
National perspective on hospital readmissions following adrenalectomy
Introduction
Adrenalectomy is an increasingly common procedure in general, urologic, and endocrine surgery. Due to advancements in diagnostic technology and minimally invasive surgical procedures, adrenalectomies have increased by 45% in the past 20 years (1-3). Currently, laparoscopic adrenalectomy is the standard operative approach, with reduced postoperative pain, shorter length of hospital stay, and minimal scarring (2). Despite the widespread practice of this minimally invasive technique and its low associated mortality rate, the complication rates of adrenalectomy procedures range upwards of 20%, and the mean hospital length of stay (LOS) is reported to range from 3 to 8 days (4,5). Reported intraoperative complications include vascular injury, pleural injury, and injury to gastrointestinal organs (6). Postoperative complications include wound infection, urinary tract infection, deep vein thrombosis, sepsis, myocardial infarction, stroke, and mortality (7). Severe complications can lead to hospital readmission, which is used as a metric of hospital quality of care (8).
Readmissions represent a significant burden to the health care system (9). High readmission rates correlate with decreased quality of care, decreased patient well-being, and increased hospital costs (10,11). Recent literature has focused on analyzing readmission data for specific surgical procedures, as readmission magnitude and risk factors for post-surgical procedures are not well defined (12). Post-adrenalectomy readmission rates range from 2–10% (9). Given the heterogeneity of disease etiology and increasing frequency of adrenalectomies, identifying clusters of patients at higher risk of complications and readmission would be valuable to guide preoperative planning and postoperative care.
To delineate potential assessment points within the adrenalectomy surgical care plan, we (I) examined independent risk factors of readmission following adrenalectomy in the United States; (II) identified the clinical, demographic, and hospital factors leading to readmission; and (III) estimated the cost burden of preventable readmission on the healthcare system using an extensive, national database. We present the following article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-18/rc).
Methods
Data source
A cross-sectional analysis was carried out using the Nationwide Readmissions Database (NRD) for the years 2010–2014. NRD is part of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality (AHRQ). It is used to assess the cost and quality of healthcare services and analyze the outcomes of treatments. The NRD collects data from approximately fourteen million discharges per year from 21 geographically dispersed states in the United States. Excluded in the NRD is data from federal hospitals and long-term care facilities such as skilled nursing facilities or rehabilitation centers. Patients are tracked by a patient linkage number that allows for discharge and readmission tracking separate from index hospital. The NRD data is publicly available; thus, the institutional review board approval was exempted, and the patient’s written consent was waived. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Inclusion and exclusion criteria
The study population included adult patients (≥18 years) who underwent adrenal surgery as the primary admission procedure of either adenoma (functional and non-functional) or malignant adrenal disease (primary and secondary). Patients who died during the index hospitalization, who had additional procedures during time of adrenalectomy, or with missing values used to calculate the days from discharge to readmission were excluded. The generated sample was then surveyed for readmission. Cases are defined as patients who had unscheduled readmission within 30 or 90 days postoperatively. Index events for 30- and 90-day readmission were selected from January to November and from January to September, respectively. Controls are defined as patients who were not readmitted.
Study parameters
The study objective is to (I) assess the risk of readmission following adrenalectomy in the United States; (II) identify the clinical, demographic, and administrative factors associated with readmission; and (III) determine the burden of readmission in terms of the cost of health services.
Patient factors of interest included age (18–44, 45–64, 65+ years old), gender, state of residence (in-state or out-of-state), type of adrenalectomy (unilateral/partial or bilateral), causes of primary admission (adenoma or malignant neoplasm), number of chronic diseases, and causes of readmission. Comorbidities were identified based on Charlson comorbidity index score. NRD files for ‘cost to charge ratio’ and hospital charges were used to calculate hospital costs for each patient. The extra burden of 30- and 90-day readmission on the healthcare system was evaluated in the context of postoperative complications (none vs. one or more), inpatient mortality during adrenalectomy and readmission, hospital LOS (short stay ≤75th percentile and extended stay >75th percentile), and cost of health service (low-cost ≤75th percentile and high cost >75th percentile).
