
Multidisciplinary treatment of pancreatic cancer: a case report
Introduction
Surgical resection is the only way to radically treat pancreatic cancer, but the proportion of patients diagnosed as being resectable at the first diagnosis is very low (only 10–20% of all patients diagnosed with pancreatic cancer) (1). Postoperative recurrence of pancreatic cancer can result in pain, poor nutritional status, lower quality of life, and a reduction in mental health in patients. Building a reasonable treatment plan for a patient with postoperative pancreatic cancer requires a multidisciplinary and integrated team to alleviate the patient’s physical and psychological burden, improve their quality of life, and prolong their life. At present, the multidisciplinary diagnosis and treatment teams for patients with pancreatic cancer in China are evolving. Therefore, it is necessary to continue to accumulate multidisciplinary treatment (MDT) treatment experience and provide personalized diagnosis and treatment for more patients.
We present the following case in accordance with the CARE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-86/rc).
Case presentation
Initial diagnosis
The female patient was 53 years old. The patient developed yellow skin, yellow urine, and poor basic physical condition, and experienced weight loss for 1 month before January 2016. Pancreaticoduodenectomy was performed in Shanxi Provincial People’s Hospital in July 2016.The preoperative diagnosis was pancreatic cancer. Postoperative pathological examination indicated pancreatic adenocarcinoma. She was readmitted to the General Surgery of Shanxi Provincial People’s Hospital in August 2016 for the discovery of yellow sclera. The patient had undergone genetic testing in Shanxi Provincial People’s Hospital, August 2016. Results showed that tumor mutational burden (TMB) was below the Tris and programmed death-ligand 1 (PD-L1) was negative. The patient’s history revealed that she a laparoscopic hysteromyomectomy 4 years ago. The admission in August 2016 found that the patient had normal skin and mucosa without yellow staining. A surgical scar was found on the abdomen. There’s a T-tube in the abdomen. She had a soft abdomen without obvious tenderness or rebound pain. None of palpable abdominal mass, palpable under the liver margin, percussion pain in the liver and spleen, and percussion pain in the kidney area were found. Abdominal movement dullness was negative, and no tenderness was found in the bladder area. Bowel sounds were 5–6 times/minute. Laboratory tests showed that the tumor marker CA19-9 level was >500 µ/mL. Imaging findings by CT and MRI showed that the uncinate process of the pancreas had a lesion with a low density of 3.5 cm.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
MDT discussion and diagnosis and treatment
The first MDT discussion and treatment
MDT discussion
The comments of each team member are reproduced below.
Dr. Heng Lin, deputy chief physician (Hepatobiliary Surgery Pancreatic Group): pancreatic cancer is a common malignant tumor with an extremely high degree of malignancy. In recent years, with the development of imaging, pathology, endoscopy, and immunotherapy etc., the surgical resection success rate of pancreatic cancer has been greatly improved. The perioperative mortality and the incidence of severe complications have been remarkably reduced, but the prognosis of patients has not been improved. The patient was admitted to the Shanxi Provincial People’s Hospital for the discovery of yellow sclera. CT and MRI findings showed that the uncinate process of pancreas had an area with a low density of 3.5 cm. The patient underwent pancreaticoduodenectomy surgery, and the postoperative pathology suggested that she had pancreatic cancer. The malignant degree of carcinoma on the head of the pancreas is high; even if the tumor is removed by an operation, recurrence or metastasis occurs within 1 to 2 years after the operation, and the median survival time (MST) is only 22 to 25 months. Therefore, we should actively carry out multi-disciplinary comprehensive treatment.
Dr. Huaizhi Wang, chief physician (Hepatobiliary Surgery Pancreatic Group): according to the CONKO-0011, Espac-32 Studies, it is recommended that all patients after pancreatic cancer resection receive 6 months of adjuvant chemotherapy. Although the overall results did not prove that the combination regimen was superior to single-agent chemotherapy, stratified analysis found that the patients treated with a combination regimen had better physical performance scores than those treated with single-agent chemotherapy. This female patient had undergone radical resection Radical resection was performed 1 month before follow up, and there was no contraindication of chemotherapy in all the reexamination indexes. Therefore, the patient was recommended to be treated with the combination chemotherapy of Gemcitabine and Capecitabine to observe the patient’s tolerance to chemotherapy, and her tolerance to chemotherapy was evaluated periodically during chemotherapy.
