
Novel application of a thyroid gland flap in repairing a mucosal defect to prevent pharyngocutaneous fistula following total laryngectomy: a case report
Introduction
Pharyngocutaneous fistula (PCF) formation is the most common uncomfortable complication of total laryngectomy (TL). According to prior meta-analyses, the incidence rate of PCF is between 21% and 58% (1,2). PCF significantly delays incision healing and affects the postoperative functional recovery and quality of life of patients (1). Moreover, PCF also prolongs the hospital stay and increases the cost of hospitalization, which further aggravates patient concerns (1). It is widely accepted that the introduction of vascularized tissue dramatically reduces PCF following TL (3). To date, multiple strategies have been used to prevent PCF, including flap application to repair the mucosal defect, in which the pectoralis major myocutaneous flap is most commonly used (4). However, considering the additional surgical trauma and complex flap tissue requirements, all flap application procedures could potentially create donor-site defects (3,4).
Herein, we report the case of an elderly male patient who received TL for laryngeal squamous cell carcinoma. The patient underwent thyroid gland flap (TGF) application from the same incision as the surgical area to reduce the tension of the mucosal suture after TL. This report aimed to provide a new repair strategy for neck defects and prevent PCF. We present the following article in accordance with the CARE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-319/rc).
Case presentation
Basic information
A 78-year-old male patient was admitted to the Baotou Cancer Hospital on December 14, 2017, due to “hoarseness for 3 months and difficulty breathing after activity for 1 week”. Upon admission, physical examination determined that the patient was 165-cm tall and only weighed 44 kg. It was noted that he lost 3 kg since his symptoms began. A medical history of major illnesses and hereditary diseases were denied. Preoperative ultrasound and functional examination of the thyroid, which were carried out in another hospital in October 2017, were normal and excluded tumor invasion, metastasis, and other thyroid diseases. The biopsy suggested laryngeal squamous cell carcinoma, but no interventions were initiated. The patient’s body mass index (BMI) was only 16.17 kg/m2 due to tumor consumption and insufficient nutrient intake, and presented cachexia symptom. He also has dyspnea and decreased respiratory function. Cardiac ejection fraction was 45%.
Clinical diagnosis
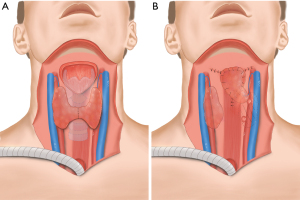
Following admission to our hospital, computed tomography (CT) was performed. The image of the tumor is presented in Figure 1. During the operation, an ulcerative mass of the right arytenoepiglottis fold, infiltrative growth of the bilateral vocal cords and ventricular zone mass, local destruction of the right thyroid cartilage plate, and tumor invasion were observed. The final diagnosis was confirmed to be laryngeal squamous cell carcinoma (T4N1M0 phase III).
Surgical procedures of TGF
The patient underwent TL, lymph node biopsy, TGF repair, and tracheostomy, under general anesthesia on December 27, 2017. After TL, a semi-Y-shaped suture was applied, and the pharyngeal mucosal defect was about 2.0 cm × 2.0 cm. Given the advanced age of the patient and relative weakness from the disease, it was decided that the thyroid gland from the same incision as a pedicled flap would be used to repair the mucosal defect and prevent PCF, as opposed to additional incisions for flap retrieval.
Briefly, the left superior thyroid artery and vein were reserved, and the inferior pole and middle vein of the left thyroid were cut and ligated. Next, the thyroid isthmus was severed on the right side and the thyroid gland tissue flap, pedicled with the left superior thyroid artery, was prepared, rotated upward, and inserted to repair the pharyngeal mucosal defect (Figure 2A,2B). No adverse events or complications occurred during the hospital days. Postoperatively, the patient recovered well and was discharged on January 12, 2018. Routine care for tracheostomy was carried out every day. The patient was satisfied with the relevant treatment and cooperated well.
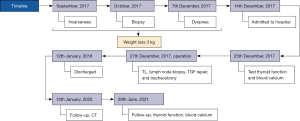
Subsequently, the patient was followed up every 6 months for more than 50 months (up to the present). Laboratory tests and image findings showed no tumor recurrence or distant metastasis. In the follow-up examinations on January 15, 2020, the thyroid flap remained healthy and in place (Figure 3). The internal surface of the pharyngeal cavity had sufficient and normal mucosa, and no postoperative complications such as PCF, dysphagia, hypothyroidism, and hypocalcemia were detected (Table 1). See Figure 4 for the treatment timeline in this article.
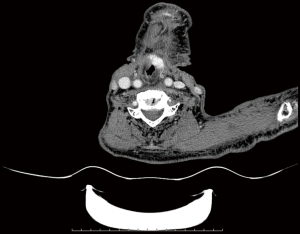
Table 1
| Items (reference range) | 2017-12-25 | 2021-6-29 |
|---|---|---|
| FT3 (3.10–6.80 pmol/L) | 4.16 | 4.21 |
| FT4 (12.00–22.00 pmol/L) | 13.16 | 12.68 |
| TSH (0.27–4.20 mIU/L) | 3.10 | 2.96 |
| Ca2+ (2.10–2.60 mmol/L) | 2.19 | 2.21 |
FT3, free triiodothyronine; FT4, free tetraiodothyronine; TSH, thyroid-stimulating hormone; Ca2+, blood calcium concentration.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
As the standard surgical intervention for laryngeal cancer, TL often results in PCF as a common complication (1-4). Generally, excessive suture tension of the residual mucosa and mucosal defect can lead to PCF development, and flap repair is the most popular strategy for PCF prevention (3,4). There are numerous alternative flaps available for neck repair, such as a pectoralis major flap (5), temporoparietal fascia flap (6), folded trapezius flaps (7), etc. If chosen correctly, mucosal repair can greatly alleviate the mucosal defect caused by tumor resection and can reduce the resulting mucosal suture tension. In addition, the tissue provided by the flap can effectively fill the dead space caused by surgery, which is conducive to surgical area healing (3,4).