The study also included the following hospital characteristics: median household income quartile for patient’s zip code, hospital procedure volume (low, medium, and high volume: based on ≤25th percentile and >75th percentile), primary insurance type (Medicare, Medicaid, private insurance, and other), hospital ownership (government non-federal, private not-for-profit, and private investor-owned), hospital teaching status (metropolitan teaching, metropolitan non-teaching, and non-metropolitan), hospital bed size (small, medium, and large), and discharge disposition (routine, transfer to short-term hospital, home health care, against medical advice). International Classification of Disease, 9th Revision (ICD-9) was used to define the study variables (Table S1). Clinical Classification Software (CCS) was used to categorize diagnoses and procedures.
Statistical analysis
Data analysis used weighted measurements reflecting the national estimate level. Based on the HCUP user agreement, some variables with a low number of observations were not reported to avoid patient tracking. Unbiased and a priori cut-off values of quantitative variables were set at the median levels. Chi-square, Fisher’s Exact, Student’s t-test, and Mann-Whitney U tests were employed for univariate analysis of each independent factor. Significant variables were considered confounders and were further included in multivariate regression models. Odds ratio (OR) and 95% confidence interval (CI) were estimated. A significance level was set at P<0.05. Kaplan-Meier method and log-rank test were performed to generate curves of the probability of being readmission-free within 90 days following the initial procedure. Mean adjusted hospitalization cost and LOS were calculated by linear and binary logistic regression, respectively, to control for other covariates. Statistical data analyses were carried out using SAS 9.4 for Windows (SAS Institute Inc., Cary, NC, USA) and SPSS version 24.0.
Results
Demographic and clinical characteristics of adrenalectomy patients
A total of 20,494 adrenalectomy admissions (patients ≥18 years old) were reported between 2010 and 2014. Workflow for study selection is shown in Figure 1. Patients’ mean age was 57.4±13.8 years, and 10,267 (50.1%) of them were female. Patients presented with adenomas accounted for 17,502 (85.4%), while malignancy was diagnosed in 2,992 (14.6%) of cohorts. Most cases underwent unilateral and partial adrenalectomy, 17,748 (86.6%) and 2,377 (11.6%) respectively, whereas 369 (1.8%) of patients had bilateral adrenalectomy procedures (Table 1).
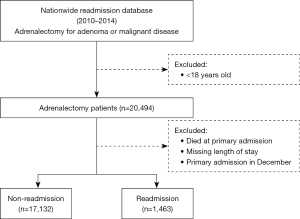
Table 1
| Characteristics | % |
|---|---|
| Age | |
| 18–44 years | 18.1 |
| 45–64 years | 48.4 |
| >65 years | 33.8 |
| Gender | |
| Male | 49.9 |
| Female | 50.1 |
| Residence of same state | |
| Non-resident | 10.3 |
| Resident | 89.7 |
| Household income quartile (percentile) | |
| 0–25th | 25.9 |
| 26–50th | 24.7 |
| 51–75th | 24.6 |
| 76–100th | 24.8 |
| Charlson comorbidity index score | |
| 0 | 61.1 |
| 1 | 27.7 |
| 2+ | 11.2 |
| No. of chronic conditions | |
| ≤6 | 81.8 |
| >6 | 18.2 |
| Cause of surgery | |
| Non-functional adenoma | 58.8 |
| Functional adenoma | 26.6 |
| Primary malignancy | 3.1 |
| Secondary malignancy | 11.5 |
| Type of procedure | |
| Unilateral/partial adrenalectomy | 98.2 |
| Bilateral adrenalectomy | 1.8 |
| Laparoscopic | |
| No | 97.8 |
| Yes | 2.2 |
| Postoperative complications | |
| None | 84.6 |
| One or more | 15.4 |
| In-hospital mortality | |
| Not reported | 99.8 |
| Reported | 0.2 |
| LOS, days | |
| Short stay (≤4) | 61.7 |
| Prolonged stay (>4) | 38.3 |
| Hospital charge, $ | |
| Low charge | 75 |
| High charge | 25 |
| Hospital cost, $ | |
| Low cost | 75 |
| High cost | 25 |
| Insurance status | |
| Private | 35.8 |
| Medicare | 8.2 |
| Medicaid | 49.4 |
| Others | 6.6 |
| Hospital bed size | |
| Small | 8.8 |
| Medium | 18.2 |
| Large | 73.0 |
| Hospital teaching status | |
| Metropolitan teaching | 23.2 |
| Metropolitan non-teaching | 73.2 |
| Non-metropolitan | 3.6 |
| Hospital volume | |
| Low | 32.6 |
| Medium | 45.1 |
| High | 22.3 |
| Hospital ownership | |
| Government non-federal | 13.8 |
| Private not-for-profit | 78.8 |
| Private investor owned | 7.4 |
| Urban-rural designation | |
| Large metropolitan areas | 61.6 |
| Small metropolitan | 34.8 |
| Micropolitan areas | 3.3 |
| Non-core | 0.3 |
| Discharge disposition | |
| Routine | 88.8 |
| Transfers | 5.6 |
| Home health care | 5.6 |
Data is presented as percentage. All adult patients underwent adrenalectomy during the period between 2010 and 2014 are included in the table. All numbers are presented as weighted national estimates. Cut-off values of hospital charge and cost are 54,165.07 and 15,454.06, respectively. LOS, length of stay.
