
The efficacy and safety of acupuncture and moxibustion for breast cancer lymphedema: a systematic review and network meta-analysis
Highlight box
Key findings
• Acupuncture combine with moxibustion has the best effect in BCL.
What is known and what is new?
• Many studies have shown that acupuncture has a good effect on BCL. However, it is not known whether different acupuncture treatments have different curative effects.
• This study compared the efficacy of different acupuncture, determine which acupuncture is likely to be the best intervention.
What is the implication, and what should change now?
• The discovery of new evidence of acupuncture treatment of BCL can guide clinical treatment. Acupuncture combined with moxibustion is the most effective in reducing arm circumference, and acupuncture (face) is the greatest analgesic effect.
Introduction
Breast cancer is one of the most common cancers in women, and represents a serious threat to women’s health. According to reports, there were 2.089 million new cases of breast cancer worldwide in 2020, and with an incidence rate of 24.2%, breast cancer ranks first among female cancers (1). The latest data on global cancer shows that in 2020, breast cancer surpassed lung cancer to become the cancer with the highest incidence rate in the world, and its incidence continues to increase (2).
Surgery is currently the most effective way to treat early- and mid-stage breast cancer. However, complications related to surgical treatments may arise. Breast cancer lymphedema (BCL) (3) is one of the most common complications after breast cancer surgery. The surgical removal of the axillary lymph nodes destroys the lymphatic system and blood vessels, affecting the normal return of lymphatic vessels, causing protein-rich lymph fluid to accumulate in the interstitial spaces. Pain, limited mobility, and impaired limb function seriously affect the quality of life of patients (4). The incidence of BCL has been reported to range from 13.5% to 41.2%, and increases with the number of lymph nodes removed (5). Axillary dissection, chemotherapy, and radiotherapy significantly increase BCL’s severity (5,6).
Western medical treatment for BCL mainly includes the following 4 approaches: lymphatic drainage, bandage, rehabilitation exercise, and skin care. However, clinical observations have revealed that the effect of such treatment is not good, and it was easy to recur (7).
Acupuncture and moxibustion are important therapies in traditional Chinese medicine (TCM). Acupuncture refers to inserting specifically-designed needles into patients’ skin and the underlying tissues at a certain angle, and exerting manipulation to stimulate specific sites of the body, so as to treat diseases. The inserting sites are acupoints. Moxibustion refers to using prefabricated moxa cones or sticks, which exert warm stimulation on the acupoints to prevent or treat diseases. There are various acupuncture and moxibustion modalities, including manual acupuncture, ignipuncture, electroacupuncture, moxibustion, on-salt moxibustion, acupuncture-moxibustion combination therapy, acupoint application. Acupuncture is widely used to treat BCL, and it is effective in reducing swelling, pain relief, and improving patients’ quality of life. Numerous meta-analyses have shown that acupuncture has good efficacy and safety in the treatment of BCL (8-10).
A study has shown that local acupuncture could promote blood circulation in the edema sites of the upper limb, cause accumulation of inflammatory cells, and accelerate local metabolism, so as to attenuate the edema (11). The stimulative effect of acupuncture leads to re-dilation of lymphatic vessels that are closed due to being damaged, especially micro-vessels that are crucial to lymphatic return. After the re-dilation, various immune cells are activated, which could help limit the inflammatory response in the process of wound healing, down-regulate the release and accumulation of multiple celluloses, reduce the inter-tissue adhesion within the shoulder joint, and improve its mobility and function. Warm stimulation caused by moxibustion or ignipuncture could effectively alleviate the pain and promote recovery of the disease (12).
However, there are multiple modalities of acupuncture and moxibustion, with different manipulating difficulty levels and costs, as well as the efficacy and safety. Currently published clinical trials comparing different acupuncture and moxibustion modalities have revealed differences in the efficacy among different modalities. For example, Yang et al. (13), has reported that ignipuncture is more effective than conventional acupuncture, while study by Zeng et al. (14), has shown that acupuncture (face) would be more effective than the conventional acupuncture. However, it remains unclear which of the two modalities would be better. Selection of proper acupuncture and moxibustion modalities is helpful to improve the therapeutic effects and save treatment costs, so as to reduce clinicians’ workload and alleviate burden on the patients. Compared with conventional meta-analysis, network meta-analysis could provide comparisons among different interventions for one certain disease, and perform quantitative analyses to assess and rank the efficacy of these interventions (15). Therefore, this study applies network meta-analysis to compare and rank different acupuncture and moxibustion modalities, so as to identify the most effective acupuncture and moxibustion modality and provide reference for clinical practice. We present the following article in accordance with the PRISMA-NMA reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-767/rc).