Dr. Xifen Gong, deputy chief physician (Nutrition Department): patients with this type of pancreatic cancer should undergo routine nutritional screening and assessment and should be given active nutritional support if there is a risk of malnutrition in order to prevent the occurrence of cachexia caused by cancer. Patients should be given 25–30 kcal/kg of their body weight in food and 1.2–2.0 g/kg of their body weight in protein, and then the nutrition supply should be adjusted according to the nutritional and metabolic conditions of the patients. Meanwhile, the patients should be given nutrition education such as diet habits, diet composition, and diet collocation. If the patient appears to have anorexia or dyspepsia in the course of chemotherapy, she should receive relevant medicaments, such as pancreatin tablets, to improve appetite and promote digestion.
Dr. Hongyu Zhang, chief physician (Hepatobiliary Surgery Pancreatic Group): different tumors can effectively escape the recognition and death by immune cells due to immune tolerance, resulting in the occurrence and development of tumors. Tumor immunotherapy can control and eliminate tumors by restarting and maintaining the tumor-immune cycle and restoring the normal anti-tumor immune response. There are currently two main types of antibodies that kill tumor cells, one that binds to PD-1 on the surface of T cells, and another that binds to PD-L1 on the surface of tumor cells. The patient had undergone genetic testing in Shanxi Provincial People’s Hospital, August 2016. Results showed that TMB was below the Tris and PD-L1 was negative, therefore immunotherapy was not appropriate. The results of a comparative study between Erlotinib in combination with Gemtesa (GEM) and single-drug GEM showed that, although there was a statistically significant survival benefit, the benefit time was very limited. The standard treatment for unresectable pancreatic cancer is chemotherapy. The efficacy of gemcitabine was reported in 1997 (2). Therefore, first-line combination chemotherapy was given. The patient was given Eastern Cooperative Oncology Group (ECOG) scores during the procedure. Routine blood examination, biochemistry, CA19-9, CT of the chest, and enhanced CT of the upper abdomen were monitored to adjust the comprehensive treatment plan.
Diagnosis and treatment
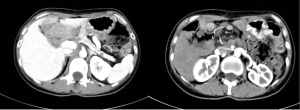
After admission, the patient underwent gene testing in August 2016, which showed low TMB and negative PD-L1 expression. Gemcitabine + nabupaclitaxel (GnP) (3), 5-fluorouracil (5-FU) + leucine + irinotecan + oxaliplatin (FOLFIRINOX) (4), S-1 (5) have been reported in large-scale clinical trials in recent years, and treatment options are increasing. With the increase of therapeutic methods, the therapeutic effect of unresectable pancreatic cancer has improved, but the MST is 8–11 months, which is not satisfactory. Chemotherapy began on September 8, 2016, with the following regimen: GEM 1,000 mg/m2 ivgtt on days 1 and 8, and Capecitabine 1,000 mg/m2/d Po on days 1–14, repeated every 3 weeks for 6 cycles. CT reexamination in March 2017 showed portal recurrence with liver metastasis (Figure 1). Regular chemotherapy was continued. It lasted about 5 months.
In July 2017, CT reexamination showed pancreatic cancer postoperative performance, tail pancreatic nodules, the nature of undetermined multiple hepatic small nodules, and metastases (Figure 2). The multiple lymph nodes in the mesentery and retroperitoneum were enlarged and surrounded the superior artery and vein of the mesentery. We saw local stenosis and occlusion of the superior vein and multiple instances of tortuous thickening collateral circulation in the abdominal cavity. Chemotherapy was changed to irinotecan liposomes 180 mg/m2 on the first day, calcium folinate 400 mg/m2 on the first day, then 5-Fu 2,400 mg/m2 continuously via intravenous injection (IV) for 46 hours, repeated for 2 weeks.
In January 2018, the patient had repeated bleeding of the digestive tract. CT reexamination showed that new soft tissue nodules were found near the anastomosis site of the pancreas and intestine. Multiple nodules were found near the anastomosis of the right side, and retroperitoneal and mesenteric lymph nodes were enlarged, with little change compared with the previous CT examination. The superior mesenteric vein and the splenic vein confluence segment was narrow. Esophageal varies in funds of stomach.
The portal vein stenosis due to tumor invasion was considered and treated with percutaneous transhepatic portal vein stenting after readmission (Figure 3).
In late February 2018, the patient developed intractable edema and ascites in her lower extremities. In early March 2018, she developed jaundice. Reexamination results were the following: white blood cell count =9.55×109/L; red blood cell count =2.23×1012/L; hemoglobin =66 G/L; platelets =166×109/L; total bilirubin =268.8 µmol/L; direct bilirubin =153.9 µmol/L; indirect bilirubin =114.9 µmol/L; albumin =31.8 G/L; alanine transaminase =54.5 IU/L; and aspartate aminotransferase =66 IU/L.