A previous report showed that vascular pedicled flaps of the thyroid and submandibular glands were superior to other materials in the reconstruction of the larynx (8). The TGF strategy used in this case is characterized by multiple advantages. Firstly, the TGF was prepared using tissues in the same incision as the TL (with or without neck dissection), resulting in less trauma and a shorter operation time. In contrast, the use of the major pectoralis flap or other vascularized free flaps may lead to donor-site defects and longer recovery time (3,4). Secondly, since TGF is a pedicle flap, the superior thyroid vessels remain stable and reliable, and the preparation process can be completed easily, without the need for vascular anastomosis. Thirdly, TGF can also provide an almost appropriate size, without forming a bloated outer appearance. It also provides an adequate area and smooth luminal surface for the restoration of the pharynx surface, thus reducing stricture formation and dysphagia. Fourthly, compared to other types of flaps, TGFs are less likely to develop atrophy due to their rich blood supply and excellent durability (9). This was evident in our patient, who exhibited both normal thyroid function and normal serum calcium levels during the postoperative follow-up. Fifthly, given that TGF has a longer vascular pedicle, it can reach and repair defects in the head and neck region, as compared to other flap candidates such as the submandibular gland (10). To sum up, because the preparation of TGF is simple and fast, its blood supply is stable, and provides a volume of tough tissue that can be used to repair defects and fill dead space. In addition, the flap transposition has no significant impact on the thyroid and parathyroid functions. So, the application of TGF is safe and effective. In this case, TGF was used to repair the pharyngeal mucosal defect after TL. There was no relevant application report in the previous literature. This method may provide a new choice for the repair of cervical defects.
The experience of this case showed that TGF application is suitable for elderly and medically fragile patients with a healthy thyroid gland who is unable to undergo prolonged surgery. Further controlled studies should be designed to demonstrate the safety and efficacy of TGF in TL.
Conclusions
To the best of our knowledge, this is the first report of the application of TGF in repairing the mucosal defect and reducing the suture tension after TL. TGF was easily employed without any associated complications in our elderly patient who had severe weight loss and locally advanced laryngeal cancer. Therefore, TGF may be a new pedicled flap strategy for repairing defects in the neck, benefiting patients in selectively suitable cases.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-319/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-319/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang M, Xun Y, Wang K, et al. Risk factors of pharyngocutaneous fistula after total laryngectomy: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 2020;277:585-99. [Crossref] [PubMed]
- Liang JW, Li ZD, Li SC, et al. Pharyngocutaneous fistula after total laryngectomy: A systematic review and meta-analysis of risk factors. Auris Nasus Larynx 2015;42:353-9. [Crossref] [PubMed]
- Chen DW, Ellis MA, Horwich P, et al. Free Flap Inset Techniques in Salvage Laryngopharyngectomy Repair: Impact on Fistula Formation and Function. Laryngoscope 2021;131:E875-81. [Crossref] [PubMed]
- Han B, Han Z, Wu J, et al. Regional pedicled flaps in prevention and repair of pharyngocutaneous fistulas. Am J Otolaryngol 2021;42:103119. [Crossref] [PubMed]
- Gonzalez-Orús Álvarez-Morujo R, Martinez Pascual P, Tucciarone M, et al. Salvage total laryngectomy: is a flap necessary? Braz J Otorhinolaryngol 2020;86:228-36. [Crossref] [PubMed]
- Molteni G, Gazzini L, Sacchetto A, et al. Role of the temporoparietal fascia free flap in salvage total laryngectomy. Head Neck 2021;43:1692-4. [Crossref] [PubMed]
- Huang ZQ, Zhou B, Chen WL, et al. Use of a folded extended vertical lower trapezius island myocutaneous flap to repair large pharyngocutaneous fistulae developing after salvage total laryngectomy. Int J Oral Maxillofac Surg 2018;47:1268-73. [Crossref] [PubMed]
- Mozolewski E, Maj P, Kordowski J, et al. Vascular pedicle flap of the thyroid or submandibular gland in the reconstruction following partial laryngectomy. Otolaryngol Pol 1999;53:387-96. [PubMed]
- Ikeda A, Okamoto H, Tsuchiya Y, et al. Case of partial vertical laryngectomy with vocal cord reconstruction using a thyroid gland flap. Head Neck 2014;36:E73-7. [Crossref] [PubMed]
- Yang B, Su M, Li H, et al. Use of submandibular gland flap for repairing defects after tumor resection in the infratemporal region. J Craniomaxillofac Surg 2015;43:87-91. [Crossref] [PubMed]
(English Language Editor: A. Kassem)