Methods
Registration
This study was registered on PROSPERO (No. CRD42022357173).
Inclusion criteria
To be eligible for inclusion in this study, the articles had to meet the following inclusion criteria: (I) study type: randomized controlled trials (RCTs). There are no restrictions on publication time or region; (II) patients diagnosed with BCL according to relevant diagnostic criteria (16,17). Notably, there were no restrictions on race, nationality, age, gender, or course of disease; (III) interventions: acupuncture. Because acupuncture and moxibustion are usually used in combination, the combined use of acupuncture and moxibustion is considered as an intervention; (IV) control: acupuncture (different from the intervention group); (V) outcome indicators: arm circumference, and safety evaluation (adverse reactions). Secondary outcome measures: visual analogue scale (VAS) (18). Studies that reported on only one of these outcome measures were included in the meta-analysis.
Exclusion criteria
Articles were excluded from the study if they met any of the following exclusion criteria: (I) were duplicate documents; (II) were published in languages other than Chinese and English; (III) concerned non-RCTs (e.g., basic trials, reviews, abstracts, or letters); (IV) the intervention is not acupuncture; (V) studied inconsistent diseases; (VI) had incomplete or incorrect data; (VII) included no mention of the outcome measures examined in the study; (VIII) the included interventions cannot be plotted on the network evidence plot.
Literature search
We searched the PubMed, Web of Science, Embase, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang, VIP, and SinoMed databases for articles published on RCTs examining the use of acupuncture or moxibustion in the treatment of BCL from the inception of the databases until September 30, 2022. The search used subject headings combined with free words. The search terms included “breast cancer lymphedema”, “breast cancer lymphedemas”, “breast cancer treatment related lymphedema”, “breast cancer related arm lymphedema”, “post mastectomy lymphedema”, “acupuncture”, “pharmacopuncture”, “acupuncture treatment”, “acupuncture”, “ear”, “electroacupuncture”, and “moxibustion”. Taking the PubMed search as an example, details of our retrieval strategy are provided in the Appendix 1.
Literature screening and data extraction
Two researchers (S Wang and F Zhang) managed the literature with Endnote and extracted data with Excel according to the inclusion and exclusion criteria. First, the imported articles were screened using Endnote. The titles and abstracts of the articles were then read to exclude any articles that clearly did not meet the inclusion criteria. Finally, the full text was read to select the original studies that were ultimately included in the meta-analysis. If important information was not reported in the original text, an attempt was made to contact the author by telephone or Email. The extracted content included details of the authors, publication date, basic characteristics of the patients, sample size, intervention measures, treatment course, outcome indicators, funding sources, and risk factors of bias (i.e., random method, allocation concealment, and blinding). If there any disagreements arose during this process, a third investigator was consulted (H Tang), and a decision was reached following discussion.
Risk of bias assessment
Two researchers (F Zhang and W Ning) assessed the risk of bias of included studies using the Risk of Bias Assessment Tool 2 (ROB2) recommended in the Cochrane Handbook (19), which contains the following domains: randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported outcome. Each domain could be graded as “low risk of bias”, “some concerns”, and “high risk of bias”. If all the domains are graded as “low risk”, the overall risk of bias is low. If more than one domain is graded as “some concerns” and none of the domains graded as “high risk of bias”, the overall risk of bias is “some concerns”. If more than one domain is graded as “high risk of bias”, the overall risk of bias is high.
Statistical analysis
The network meta-analysis was performed using Stata16’s mvmeta, network packages. If the outcome indicators were dichotomous variables, the relative risk (RR) was used, and if the outcome indicators were continuous variables, the mean difference (MD) was used together with the confidence interval (CI).