Second MDT discussion and treatment process
MDT discussion
The comments of each team member are reproduced below.
Dr. Hongyu Zhang, chief physician (Hepatobiliary Surgery Pancreatic Group): the patient presented with intractable edema and ascites in both lower limbs in late February 2018. Abdominal b-ultrasound showed a 20 mm interval liquid dark area around the liver and a 120 mm interval liquid dark area in the pelvis cavity. Ascites could not be reduced after correction of hypoalbuminemia. Combined with the CT results, the obstruction caused by tumor compression of the inferior vena cava may be venous obstructive leaky ascites. But the patient had an advanced tumor and local recurrence, therefore liver metastasis was considered, and we also needed to rule out bloody ascites. It was suggested that abdominal paracentesis should be completed, and ascites should be extracted to clarify the cause of the ascites. The patient presented jaundice, which, combined with MRI and CT results, suggested biliary-intestinal anastomotic stricture due to tumor compression. Percutaneous transhepatic cholangio-drainage (PTCD) could effectively reduce the bilirubin level, relieve jaundice, and improve liver function.
Dr. Xuequan Huang (Director, Interventional Radiology Department): in January 2018, the patient presented with recurrent gastrointestinal bleeding. A CT scan showed stenosis of the lumen of the superior mesenteric vein and splenic vein confluence, and esophageal gastric varices. Portal vein stenosis due to the tumor invasion caused portal hypertension, gastric varices, and percutaneous transhepatic portal vein stenting. The results of a B ultrasound, CT, and MRI indicated that the diameter of the main portal vein was 10 mm, the velocity of the right portal vein was 16 cm/S, and the albumin was 41 g/L. Stent implantation is recommended for the treatment of refractory ascites that are caused by stenosis of the inferior vena cava as a result of tumor compression. Inferior vena cava stent implantation is recommended. PTCD is feasible in patients with obstructive jaundice, and biliary-intestinal anastomotic stent implantation should be performed when the whole-body condition permits.
Dr. Qing Ji (Director, Department of Gastroenterology): there are many reasons that ascites develop. We should determine the nature of the ascites as soon as possible to identify the cause. In order to reduce the symptoms caused by ascites, we can carry out necessary symptomatic comprehensive treatment, including limitation of sodium and water intake, correction of hypoalbuminemia, application of diuretics in a manner that gradually increases the dose from a small dose, and strict prevention of electrolyte disorders. If a large amount of ascites affects the patient and they cannot bear the aspiration or abdominal distension symptoms, treatment can be used to alleviate the symptoms. The cause of jaundice was biliary obstruction, which should be relieved as soon as possible. PTCD should be used to relieve the obstruction, but the risk of PTCD was low, and the operation results in a massive loss of bile. We must pay attention to the internal environment disorder, the malnutrition, and other related questions.
Diagnosis and treatment
Inferior vena cava stent implantation was performed by the interventional department (Figure 4). Meanwhile, we continued to strengthen the patient’s nutrition. Hypoalbuminemia was corrected, and diuresis was moderate. The patient’s obstinate ascites gradually reduced, and abdominal distension was alleviated. PTCD was performed later, along with treatment of bilioenteric anastomosis with stent implantation via the PTCD channel. After stent implantation, the patient’s bilirubin significantly decreased and liver function significantly improved (Figure 5). The patient underwent portal vein stenting, inferior vena cava stenting, and bilioenteric anastomotic stenting to solve the problems of portal hypertension, inferior vena cava hypertension, and biliary-intestinal anastomotic stenosis caused by tumor compression. After 1 week, the following stents were seen on CT and abdominal plain film: portal vein stents, inferior vena cava stents, and bilioenteric anastomotic stents (Figure 6).


In May 2018, a CT-guided percutaneous biopsy was performed in the interventional department at the request by the patient and her family (Figure 7). The second gene test and the whole exon gene test were also performed.
The results were as follows: TMB was higher than the Tris (Table 1; Figure 7), and immunotherapy was initiated. The patient was treated with Keytruda and the McAb was administered (2 mg/kg). She returned to Taiyuan in early May 2018 to continue her second-round treatment. Two weeks later, the patient was discharged from hospital. She developed recurrent chills, a high fever, septicemia, and died a month later.