Risk of complications and in-hospital mortality
Out of a total of 20,494 patients, postoperative complications were reported in 3,156 (15.4%) patients, accounting for one in six to be at risk. Bleeding and renal complications were the most frequent, accounting for 1,558 (7.6%) and 1,066 (5.2%) of complications, respectively (Figure S1). Patients with secondary malignancy were more likely to develop postoperative complications (17% vs. 12.4%, OR =1.44, 95% CI: 1.05–1.99) than primary malignancy, particularly technical complications (4.6% vs. 1%, OR =5.04, 95% CI: 1.83–13.8). In addition, patients with functional adenomas had a higher risk of renal complications (3.3% vs. 2.5%, OR =1.31, 95% CI: 1.5–1.65), bleeding (5.1% vs. 3.9%, OR =1.33, 95% CI: 1.1–1.6), and technical complications (2.4% vs. 1.1%, OR =2.21, 95% CI: 1.64–2.97). At primary admission, 41 (0.2%) patients died during their hospital stay. These patients all underwent bilateral procedures, and 37 (89.2%) experienced postoperative bleeding and cardiovascular system (CVS) complications (data not shown).
Frequency and risk factors for readmission
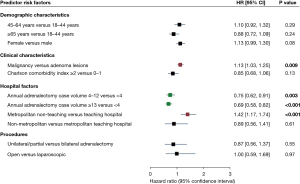
A total of 1,463 (7.9%) and 1,959 (12.7%) who were sent home from the hospital were readmitted within a month and three months, respectively (Figure 2). Half of the readmissions occurred within the first 19 days of discharge. The most common reasons for readmission were acute renal failure, postoperative infection, septicemia, glucocorticoid deficiencies, and pneumonia. Characteristics of 30- and 90-day readmitted patients are shown in Table 2. Patients with malignancy had a 13% increased risk of 30-day readmission compared to adenoma patients (HR =1.13; 95% CI: 1.03–1.25; P=0.009). Regarding hospital factors, those cohorts that underwent adrenalectomy procedures in metropolitan non-teaching hospitals were associated with 42% more risk of readmission versus metropolitan teaching hospitals (HR =1.42; 95% CI: 1.17–1.74; P<0.001). On the other hand, having an adrenalectomy procedure in a high-volume capacity of more than four operations per year showed a decreased risk of readmission to 25%, reaching as low as a 31% risk decrease in hospitals performing over 13 adrenalectomy procedures in a year (HR =0.75; 95% CI: 0.62–0.91; P=0.003) (Figure 3).