A diagram of the evidence network was generated. The size of the dots in the figure indicates the sample size of the intervention, and the thickness of the line indicates the amount of direct evidence between the interventions. If there was a closed loop, an inconsistency model was used to evaluate the degree of consistency between the results of the direct comparison and the indirect comparison. If there was no closed loop, the consistency model was used for the analysis. If the P value was >0.05, the inconsistency was low. If the P value was <0.05, the inconsistencies were reported, and the evaluation results were treated with caution.
The heterogeneity between the studies was assessed. If I2<50%, the heterogeneity among the studies was small, and the fixed-effects model was used for the analysis. If I2≥50%, the random-effects model was used, and sensitivity and subgroup analyses were performed to explore the source of heterogeneity.
The intervention measures for each outcome were ranked by the surface under the cumulative ranking probability area (SUCRA), and the higher the SUCRA value, the better the effect of the intervention. A “comparison-adjusted” funnel plot was generated to identify studies with small-sample effects and publication bias, and Egger’s test was also performed.
Results
Literature search and basic features
The preliminary search yielded 1,044 articles, and after the screening, a total of 7 studies were included (13,14,20-24). All studies were published in the Chinese language. The publication area was China, and the publication years ranged from 2017 to 2022. A total of 422 patients (218 in the intervention group and 204 in the control group) were included in the meta-analysis, all of whom met the diagnostic criteria of BCL The studies included in the meta-analysis examined the following 7 types of acupuncture methods: fire acupuncture, acupuncture (face), moxa-moxibustion, heat-sensitive moxibustion, moxibustion (TCM), acupuncture combine with moxibustion, acupoint application. The outcome indicators included arm circumference, VAS, and safety evaluation (adverse reactions). Figure 1 is a flow chart of the literature screening process. Table 1 presents the basic characteristics of the included literature.
Table 1
| Study | Year | Sample size | Age (years), mean ± SD | Interventions | Time | Outcomes | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| I | C | I | C | I | C | ||||||
| Yang et al. (13) | 2021 | 30 | 30 | 57.73±3.49 | 56.86±3.39 | 1 | 2 | 2 weeks | AC, S | ||
| Zeng et al. (14) | 2021 | 32 | 32 | 53.56±8.15 | 55.44±9.81 | 3 | 2 | 3 weeks | AC, VAS | ||
| Han et al. (20) | 2020 | 20 | 10 | 59.95±4.77 | 62.00±8.76 | 7 | 1 | 7 weeks | AC | ||
| Jiao et al. (21) | 2017 | 15 | 15 | 45.62±3.52 | 45.57±3.50 | 7 | 5 | 9 weeks | AC | ||
| Wang et al. (22) | 2019 | 24 | 24 | 59.42±7.02 | 58.25±6.19 | 4 | 5 | 4 weeks | VAS | ||
| Zhang et al. (23) | 2022 | 77 | 73 | 45.85±4.88 | 45.62±5.01 | 7 | 8 | 4 weeks | AC | ||
| Liu et al. (24) | 2020 | 20 | 20 | 58.62±8.58 | 59.67±5.38 | 6 | 4 | 8 weeks | VAS | ||
Interventions: 1, fire acupuncture; 2, acupuncture (body); 3, acupuncture (face); 4, moxa-moxibustion; 5, heat-sensitive moxibustion; 6, moxibustion (TCM); 7, acupuncture combine with moxibustion; 8, acupoint application. SD, standard deviation; I, intervention group; C, control group; AC, arm circumference; S, safety; VAS, visual analogue scale; TCM, traditional Chinese medicine.
Quality evaluation of the included articles
Five studies applied proper randomization (random number table) (13,14,20,22,23), and 1 study (21) performed randomization of high risk (odd and even numbers). For allocation concealment, 2 studies (14,22) used sealed and light-proof envelopes, and 1 study (20) put the allocation under the management of a certain researcher. As for blinding, all the included studies provided no descriptions regarding the blinding. In 1 study (23), the number of participants was uneven between the two group, so that there might be possibility that the participants were aware of the intervention and chose which group to be assigned. Blinding is generally difficult to be implemented due to complexities of acupuncture therapy. However, the participants were of good treatment compliance, so the absence of blinding would less likely affect the results. Figure 2 shows a graph of the risk of bias assessment of the included studies.
