
The efficacy of continuing nursing interventions on intraoperative pressure ulcer-related complications in breast cancer patients: systematic review and meta-analysis
Introduction
In 2021, there were approximately 430,000 new cancer cases and 290,000 cancer deaths in China, accounting for 23.7% and 30.0% of the worldwide incidence and death rates, respectively (1). The high incidence and fatality rates make malignant tumors a serious threat to human health and life. In 2018, there were 2.094 million new breast cancer patients and 1.761 million deaths worldwide, accounting for 11.6% of the total cancer incidence and 18.4% of cancer mortality, ranking breast cancer first among malignant tumors (2). The symptoms of breast cancer patients are complex and changeable (3). In clinical work, pressure ulcers (PUs) are recognized as a common nursing complication (4). There are 2.5 million people suffering from PUs in the United States every year, along with 23.1% in the Netherlands, 7.3–13.9% in Germany, 26.5% and 9–12% in Victoria and Western Australia (5). The prevalence of PUs in China is 1.14% and 1.78% (6). PUs increase the pain of patients, and patients can experience a sense of isolation, fear, anxiety, and other bad emotions. The cost of hospitalization is increased, wasting social resources at the same time, which increases social and family economic burden and prolongs the hospitalization of patients. This in turn affects the diagnosis and treatment of the primary disease. PUs have become one of the most expensive complications of the 20th century due to their high cost of treatment.
Continuous nursing intervention is based on a certain scientific theory, under the guidance of nursing diagnosis, continuous according to the predetermined intervention methods engaged in a series of nursing activities. Nurses determine nursing interventions according to the characteristics of nursing diagnosis, nursing research results, the potential of patients’ functional rehabilitation, and the ability of patients and nurses themselves. Compared with the control group, the incidence of pressure ulcers complications in the experimental group was significantly less due to the continuous nursing intervention (P<0.05) (7). However, another single-center randomized controlled study (8) found that complications of pressure ulcers were inevitable in patients with breast cancer after surgery due to long-term bed rest and whether continuous nursing intervention was given.
Good nursing behavior of caregivers is very important to prevent PUs and improve the quality of life of bedridden patients. Studies (9,10) have shown that there is a positive correlation between the level of PUs and the nursing behavior of the primary caregivers. PUs increase the burden of patients and caregivers. How to reduce the incidence of PUs in patients with advanced breast cancer and improve their quality of life is worthy of discussion and study.
The effectiveness of continuous nursing intervention for intraoperative pressure ulcers related complications in breast cancer patients is highly controversial. Therefore, it is necessary to systematically review and address this issue by means of meta-analysis. Although continuous nursing intervention plays an important role in the management of intraoperative PUs in breast cancer patients, there are still many controversies. Therefore, we systematically reviewed the value of continuous nursing intervention in the prevention of intraoperative PUs in breast cancer patients by adopting the method of meta-analysis. We present the following article in accordance with the PRISMA reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-258/rc).
Methods
Literature inclusion criteria
The literature inclusion criteria were as follows: (I) patients met the clinical diagnosis criteria for stage III and IV advanced breast cancer in the Primary Breast Cancer Diagnosis and Treatment Guidelines 2021 edition; (II) PU Braden score ≤18 points; (III) Karnofsky Performance Status (KPS) score ≥70; (IV) voluntarily participated in the study with informed consent; (V) no skin damage occurred; (VI) patients who lived in this city (Chengdu, China); (VII) literature was included in strict compliance with the PICOS principle. Experimental group: continuous nursing intervention; control group: conventional nursing.
Literature exclusion criteria
The literature exclusion criteria were as follows: (I) patients with unavoidable PUs (according to the standard of unavoidable PUs, the expert group of wound stomostomy was judged by 2 people); (II) patients who had developed skin lesions, including rashes and skin ulceration caused by targeted drugs; (III) studies on multiple malignant tumors were excluded; (IV) patients with severe infection were excluded.
Search strategy
In this study, the Cochrane Library, PubMed, Web of Science, Embase, and Chinese Biomedical Literature Database (CBM) were searched, along with other databases and related websites. Subject words such as “continuing nursing interventions”, “breast cancer”, “pressure ulcer care”, and related drug trade names were retrieved as subject words and free words, respectively. In order to avoid bias caused by language limitations, this study searched both Chinese and English literature. In order to avoid missing relevant studies, relevant references listed in the article and conference abstracts found in the search were traced (Figure 1).
Data collection and extraction
Study data that met the criteria were extracted unblinded. Basic information including the first author, study area, year of literature publication, type of study design, sample content (case and control groups), control source, odds ratio (OR) values of breast cancer risk factors, and 95% confidence interval (CI) were collected.