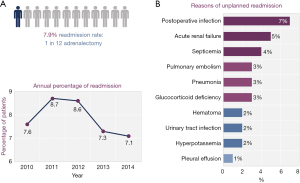
Table 2
| Characteristics at primary admission | 30-day readmission status | 90-day readmission status | |||||
|---|---|---|---|---|---|---|---|
| Non-readmission | Readmission | P value | Non-readmission | Readmission | P value | ||
| Demographic characteristics | |||||||
| Age (mean ± SD), years | 57.3±13.9 | 59.2±14.3 | <0.001 | 57±13.8 | 60±13.7 | <0.001 | |
| Gender | 0.87 | 0.014 | |||||
| Male | 8,522 (49.7) | 731 (50.0) | 6,710 (49.9) | 1,037 (52.9) | |||
| Female | 8,610 (50.3) | 731 (50.0) | 6,732 (50.1) | 923 (47.1) | |||
| Household income quartile | <0.001 | <0.001 | |||||
| Quartile 1 | 4,394 (26.1) | 403 (28.0) | 3,459 (26.2) | 460 (23.8) | |||
| Quartile 2 | 4,147 (24.6) | 400 (27.8) | 3,259 (24.7) | 605 (31.3) | |||
| Quartile 3 | 4,196 (24.9) | 294 (20.4) | 3,251 (24.6) | 437 (22.6) | |||
| Quartile 4 | 4,091 (24.3) | 343 (23.8) | 3,246 (24.6) | 429 (22.2) | |||
| Clinical characteristics | |||||||
| Primary diagnosis | <0.001 | <0.001 | |||||
| Non-functional adenoma | 5,119 (44.3) | 328 (34.8) | 4,090 (45.0) | 457 (35.8) | |||
| Functional adenoma | 4,826 (41.8) | 421 (44.6) | 3,864 (42.5) | 502 (39.3) | |||
| Primary malignancy | 320 (2.8) | 55 (5.8) | 243 (2.7) | 57 (4.5) | |||
| Secondary malignancy | 1,295 (11.2) | 140 (14.8) | 893 (9.8) | 262 (20.5) | |||
| Adrenalectomy type | 0.76 | 0.84 | |||||
| Unilateral/partial | 16,836 (98.3) | 1,435 (98.2) | 13,216 (98.3) | 1,928 (98.4) | |||
| Bilateral | 296 (1.7) | 27 (1.9) | 227 (1.7) | 31 (1.6) | |||
| Charlson comorbidity index score | 0.005 | 0.002 | |||||
| 0–1 | 10,448 (61.0) | 871 (59.5) | 8,261 (61.5) | 1,144 (58.4) | |||
| 2–3 | 4,622 (27.0) | 445 (30.4) | 3,557 (26.5) | 592 (30.2) | |||
| 4+ | 2,061 (12.0) | 147 (10.1) | 1,625 (12.1) | 224 (11.4) | |||
| Outcomes | |||||||
| Complications | <0.001 | <0.001 | |||||
| One or more | 982 (5.7) | 163 (11.1) | 747 (5.6) | 200 (10.2) | |||
| LOS (mean ± SD) | 3.8±3.5 | 5.8±6.8 | <0.001 | 3.8±3.5 | 5.6±6.6 | <0.001 | |
| Total cost, $ (mean ± SD) | 8,894±8,925.2 | 18,470.1±18,996.2 | <0.001 | 8,692.1±8,484.5 | 18,506.8±20,419.2 | <0.001 | |
| Hospital factors | |||||||
| Service payer | <0.001 | <0.001 | |||||
| Private | 6,080 (35.6) | 611 (42.0) | 4,650 (34.6) | 855 (43.7) | |||
| Medicare | 1,382 (8.1) | 174 (12.0) | 1,073 (8.0) | 233 (11.9) | |||
| Medicaid | 8,503 (49.7) | 571 (39.2) | 6,838 (50.9) | 746 (38.1) | |||
| Others | 1,149 (6.6) | 100 (6.8) | 871 (6.4) | 123 (6.3) | |||
| Hospital teaching status | 0.001 | 0.003 | |||||
| MT | 3,920 (22.9) | 302 (20.6) | 3,104 (23.1) | 391 (20.0) | |||
| MNT | 12,567 (73.4) | 1,128 (77.1) | 9,827 (73.1) | 1,503 (76.7) | |||
| NM | 645 (3.8) | 33 (2.3) | 512 (3.8) | 66 (3.4) | |||
| Discharge disposition | <0.001 | <0.001 | |||||
| Routine | 15,882 (92.7) | 1,196 (81.8) | 12,494 (93.0) | 1,658 (84.7) | |||
| SNICOF | 370 (2.2) | 96 (6.6) | 272 (2.0) | 105 (5.4) | |||
| Home care | 860 (5.0) | 169 (11.6) | 663 (4.9) | 194 (9.9) | |||
| Annual adrenalectomy volume | 0.021 | 0.036 | |||||
| Low | 5,608 (32.7) | 509 (34.8) | 4,390 (32.7) | 678 (34.6) | |||
| Medium | 7,329 (42.8) | 571 (39.0) | 5,759 (42.8) | 779 (39.8) | |||
| High | 4,195 (24.5) | 383 (26.2) | 3,294 (24.5) | 502 (25.6) | |||
Data is presented as number (percentage) or mean ± SD or median (quartiles). All numbers are presented as weighted national estimates. Two-tailed Chi-square and Fisher’s Exact were used for categorical variables while Student’s t-test was employed for quantitative data. Statistical significance was considered at P value <0.05. Annual hospital adrenalectomy volume (≤3, 4–13, >13). Categorization of quantitative variables were based on their medians. SD, standard deviation; LOS, length of stay; MT, metropolitan teaching; MNT, metropolitan non-teaching; NM, non-metropolitan; SNICOF, skilled nursing intermediate care other facility.