Network meta-analysis
Evidence network
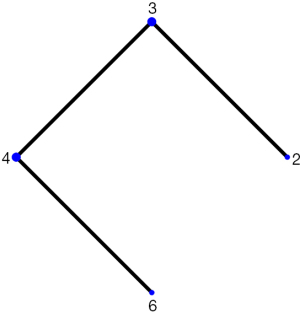
Five studies reported the arm circumference, involving 6 acupuncture and moxibustion modalities. Acupuncture-moxibustion combination therapy was the most commonly used. There was no close loop in the evidence network diagram. The consistency test showed that the consistency was good.
There were 3 studies that reported the VAS, involving 4 interventions. There was no close loop in the evidence network diagram. The consistency test showed that the consistency was good. The evidence network diagrams of outcome measures are shown in Figures 3,4.

Network meta-analysis results
Arm circumference
The overall heterogeneity was small. Network meta-analysis produced 56 pair-wise comparisons, in which 6 were statistically significant. The results showed that compared with heat-sensitive moxibustion, fire acupuncture [MD =−8.02; 95% CI: (−10.55, −5.49); P<0.05], acupuncture (body) [MD =−7.38; 95% CI: (−10.25, −4.51); P<0.05], acupuncture (face) [MD =−7.16; 95% CI: (−10.45, −3.87); P<0.05], acupuncture combined with moxibustion [MD =−8.06; 95% CI: (−10.54, −5.58); P<0.05], and acupoint application [MD =−7.52; 95% CI: (−10.00, −5.04); P<0.05] were effective, acupuncture combined with moxibustion was more effective than acupoint application [MD =−0.54; 95% CI: (−0.67, −0.41); P<0.05]. The SUCRA ranking was: acupuncture combined with moxibustion > fire acupuncture > acupuncture (body), acupoint application > acupuncture (face), and heat-sensitive moxibustion. Acupuncture combined with moxibustion was the most effective.
VAS
The overall heterogeneity was small. Network meta-analysis produced 12 comparisons, in which 1 was statistically significant. The results showed that acupuncture (face) was more effective than acupuncture (body) [MD =−0.85; 95% CI: (−1.09, −0.61); P<0.01]. The SUCRA ranking was: acupuncture (face) > moxibustion (TCM) > moxa-moxibustion > and acupuncture (body). Acupuncture (face) was the most effective in pain-relieving. The forest plots and league table are provided in Appendix 1. Table 2 is the SUCRA ranking.
Table 2
| Interventions | Arm circumference | VAS | |||
|---|---|---|---|---|---|
| SUCRA | Sequence | SUCRA | Sequence | ||
| 1 | 80.6 | 2 | – | – | |
| 2 | 47.9 | 3 | 5.8 | 4 | |
| 3 | 43.2 | 5 | 84.8 | 1 | |
| 4 | – | – | 51.7 | 3 | |
| 5 | 0.0 | 6 | – | – | |
| 6 | – | – | 57.8 | 2 | |
| 7 | 83.5 | 1 | – | – | |
| 8 | 44.8 | 4 | – | – | |
Interventions: 1, fire acupuncture; 2, acupuncture (body); 3, acupuncture (face); 4, moxa-moxibustion; 5, heat-sensitive moxibustion; 6, moxibustion (TCM); 7, acupuncture combine with moxibustion; 8, acupoint application. SUCRA, surface under the cumulative ranking probability area; VAS, visual analogue scale; TCM, traditional Chinese medicine.
Safety evaluation
One study (13) reported 1 case of hematoma caused by acupuncture in the intervention group and 1 case of fainting from acupuncture in the control group. The above symptoms are mild, no special treatment is needed, and patients can recover spontaneously in a short time. These results indicate that acupuncture treatments are safe.
