had the pathological type of invasive lobular carcinoma (24).
At present, there is no definite consensus or guiding opinions on the treatment of digestive tract metastasis after breast cancer surgery. Chemotherapy, targeted therapy, and endocrine therapy are the main treatment measures for patients with digestive tract metastasis of breast cancer, and surgical treatment cannot improve the overall survival and prognosis of patients. Only a few patients are eligible for palliative surgery if they have symptoms of digestive tract obstruction (8,9,25).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Colon metastasis of breast cancer is relatively rare, and the prognosis of such patients is very poor. The main reasons are the long interval between tumor recurrence, the lack of specific clinical symptoms, and the lack of experience of the receiving doctor. The patients with digestive tract metastasis of breast cancer usually have no specific symptoms. Endoscopic findings are non-specific (21-23). It is often difficult for patients to obtain an accurate diagnosis because of these non-specific symptoms.
For patients suspected that digestive tract lesions may be metastatic from breast cancer, it is important to improve the biopsy and IHC stain of the lesions. GCDFP-15, mammaglobin, and GATA3 are relatively specific antibodies in the breast, and their combined application is helpful to determine the source of tumor cells.
We also summarized and compared the immunohistochemical detection indicators of digestive tract metastasis of breast cancer, and selected the immunohistochemical detection indicators with high sensitivity and specificity. GCDFP-15, mammaglobin, and GATA3are relatively specific antibodies in the breast, and their combined application is helpful to determine the source of tumor cells. Due to the diversity of the tumor histological types, the different immunophenotypes, the differences in the expression of primary and metastatic lesions, the differences in detection methods, and the differences in statistical methods, reports on the sensitivity and specificity of the expression of the above-mentioned 3 antibodies in breast cancer vary greatly. Notably, GCDFP-15 has a sensitivity of 5–74% and a specificity of 9–100%, mammaglobin has a sensitivity of 7–84% and a specificity of 85–100%, and GATA3 has a sensitivity of 32–100% and a specificity of 71–93%. ER and PR can also be expressed in primary gastric tumors. However, it is not recommended that they be used alone as immunohistochemical markers to determine the origin of tumors (26). In this case, the negative postoperative pathology immunohistochemical results for CK-20 and Cdx-2 for this patient largely excluded the presence of primary gastrointestinal tumors, and the positive results of CK-7, GATA-3, mammaglobin, and ER largely supported the presence of metastatic breast cancer.
At present, there is no definite consensus or guiding opinions on the treatment of digestive tract metastasis after breast cancer surgery. Chemotherapy, targeted therapy, and endocrine therapy are the main treatment measures for patients with digestive tract metastasis of breast cancer, and surgical treatment cannot improve the overall survival and prognosis of patients. Only a few patients are eligible for palliative surgery if they have symptoms of digestive tract obstruction (8,9,25).
The early detection and timely and effective systemic treatment may help to improve prognosis. Thus, doctors treating patients with a history of breast cancer should be alert to the possibility of metastasis when gastrointestinal symptoms are observed. Additionally, in the clinical follow-up of patients with breast cancer, regular endoscopic examination are essential, especially when patients have gastrointestinal symptoms, such as a loss of appetite, nausea, vomiting, abdominal pain and discomfort, and changes in bowel habits. For abnormal lesions detected under endoscopy, whether ulcer or polypoid hyperplasia, a pathological examination and immunohistochemical examination should be carried out to avoid delay in diagnosis and treatment.
Conclusions
The combination of a long interval from initial diagnosis of breast cancer to the presentation and the rarity of isolated colonic metastases makes the diagnosis of colonic metastases difficult and easily missed.
There are no certain guideline on how to manage colonic metastasis from breast cancer; however, surgical resection was not guarantee to improve the survival of patients with GIT metastasis and/or carcinomatosis over chemotherapy and/or hormonal therapy. So surgical procedure should only be considered in the case of life-threatening complications (e.g., to treat bleeding, obstruction, and perforation) (6).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-642/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-642/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. [Crossref] [PubMed]
- Chen W, Zheng R. Incidence, mortality and survival analysis of breast cancer in China. Chinese J Clin Oncol 2015;42:668-74.
- Xiao W, Zheng S, Yang A, et al. Breast cancer subtypes and the risk of distant metastasis at initial diagnosis: a population-based study. Cancer Manag Res 2018;10:5329-38. [Crossref] [PubMed]
- Jansen van Rensburg A, Riddell A. A case report of ductal carcinoma of the breast metastasizing to the bowel. J Surg Case Rep 2021;2021:rjab471. [Crossref] [PubMed]
- Kobayashi M, Tashima T, Nagata K, et al. Colorectal and gastric metastases from lobular breast cancer that resembled superficial neoplastic lesions. Clin J Gastroenterol 2021;14:103-8. [Crossref] [PubMed]
- Washington K, McDonagh D. Secondary tumors of the gastrointestinal tract: surgical pathologic findings and comparison with autopsy survey. Mod Pathol 1995;8:427-33.