Burden of readmission on healthcare system
Readmission cases, on average, had 2.06 days of additional hospital stay, which is 0.54% more than the non-readmission controls. If this value is extrapolated to the national level, readmission resulted in 343.19 days of additional hospital stays. Aligned with LOS, the average additional cost attributed to readmission accounted for $18,529.4. Thus, from a national perspective, these cases were associated with additional hospital costs of $3,087,013.03.
Discussion
The Hospital Readmission Reduction program uses readmission rates as a quality metric, tracking hospital readmission rates through the Nationwide Readmissions database (8). Due to payment incentives and penalties, hospital leaders and clinical researchers are motivated to investigate specific variables that may be attributed to readmission rates (13). By identifying patient risk factors that lead to complications and subsequent readmission, surgeons can alter their surgical care plan, operative approach, or preoperative preparation to account for a higher-risk procedure (9).
In our study, 7.9% and 12.7% of adrenalectomy patients were readmitted at 30 and 90 days after discharge, respectively. Our observed readmission rate is nearly consistent with recent literature, reporting readmission rates between 2–10% (9). Postoperative complications were reported in 15.4% of patients, accounting for one in six at risk. Bleeding (7.6%) and renal complications (5.2%) were the most frequent. A previous national study on adrenalectomies reported a similar complication rate at 16% (5). Previous studies have focused on operational approach, surgeon specialty training, and intraoperative complications as variables for readmission rates following adrenalectomy (5,9). For our study, we examined the variables of patient demographics, type of adrenalectomy (unilateral/partial or bilateral), causes of primary admission (adenoma or malignant neoplasm), number of chronic diseases, causes of readmission, hospital demographics, and case volume in relation to post-adrenalectomy readmission rates.
Our study demonstrated that surgical complications and subsequent prolonged initial hospital stay were associated with a higher risk of readmission for patients following adrenalectomies. Patients with primary and secondary malignancy had the highest incidence of complications; therefore, patients with primary and secondary malignancy were most likely to be readmitted than patients with an adenoma lesion.
According to our findings, overall complication rates are higher in patients with primary and secondary malignancy, specifically technical and bleeding complications, after an adrenalectomy procedure. Malignancies are associated with increased vascularity, inflammation, immunosuppression, and a limited wound healing process, representing a complex pathology that may interfere with surgical recovery (14,15). Overall, the literature reports higher complication rates in patients with malignancies in many surgical specialties (14-17). To decrease the risk of complications, surgeons should consider a minimally invasive technique to reduce the risk of infection and complication when designing a surgical care plan (18,19). According to Beck et al. (9), open technique is associated with a higher readmission rate, as these patients were also associated with a higher complication rate and need to additional interventions, such as blood transfusion. Complications associated with open procedure included hemorrhage and adrenal injury (9). Surgeons may consider preventative measures such as preoperative administration of antibiotics and monitoring for renal insufficiency, hypercoagulability, and hemodynamic instability in patients with a co-existing metastasis and malignancy (9,20). We encourage researchers to investigate specific types of malignancies as well as the location, and their associated complications, as pathology and proximity may lead to an explanation of the occurrence of the complication and lead to appropriate preoperative prophylactic measures.