Discussion
Breast cancer is a systemic comprehensive disease. Lymphedema is likely to occur after surgery, which can lead to swelling and pain of the limbs and affect the long-term quality of life of patients. Its risk factors mainly include the surgical methods, postoperative local radiotherapy, and injuries and infections of the upper extremities. There is currently no effective therapy for the treatment of upper extremity lymphedema. Western medicine mainly controls the swelling through the comprehensive treatment of the upper limbs, but the long-term effect is not good, and it is easy to recur. A study has shown that functional exercise can promote strength and muscle gain and reduce the risk of BCL (17). Effective treatment options need to be explored. In China, acupuncture is widely used in the treatment of BCL and has a good curative effect. However, the efficacy of different acupuncture methods is different. Therefore, this study used a network meta-analysis to compare the efficacy of different acupuncture methods, with the aim to provide a reference for clinical practice.
In total, 7 studies were included in this study, and >90% of the articles published in the past 5 years were relatively new. Network meta-analysis showed that acupuncture combined with moxibustion would probably be the most effective modality in reducing arm circumference. A study has shown that acupuncture stimulation could cause a physiological inflammatory response, promote blood circulation in the edema sites of the upper limb, and induce the accumulation of inflammatory cells, to maintain the body homeostasis. It regulates local epidermal and dermal plasma osmotic pressure and accelerates local blood flow to attenuate the edema. The addition of electrostimulation speeds up the systemic blood circulation, improve the lymph fluid flow, and the positive reverse transport of ions inside and outside the tissue. These effects promote the rapid excretion of metabolic waste generated in the life-maintaining processes, and reduce the inflammatory response caused by trauma, thereby effectively alleviating inflammation and edema (25). Burning moxa produces volatile oil that is of antibacterial and bactericidal effects. Its residue could attach to the skin, bringing warm stimulation to exert therapeutic effects (26). Moxibustion produces surrounding warm stimulation through its own heat radiation and light radiation, so as to improve local blood and lymphatic circulation, and accelerate the dissipation and absorption of inflammatory substances. On the other hand, it could improve and enhance immunity to exert anti-infection and analgesic effects. When using the acupuncture-moxibustion combination, the warm stimulation caused by burning moxa could be conducted into the body through acupuncture, which could improve the pain threshold and effectively relieve the pain. This would be of greater recovery effect for the shoulder joint function. The combination of acupuncture and moxibustion could be synergistic, and could yield more remarkable therapeutic effects (27). In reducing the VAS score, SUCRA showed that acupuncture (face) might be the most effective intervention. Acupuncture (face) is theoretically based on holographics. In TCM, the face contains holographic units of the whole body, forming a tiny holographic projection system on the face. It is believed that there is a holographically-targeted correspondence between the disease location and facial acupoints. Facial acupoints could be used to treat diseases all over the body. From the perspective of anatomy, there are trigeminal nerves and facial nerves in the distribution area of facial acupoints. The two cranial nerves respectively control human sensation and movement. Acupuncture stimulation might treat diseases by regulating nerve conduction pathways (28). Basis studies have found that acupuncture (face) exerts an analgesic effect by regulating the release of exogenous and endogenous algogenic substances (29,30). Multiple clinical trials have indicated that acupuncture (face) is of great effect on alleviating acute and chronic pain, visceral pain, bone pain, and cancer pain (31-35). Moreover, it is easier to be performed compared to conventional acupuncture, with lower costs and higher safety. With regard to safety, 1 study reported the safety. However, the patients’ symptoms were mild with no need for intervention, and these symptoms disappeared after a period of time. Clinicians should inform the patients prior to implementation and strive to improve surgical techniques to reduce the risk of adverse events. Based on the current evidence, it can be concluded that acupuncture is of good safety. However, due to a limited number of included studies, the safety needs to be further assessed by more clinical trials.
This study had several limitations. Firstly, some of the included studies had methodological problems in randomization, allocation concealment, and blinding. Future studies should take into more serious consideration the methodological quality, and report the results in strict accordance with the CONSORT principle to improve the quality of the reports and reduce the risk of bias. Secondly, the sample size of each included study was small, which compromised the statistical power of this study. The lack of standardized sample size estimation criteria in each study might affect the validity of the study. Future studies should implement a strict sample size calculation method, and more well-designed clinical trials with a large sample size are needed to provide high-quality evidence for clinical practice. Thirdly, we only searched studies published in Chinese and English, the literature search would be uncomprehensive. Lastly, the number of included studies was limited, which also compromised the validity of this study. More studies performing direct comparisons for different acupuncture and moxibustion modalities should be conducted to identify the most appropriate intervention, and to provide more robust support for clinical practice.