- Montagna E, Pirola S, Maisonneuve P, et al. Lobular Metastatic Breast Cancer Patients With Gastrointestinal Involvement: Features and Outcomes. Clin Breast Cancer 2018;18:e401-5. [Crossref] [PubMed]
- Rodrigues MV, Tercioti-Junior V, Lopes LR, et al. Breast cancer metastasis in the stomach: when the gastrectomy is indicated? Arq Bras Cir Dig 2016;29:86-9. [Crossref] [PubMed]
- Alabd A, Mok SRS. Multilevel stenting of malignant colonic obstructions from multilevel breast cancer colonic metastasis. VideoGIE 2022;7:152-3. [Crossref] [PubMed]
- Higley C, Hsu A, Park BU, et al. Back to Basics: History and Physical Examination Uncover Colonic Metastasis in a Patient With Remote History of Breast Cancer. ACG Case Rep J 2020;7:e00494. [Crossref] [PubMed]
- Noor A, Lopetegui-Lia N, Desai A, et al. Breast Cancer Metastasis Masquerading as Primary Colon and Gastric Cancer: A Case Report. Am J Case Rep 2020;21:e917376. [Crossref] [PubMed]
- Blachman-Braun R, Felemovicius I, Barker K, Kehrberg E, Khan F. Widespread metastatic breast cancer to the bowel: an unexpected finding during colonoscopy. Oxf Med Case Reports 2019;2019:omy133. [Crossref] [PubMed]
- Katz H, Jafri H, Saad R, et al. Colonic Obstruction from an Unusual Cause: A Rare Case of Metastatic Invasive Ductal Carcinoma to the Colon. Cureus 2018;10:e2588. [Crossref] [PubMed]
- Algethami NE, Althagafi AA, Aloufi RA, et al. Invasive Lobular Carcinoma of the Breast With Rectal Metastasis: A Rare Case Report. Cureus 2022;14:e23666. [Crossref] [PubMed]
- Do JE, Ganguly T, Chang S, et al. Metastatic Infiltrating Lobular Breast Cancer to the Colon Diagnosed Through Routine Bowel Screening in a 67-Year-Old Female. Cureus 2022;14:e29279. [Crossref] [PubMed]
- Schellenberg AE, Wood ML, Baniak N, et al. Metastatic ductal carcinoma of the breast to colonic mucosa. BMJ Case Rep 2018;2018:bcr2018224216. [Crossref] [PubMed]
- Falco G, Mele S, Zizzo M, et al. Colonic metastasis from breast carcinoma detection by CESM and PET/CT: A case report. Medicine (Baltimore) 2018;97:e10888. [Crossref] [PubMed]
- Jones A, Kocher MR, Justice A, et al. Colonic metastasis from infiltrating ductal breast carcinoma in a male patient: A case report. Int J Surg Case Rep 2019;54:34-8. [Crossref] [PubMed]
- Imai J, Hanamura T, Kawanishi A, et al. A case of breast cancer with extensive colon metastasis. DEN Open 2023;3:e189. [Crossref] [PubMed]
- Ambroggi M, Stroppa EM, Mordenti P, et al. Metastatic breast cancer to the gastrointestinal tract: report of five cases and review of the literature. Int J Breast Cancer 2012;2012:439023. [Crossref] [PubMed]
- Jones GE, Strauss DC, Forshaw MJ, et al. Breast cancer metastasis to the stomach may mimic primary gastric cancer: report of two cases and review of literature. World J Surg Oncol 2007;5:75. [Crossref] [PubMed]
- Abid A, Moffa C, Monga DK. Breast cancer metastasis to the GI tract may mimic primary gastric cancer. J Clin Oncol 2013;31:e106-7. [Crossref] [PubMed]
- Inoue H, Arita T, Kuriu Y, et al. Colonic Metastasis from Breast Cancer: A Case Report and Review of the Literature. In Vivo 2022;36:522-7. [Crossref] [PubMed]
- McLemore EC, Pockaj BA, Reynolds C, et al. Breast cancer: presentation and intervention in women with gastrointestinal metastasis and carcinomatosis. Ann Surg Oncol 2005;12:886-94. [Crossref] [PubMed]
- Bolzacchini E, Nigro O, Inversini D, et al. Intestinal metastasis from breast cancer: Presentation, treatment and survival from a systematic literature review. World J Clin Oncol 2021;12:382-92. [Crossref] [PubMed]
- Gown AM, Fulton RS, Kandalaft PL. Markers of metastatic carcinoma of breast origin. Histopathology 2016;68:86-95. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)