High hospital adrenalectomy volume was associated with a lower risk of readmission. Previous literature shows that high-volume surgeons performing adrenalectomy procedures are associated with lower complication rates, shorter LOS, and lower readmission rates (2,5,9). However, only 16% of adrenalectomy-performing surgeons are defined as high-volume, which may influence our reported nationwide complication rate (2). Gray et al. (21) reported that only one-third of surgeons had performed at least six adrenalectomies per year. Another study showed that surgeons performing at least six procedures were associated with lower complication rate and decreased hospital costs (22). Metropolitan teaching hospitals were also associated with a lower risk of readmission than metropolitan non-teaching hospitals. Excluding the ‘July Effect’ during which new interns enter residency after their medical school graduation, major teaching hospitals are associated with annual overall lower mortality rates, increased quality of care, and lower complication rates (23-25). These trends may result from increased oversight due to the presence of trainees and increased patient safety and quality of care initiatives due to government subsidies for graduate medical education. Referring physicians should consider directing their patients to high-volume metropolitan teaching hospitals for adrenalectomy procedures. Further characterization of hospital operational factors and their interaction with complication rate and LOS can identify measures to reduce readmissions rates nationally.
Regarding the cost burden on the healthcare system, we found that readmission following adrenalectomy added an extra 2.06 days to a hospital visit for the average patient, with additional hospital costs of $3,087,013.03. This additional LOS is consistent with the literature, which reports 2–9 days (4). To reduce costs, efforts may be made to ensure the above factors are considered: anticipate and prepare for common complications, define patients with primary malignancy and secondary malignancy as high-risk groups, and perform adrenalectomy cases at high volume, metropolitan teaching hospitals.
This study was conducted specifically for patients undergoing adrenalectomy. A considerable limitation is placed on extrapolating and generalizing the outcomes, given that we studied only one procedure (adrenalectomies), and common surgical complications and their respective risk factors specific to this procedure do not apply to other surgical procedures. Another considerable limitation is erroneous encoding in the database. We are unable to account for an unreported procedure that may have taken place during the adrenalectomy procedure. Limited information is available in database regarding operative approach; therefore, we were unable to include this variable in our analysis. Since this study reflects data from 2010–2014, results may be affected by time and changes that have occurred in the last 6 years. Unfortunately, due to the nature of the Nationwide Readmissions Database, the 2010–2019 data years cannot be combined to create a multi-data year database. Patient and hospital linkage numbers to not track the same patients and hospitals, respectively, across the years.
Conclusions
Hospital readmission rates following adrenalectomy are related to complication rates and initial hospital LOS. Specific adrenal pathologies are at higher risk for complications; therefore, they are at higher risk for readmission. To decrease complication rates and subsequent readmission rates, surgeons should recognize patient comorbidities, categorize risks associated with each adrenal pathology, and anticipate procedure complications specific to adrenalectomies. Referring physicians may also consider directing referrals to high-volume hospitals and metropolitan teaching hospitals. In effect, readmission rates may be decreased, leading to an increase in quality of care, an increase in patient well-being and satisfaction, and a decrease in unnecessary healthcare spending.
Further studies on the variables that correlate with readmission may provide insight into how hospital leadership and clinicians can deliver safe, quality, and efficient healthcare for hospitalized patients undergoing an adrenalectomy procedure.