Conclusions
Based on the current evidence, acupuncture and moxibustion is of great efficacy and safety for the treatment of BCL. Acupuncture combined with moxibustion is the most effective in reducing arm circumference, and acupuncture (face) is of the greatest analgesic effect. This deserves more attention and can serve as a reference for clinicians when selecting clinical interventions. The conclusion needs to be further validated by more well-designed trials due to the low methodological quality of the included studies.
Acknowledgments
We would like to thank the researchers and study participants for their contributions.
Funding: This study was funded by the National Natural Science Foundation of China (No. 81360579).
Footnote
Reporting Checklist: The authors have completed the PRISMA-NMA reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-767/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-767/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Cao MM, Chen WQ. Interpretation on the global cancer statistics of GLOBOCAN 2020. Chinese Journal of Medical Frontiers 2021;13:63-9. (Electronic Edition).
- Kilbreath SL, Refshauge KM, Beith JM, et al. Risk factors for lymphoedema in women with breast cancer: A large prospective cohort. Breast 2016;28:29-36. [Crossref] [PubMed]
- Chowdhry M, Rozen WM, Griffiths M. Lymphatic mapping and preoperative imaging in the management of post-mastectomy lymphoedema. Gland Surg 2016;5:187-96. [Crossref] [PubMed]
- Ribeiro Pereira ACP, Koifman RJ, Bergmann A. Incidence and risk factors of lymphedema after breast cancer treatment: 10 years of follow-up. Breast 2017;36:67-73. [Crossref] [PubMed]
- Tobin MB, Lacey HJ, Meyer L, et al. The psychological morbidity of breast cancer-related arm swelling. Psychological morbidity of lymphoedema. Cancer 1993;72:3248-52. [Crossref] [PubMed]
- Quirion E. Recognizing and treating upper extremity lymphedema in postmastectomy/lumpectomy patients: a guide for primary care providers. J Am Acad Nurse Pract 2010;22:450-9. [Crossref] [PubMed]
- Chien TJ, Liu CY, Fang CJ. The Effect of Acupuncture in Breast Cancer-Related Lymphoedema (BCRL): A Systematic Review and Meta-Analysis. Integr Cancer Ther 2019;18:1534735419866910. [Crossref] [PubMed]
- Jin H, Xiang Y, Feng Y, et al. Effectiveness and Safety of Acupuncture Moxibustion Therapy Used in Breast Cancer-Related Lymphedema: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med 2020;2020:3237451. [Crossref] [PubMed]
- Yu S, Zhu L, Xie P, et al. Effects of acupuncture on breast cancer-related lymphoedema: A systematic review and meta-analysis. Explore (NY) 2020;16:97-102. [Crossref] [PubMed]
- Chen J, Pei CQ, Wu XM, et al. Acupuncture therapy for 28 cases of postoperative upper limb edema after breast cancer. Zhejiang Journal of Traditional Chinese Medicine 2016;51:905.
- Liu XF, Zhang X, Kong J. Observational Study on the Efficacy of Needle Warming Moxibustion in Edema of the Upper Extremity and Anxiety-depression of Mammary Cancer Patients After Operation. World Chinese Medicine 2019;14:1856-60.
- Yang XH. Observation on the clinical efficacy of filiform fire needle therapy in the treatment of lymphedema after breast cancer surgery. Changsha: Hunan University of Traditional Chinese Medicine, 2021.
- Zeng HZ. Effect of buccal acupuncture on postoperative pain syndrome of breast cancer. Guangzhou: Guangzhou University of Chinese Medicine, 2021.