Risk bias analysis
We used Cochrane risk of bias to analyze the risk of bias in the literature included in this study.
Braden scores
Braden scale is an important evaluation method to judge the risk of pressure ulcer. The lower the score, the higher the risk of pressure ulcer. The highest score is 23 points, 15–18 points are low risk, 13–14 points are medium risk, 10–12 points are high risk, and <9 points are high risk of pressure ulcer.
Statistical analysis
Statistical analysis was performed using Review Manager 5.1. Using the OR value of each study as the effect size for binary variable, and MD value for Continuity variable. Heterogeneity was assessed using the Q test and I2 (P<0.1 indicated heterogeneity), where I2 of 0% to 40% indicated that heterogeneity was unimportant, 30% to 60% indicated possible moderate heterogeneity, 50% to 90% indicated substantial heterogeneity, and 75% to 100% indicated considerable heterogeneity. Homogeneity and heterogeneity data were analyzed with fixed and random effects models. The sensitivity analysis combined the changes of the effect size between the fixed effects model and the random effects model to determine whether the analysis results were stable. P<0.05 indicated that the difference between the two groups was statistically significant.
Results
Literature screening results
A total of 1,431 relevant documents were retrieved. After eliminating articles according to the inclusion and exclusion criteria and removing duplicate literature, 9 documents were finally included (11-19) after reading the topic, abstract, and full text (Table 1). The bias assessment was done by Cochrane ROB (Figure 2).
Table 1
| Study | Age (years) | Tumor type | Braden score | Experimental group (N) | Control group (N) |
|---|---|---|---|---|---|
| Hu BH 2016 | 68.9±5.67 | Breast cancer | <11 | 130 | 130 |
| Guan XM 2015 | 72.2±18.1 | Breast cancer | 11.03±0.88 | 113 | 113 |
| Zeng J 2015 | 61–97 | Breast cancer | NR | 35 | 33 |
| Wu YF 2016 | 73.4±19.2 | Breast cancer | 10.53±0.94 | 76 | 80 |
| Wang XL 2017 | 73.51±18.9 | Breast cancer | 12.51±0.91 | 82 | 83 |
| Liu N 2019 | 65.32±6.3 | Breast cancer | <12 | 53 | 53 |
| Cao P 2017 | 60–87 | Breast cancer | <11 | 65 | 65 |
| Li Y 2017 | 67.2±4.5 | Breast cancer | NR | 100 | 100 |
| Chen QA 2017 | 73.7±8.6 | Breast cancer | <11 | 60 | 60 |
The data are represented as mean ± SD or range. NR, no report.
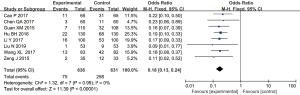
PU incidence
Eight of the 9 studies reported UP incidence, there was significant statistical difference in the incidence of PUs between the experimental group and the control group (OR =0.18, 95% CI: 0.13–0.24, P<0.00001) (Figure 3).
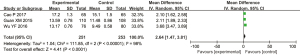
Braden pressure ulcer risk score
Only 3 studies assessing the Braden pressure ulcer risk score after nursing, there was significant statistical difference in Braden score between the experimental group and the control group (MD =2.64, 95% CI: 1.47–3.81, P<0.0001) (Figure 4).
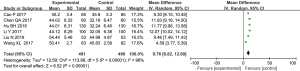
Quality of life
Six of the 12 studies reported the quality of life after nursing, there was significant statistical difference between the experimental group and the control group (MD =9.76, 95% CI: 6.82–12.69, P<0.00001) (Figure 5).
Publication bias
There was no significant bias for the study (Figure 6).
Discussion
Breast cancer has the highest mortality rate of all malignant tumors in women worldwide (20). Due to the complex and variable symptoms of breast cancer patients, this population has a high incidence of PUs. Various anti-tumor treatments affect patients’ nutrition metabolism, food intake, absorption barriers, the catabolism of tumor cells, and tumor biological activity, resulting in advanced cancer pain, hypoalbuminemia, severe malnutrition, and other issues. If corresponding measures are not taken in time, PUs can develop in a short time (21). At present, China’s community medical care is not perfect. The home care of patients with advanced breast cancer is mainly taken care of by patients’ relatives, and relatives’ understanding of PUs directly affects the quality of life of patients, and the occurrence of PUs is also closely related (22-24). Continuity of care is a continuation from hospital to home, including hospital discharge plans, referrals, and continued follow-up and guidance after patients return to their families or communities. The continuity of care model in foreign studies (25-28) is mainly through the integration of the telemedicine specific model, telemedicine platform including the use of web-based education programs, promoting self-management patient applications, and the peer-based patient-driven platform of pressure ulceration continuity care model. Researchers in various countries are increasingly using a multidisciplinary mode of treatment for PUs, rather than just relying on nursing for treatment and prevention. PU treatment guidelines include PU laser treatment, with the recommended grade being the lowest (29), but these guidelines also broaden our understanding of the treatment of PUs. Continuity of care from the perspective of patients involves experiencing the process of coordination and the continuation of health care services. Continuity will be accepted by the patients of health services in the event with the patient’s knowledge background, cognitive, accepting way, so that the patients with family members, medical workers together into intrinsic motivation, have the effect of health promotion (30-32).