Acknowledgments
A sincere thank you to Loula Burton from Tulane’s Research Proposal Development Office for her diligent editing and proofreading of this paper.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-18/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-22-18/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-18/coif). EK serves as an Editor-in-Chief of Gland Surgery from May 2017 to April 2024. The other authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Saunders BD, Wainess RM, Dimick JB, et al. Trends in utilization of adrenalectomy in the United States: have indications changed? World J Surg 2004;28:1169-75. [Crossref] [PubMed]
- Kazaure HS, Sosa JA. Volume-outcome relationship in adrenal surgery: A review of existing literature. Best Pract Res Clin Endocrinol Metab 2019;33:101296. [Crossref] [PubMed]
- Fuletra JG, Schilling AL, Canter D, et al. Adrenalectomy: should urologists not be doing more? Int Urol Nephrol 2020;52:197-204. [Crossref] [PubMed]
- Lindeman B, Hashimoto DA, Bababekov YJ, et al. Fifteen years of adrenalectomies: impact of specialty training and operative volume. Surgery 2018;163:150-6. [Crossref] [PubMed]
- Park HS, Roman SA, Sosa JA. Outcomes from 3144 adrenalectomies in the United States: which matters more, surgeon volume or specialty? Arch Surg 2009;144:1060-7. [Crossref] [PubMed]
- Strebel RT, Müntener M, Sulser T. Intraoperative complications of laparoscopic adrenalectomy. World J Urol 2008;26:555-60. [Crossref] [PubMed]
- Shariq OA, Bews KA, McKenna NP, et al. Is same-day discharge associated with increased 30-day postoperative complications and readmissions in patients undergoing laparoscopic adrenalectomy? Surgery 2021;169:289-97. [Crossref] [PubMed]
- Mehtsun WT, Papanicolas I, Zheng J, et al. National Trends in Readmission Following Inpatient Surgery in the Hospital Readmissions Reduction Program Era. Ann Surg 2018;267:599-605. [Crossref] [PubMed]
- Beck AC, Goffredo P, Hassan I, et al. Risk factors for 30-day readmission after adrenalectomy. Surgery 2018;164:766-73. [Crossref] [PubMed]
- Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg 2012;215:322-30. [Crossref] [PubMed]
- Tsai TC, Joynt KE, Orav EJ, et al. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med 2013;369:1134-42. [Crossref] [PubMed]
- Bilimoria KY, Liu Y, Paruch JL, et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 2013;217:833-42.e1-3.
- Jweinat JJ. Hospital readmissions under the spotlight. J Healthc Manag 2010;55:252-64. [Crossref] [PubMed]
- Caulley L, Johnson-Obaseki S, Luo L, et al. Risk factors for postoperative complications in total thyroidectomy: A retrospective, risk-adjusted analysis from the National Surgical Quality Improvement Program. Medicine (Baltimore) 2017;96:e5752. [Crossref] [PubMed]
- Lorusso R, Vizzardi E, Johnson DM, et al. Cardiac surgery in adult patients with remitted or active malignancies: a review of preoperative screening, surgical management and short- and long-term postoperative results. Eur J Cardiothorac Surg 2018;54:10-8. [Crossref] [PubMed]
- Bagrodia N, Button AM, Spanheimer PM, et al. Morbidity and mortality following elective splenectomy for benign and malignant hematologic conditions: analysis of the American College of Surgeons National Surgical Quality Improvement Program data. JAMA Surg 2014;149:1022-9. [Crossref] [PubMed]
- Tevis SE, Steiman JG, Neuman HB, et al. Postoperative complications in combined gynecologic, plastic, and breast surgery: An analysis from National Surgical Quality Improvement Program. Breast J 2019;25:1111-6. [Crossref] [PubMed]
- Uludağ M, Aygün N, İşgör A. Surgical Indications and Techniques for Adrenalectomy. Sisli Etfal Hastan Tip Bul 2020;54:8-22. [PubMed]
- Gonzalez R, Smith CD, McClusky DA 3rd, et al. Laparoscopic approach reduces likelihood of perioperative complications in patients undergoing adrenalectomy. Am Surg 2004;70:668-74. [PubMed]
- Park JT. Postoperative acute kidney injury. Korean J Anesthesiol 2017;70:258-66. [Crossref] [PubMed]
- Gray WK, Day J, Briggs TWR, et al. Volume-outcome relationship for adrenalectomy: analysis of an administrative dataset for the Getting It Right First Time Programme. Br J Surg 2021;108:1112-9. [Crossref] [PubMed]
- Anderson KL Jr, Thomas SM, Adam MA, et al. Each procedure matters: threshold for surgeon volume to minimize complications and decrease cost associated with adrenalectomy. Surgery 2018;163:157-64. [Crossref] [PubMed]
- Taylor DH Jr, Whellan DJ, Sloan FA. Effects of admission to a teaching hospital on the cost and quality of care for Medicare beneficiaries. N Engl J Med 1999;340:293-9. [Crossref] [PubMed]
- Ayanian JZ, Weissman JS. Teaching hospitals and quality of care: a review of the literature. Milbank Q 2002;80:569-93. v. [Crossref] [PubMed]
- Anderson KL, Koval KJ, Spratt KF. Hip fracture outcome: is there a "July effect"? Am J Orthop (Belle Mead NJ) 2009;38:606-11. [PubMed]