- Wang KH, Wu JR, Zhang D, et al. Comparative efficacy of Chinese herbal injections for treating chronic heart failure: a network meta-analysis. BMC Complement Altern Med 2018;18:41. [Crossref] [PubMed]
- The diagnosis and treatment of peripheral lymphedema. Consensus document of the International Society of Lymphology. Lymphology 2003;36:84-91.
- Breast Cancer Professional Committee of the China Anti-Cancer Association. Breast cancer diagnosis and treatment guidelines of China Anti-Cancer Association. China Oncology 2015;25:692-754.
- Chiarotto A, Maxwell LJ, Ostelo RW, et al. Measurement Properties of Visual Analogue Scale, Numeric Rating Scale, and Pain Severity Subscale of the Brief Pain Inventory in Patients With Low Back Pain: A Systematic Review. J Pain 2019;20:245-63. [Crossref] [PubMed]
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [Crossref] [PubMed]
- Han YJ. Efficacy and mechanism of warm acupuncture in improving upper extremity lymphedema after breast cancer surgery. Tianjin: Tianjin University of Traditional Chinese Medicine, 2020.
- Jiao HF. Efficacy evaluation of acupuncture and moxibustion in the treatment of upper limb lymphedema after breast cancer surgery. Nei Mongol Journal of Traditional Chinese Medicine 2017;36:130.
- Wang C, Yang M, Fan Y, et al. Moxibustion as a Therapy for Breast Cancer-Related Lymphedema in Female Adults: A Preliminary Randomized Controlled Trial. Integr Cancer Ther 2019;18:1534735419866919. [Crossref] [PubMed]
- Zhang JY. Clinical effect of warm acupuncture combined with acupoint application on upper limb edema after radical mastectomy. Liaoning Traditional Chinese Medicine Magazine, 2023. Available online: http://kns.cnki.net/kcms/detail/21.1128.r.20220928.1131.008.html
- Liu H, Fan YY, Shen J, et al. Clinical Observation of Drug Moxibustion and Simple Moxibustion in the Treatment of Breast Cancer Related Lymphedema. World Journal of Integrated Traditional and Western Medicine 2020;15:2274-7.
- Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342:d549. [Crossref] [PubMed]
- Wu W, Zhang XP. Observation on the curative effect of Huoxue Li Shi Jiedu Decoction combined with warm acupuncture in the treatment of upper limb edema after breast cancer surgery. Modern Journal of Integrated Traditional Chinese and Western Medicine 2016;25:3251-3.
- Zhao Y. Clinical study of electroacupuncture combined with ear acupuncture in the treatment of upper extremity lymphedema after breast cancer with qi deficiency and blood stasis. Kunming: Kunming Yunnan University of Traditional Chinese Medicine, 2019.
- Fang XL, Wang YZ, Li XH. The theory and clinical application of buccal acupuncture. Chinese Journal of Natural Medicine 2007;9:29-33.
- Pu RS. Experimental study on analgesic efficacy of buccal acupuncture and its effect on monoamine neurotransmitters. Lanzhou: Gansu University of Traditional Chinese Medicine, 2015.
- Shen W, Li LN, Zhang RX, et al. Clinical application of buccal acupuncture in the treatment of pain. Chinese Manipulation & Rehabilitation Medicine 2021;12:8-9, 12.
- Wang YZ, Wang HD, Fang XL, et al. Application of buccal acupuncture in the clinical treatment of pain. Chinese Journal of Acupuncture and Moxibustion 2000;20:43-4.
- Wang Y. Buccal acupuncture theory and its application in pain clinic. Lanzhou: Gansu Academy of Traditional Chinese Medicine, 2005.
- Ren CZ, Fang XL, Du XZ. Treatment of 56 cases of acute lumbar sprain with buccal acupuncture combined with exercise therapy. Chinese Journal of Acupuncture and Moxibustion 2014;34:245-6.
- Liu Q, Jia JJ. Buccal acupuncture combined with exercise therapy in the treatment of 41 cases of stiff neck. Journal of Traditional Chinese Medicine for External Treatment 2014;23:17.
- Dai HL. Clinical study of Cheek acupuncture in the treatment of cervical spondylosis. Guangzhou: Guangzhou University of Traditional Chinese Medicine, 2020.
(English Language Editor: L. Huleatt)