This paper has some limitations in the research process: (I) the included studies were all retrospective controlled studies with a greater probability of selection bias, which may affect the conclusions of the meta-analysis; (II) most studies did not directly report HR and its 95% CI, and the data extracted from the survival curve may be biased from the real data, which may then bias the pooled results; (III) the operation level and operation mode of the operator were not completely consistent, which may also affect the reliability of the results.
Although the number of cases of PUs in the 2 groups of patients with continuous care was low (33). Most PUs can be prevented by effective measures, though not all PUs can be prevented. Patients with advanced tumors have poor physiological function, often with varying degrees of edema, bad fluid, and other symptoms. Coupled with long-term bed rest, this can easily induce PUs (34). The model of continuous care can minimize the incidence of PUs, which requires continuous exploration and practice to find the best intervention program to reduce PUs.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-258/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-258/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gucalp A, Traina TA, Eisner JR, et al. Male breast cancer: a disease distinct from female breast cancer. Breast Cancer Res Treat 2019;173:37-48. [Crossref] [PubMed]
- Xu X, Zhang M, Xu F, et al. Wnt signaling in breast cancer: biological mechanisms, challenges and opportunities. Mol Cancer 2020;19:165. [Crossref] [PubMed]
- Liang Y, Zhang H, Song X, et al. Metastatic heterogeneity of breast cancer: Molecular mechanism and potential therapeutic targets. Semin Cancer Biol 2020;60:14-27. [Crossref] [PubMed]
- Shen Y, Peng X, Shen C. Identification and validation of immune-related lncRNA prognostic signature for breast cancer. Genomics 2020;112:2640-6. [Crossref] [PubMed]
- Hahnel E, El Genedy M, Tomova-Simitchieva T, et al. The effectiveness of two silicone dressings for sacral and heel pressure ulcer prevention compared with no dressings in high-risk intensive care unit patients: a randomized controlled parallel-group trial. Br J Dermatol 2020;183:256-64. [Crossref] [PubMed]
- Du Y, Wu F, Lu S, et al. Efficacy of pressure ulcer prevention interventions in adult intensive care units: a protocol for a systematic review and network meta-analysis. BMJ Open 2019;9:e026727. [Crossref] [PubMed]
- Young C. Using the 'aSSKINg' model in pressure ulcer prevention and care planning. Nurs Stand 2021;36:61-6. [Crossref] [PubMed]
- Díaz-Valenzuela A, García-Fernández FP, Carmona Fernández P, et al. Effectiveness and safety of olive oil preparation for topical use in pressure ulcer prevention: Multicentre, controlled, randomised, and double-blinded clinical trial. Int Wound J 2019;16:1314-22. [Crossref] [PubMed]
- Kayser SA, VanGilder CA, Lachenbruch C. Predictors of superficial and severe hospital-acquired pressure injuries: A cross-sectional study using the International Pressure Ulcer Prevalence™ survey. Int J Nurs Stud 2019;89:46-52. [Crossref] [PubMed]
- Taylor C, Mulligan K, McGraw C. Barriers and enablers to the implementation of evidence-based practice in pressure ulcer prevention and management in an integrated community care setting: A qualitative study informed by the theoretical domains framework. Health Soc Care Community 2021;29:766-79. [Crossref] [PubMed]
- Hu BH, Li H, Wei XL, et al. Study on continuous nursing to reduce the incidence of pressure ulcer in elderly patients with high-risk pressure ulcer. Chinese Journal of Practical Nursing 2016;32:1285-8.
- Guan XM, Yu LY, Lu LM, et al. Application of quality control circle activities in continuous nursing of high-risk patients with pressure ulcer. Chinese Journal of Modern Nursing 2015;5.
- Zeng J, Yang Y. Study on the effect of continuous nursing on improving the home nursing behavior of caregivers of high-risk elderly patients with pressure ulcer. Journal of Nursing Education 2015;30:4.
- Wu YF, Chen F, Jin CH. Evaluation of application effect of continuous nursing in high-risk patients with pressure ulcer. General Nursing 2016;14:2.
- Wang XL, Wang YP, Zou WF, et al. evaluation of the application effect of continuous nursing based on wechat public platform in high-risk patients with pressure ulcer. Chinese Journal of Practical Nursing 2017;33:5.
- Liu N, Wang J. Application value of continuous nursing intervention in discharge follow-up of elderly patients with high-risk pressure ulcer. Laboratory Medicine and Clinic 2019;16:3.
- Cao P. Effect of continuous nursing intervention on reducing the incidence of pressure ulcer in elderly patients with high-risk pressure ulcer. Electronic Journal of Practical Clinical Nursing 2017;2:95-6.
- Li Y. Study on continuous nursing to reduce the incidence of pressure ulcer in elderly patients with high-risk pressure ulcer. China Continuing Medical Education 2017;9:2.
- Chen QA, Xie JY, Tan JP. Effect analysis of continuous nursing on prevention and treatment of pressure ulcer among high-risk groups in elderly centers. China Medical Innovation 2017;14:4.
- Mäkinen M, Haavisto E, Lindström V, et al. Finnish and Swedish prehospital emergency care providers' knowledge and attitudes towards pressure ulcer prevention. Int Emerg Nurs 2021;55:100873. [Crossref] [PubMed]
- Parisod H, Holopainen A, Kielo-Viljamaa E, et al. Attitudes of nursing staff towards pressure ulcer prevention in primary and specialised health care: A correlational cross-sectional study. Int Wound J 2022;19:399-410. [Crossref] [PubMed]
- Nadukkandiyil N, Syamala S, Saleh HA, et al. Implementation of pressure ulcer prevention and management in elderly patients: a retrospective study in tertiary care hospital in Qatar. Aging Male 2020;23:1066-72. [Crossref] [PubMed]
- Baernholdt M, Yan G, Hinton ID, et al. Effect of preventive care interventions on pressure ulcer rates in a national sample of rural and urban nursing units: Longitudinal associations over 4 years. Int J Nurs Stud 2020;105:103455. [Crossref] [PubMed]
- Wei M, Wu L, Chen Y, et al. Predictive Validity of the Braden Scale for Pressure Ulcer Risk in Critical Care: A Meta-Analysis. Nurs Crit Care 2020;25:165-70. [Crossref] [PubMed]
- Tilmazer T, Tuzer H. Pressure Ulcer Prevention Care Bundle: A Cross-sectional, Content Validation Study. Wound Manag Prev 2019;65:33-9. [Crossref] [PubMed]
- Thomas M, Kelly ED, Abraham J, et al. Invasive lobular breast cancer: A review of pathogenesis, diagnosis, management, and future directions of early stage disease. Semin Oncol 2019;46:121-32. [Crossref] [PubMed]
- Slepicka PF, Cyrill SL, Dos Santos CO. Pregnancy and Breast Cancer: Pathways to Understand Risk and Prevention. Trends Mol Med 2019;25:866-81. [Crossref] [PubMed]
- Januškevičienė I, Petrikaitė V. Heterogeneity of breast cancer: The importance of interaction between different tumor cell populations. Life Sci 2019;239:117009. [Crossref] [PubMed]
- Anrys C, Van Tiggelen H, Verhaeghe S, et al. Independent risk factors for pressure ulcer development in a high-risk nursing home population receiving evidence-based pressure ulcer prevention: Results from a study in 26 nursing homes in Belgium. Int Wound J 2019;16:325-33. [Crossref] [PubMed]
- Efteli E, Güneş Ü. Assessing the Validity and Reliability of a New Pressure Ulcer Risk Assessment Scale for Patients in Intensive Care Units. Wound Manag Prev 2020;66:24-33. [Crossref] [PubMed]
- Reddy TP, Rosato RR, Li X, et al. A comprehensive overview of metaplastic breast cancer: clinical features and molecular aberrations. Breast Cancer Res 2020;22:121. [Crossref] [PubMed]
- Wendt C, Margolin S. Identifying breast cancer susceptibility genes - a review of the genetic background in familial breast cancer. Acta Oncol 2019;58:135-46. [Crossref] [PubMed]
- Marrazzo E, Frusone F, Milana F, et al. Mucinous breast cancer: A narrative review of the literature and a retrospective tertiary single-centre analysis. Breast 2020;49:87-92. [Crossref] [PubMed]
- Audeh W, Blumencranz L, Kling H, et al. Prospective Validation of a Genomic Assay in Breast Cancer: The 70-gene MammaPrint Assay and the MINDACT Trial. Acta Med Acad 2019;48:18-34. [Crossref] [PubMed]
(English Language Editor: C. Betlazar-Maseh)