Table 1
| TMB: 108* |
| CNV: 3.13 |
| MSI: 0.00 |
*, exception objective remission rate during immunotherapy:17.59% (5.44/MB). TMB, tumor mutation burden; CNV, copy number variations; MSI, microsatellite instability.
Discussion
In recent years, MDT has been widely used in the field of oncology. The malignant degree of carcinoma of the head of pancreas is high and has a 5-year survival rate of 5% (6). Most patients are diagnosed at an advanced stage, and only about 20–30% of patients are suitable for surgical resection. Even if surgical resection is possible, the patients are likely to have tumor recurrence or metastasis within 1–2 years after the operation, and the MST is only 22–25 months (7). The median survival is only 6–9 months in the patients who had no chance of surgery due to local progression or distant metastasis.
Meanwhile, the clinical diagnosis of pancreatic cancer is difficult and surgical indications are difficult to grasp. Moreover, perioperative and postoperative management is complex, and patients with different conditions need more attention to implement comprehensive diagnosis and treatment. The multi-disciplinary diagnosis and treatment model builds a treatment plan based on each patient’s comprehensive situation, the tumor position, the invasion scope, and the clinical symptoms. Control and the radical treatment of the tumor reduces the related complications, improves the quality of life of patients, and prolongs their survival. In 2014, the guidelines for the diagnosis and treatment of pancreatic cancer developed by the Group of Pancreatic Surgery of the surgical branch of the Chinese Medical Association incorporated the MDT discussion into the routine process of diagnosing pancreatic cancer. MDT evaluation is also recommended as a necessary part of the 2016 National Comprehensive Cancer Network (NCCN) clinical practice guide for pancreatic cancer.
The MDT from the First Affiliated Hospital of the Army Medical University assembled the departments of hepatobiliary and pancreatic surgery, oncology and internal medicine, medical imaging, and interventional medicine and endoscopy. In this case, the patient’s ascites and jaundice symptoms were improved through a combination of interventional and surgical procedures and stent implantation Intervention. Besides endoscopy, chemotherapy, nutrition, immunotherapy, and other means can effectively improve the quality of life and the prognosis of patients.
The patient’s condition changed several times during the course of treatment. After the first-line chemotherapy, the tumor recurred and metastasized, and second-line chemotherapy was used. The portal hypertension led to gastrointestinal bleeding, and with portal vein stenting, gastrointestinal bleeding symptoms were significantly controlled. Stenting through the inferior vena cava solved the problem of refractory ascites that occurred due to the stenosis of the inferior vena cava caused by tumor compression. The obstruction jaundice subsided after the bilioenteric anastomotic stent implantation. After the MDT discussion, a targeted treatment strategy was developed for the patient to improve her quality of life. The quality of life was improved through the collaboration of interventional department and surgical department. The timeline of this patient's treatment is shown in Figure 8.
In the later stage, patients’ compliance became worse, and there was insufficient experience in dealing with immune adverse reactions after PD-L1 was used. Therefore, more guidelines should be combined to strengthen the experience in dealing with immunotherapy complications.
Recently, AJCC, the joint American Cancer Board, released the eighth edition of the TNM (Tumor, Nodes, Metastases) staging system, which revised and updated the seventh edition of the TNM staging system. Non-anatomical parameters such as microsatellite instability, Ras gene, and Braf genotype were introduced as additional predictors of prognosis risk and therapeutic efficacy for colorectal cancer. The evaluation system of tumors has changed from being based on traditional anatomy and morphology to a focus on biology.
The diagnosis of pancreatic cancer, on the other hand, has not yet developed to a similar extent. Typing is still limited to the traditional morphological typing or staging. Clinical treatment depends on empiric therapy; in particular, there is a lack of sensitive chemotherapeutic drugs, targeted therapeutic drugs, immunotherapeutic drugs, and evaluation indicators with targeted therapeutic significance. The MDT model is an effective way to integrate multi-disciplinary advantages, embody precise treatment, and make the best possible individual diagnosis and treatment plan. At the same time, surgeons in clinical diagnosis and treatment are actively changing the system to diagnose and treat pancreatic cancer in a more wholistic way that includes all aspects from morphology to biology and from surgery to oncology to upgrade.
The role of immune negative regulator programmed cell death protein 1 (PD1)/PD-L1 in clinical anti-tumor therapy has attracted increasing attention. It is expressed on the surface of different tumor cells, and its high expression enhances the ability of cancer cells to resist attack by the immune system. PD-L1 is an important factor in tumor occurrence, development, and metastasis. The PD1 inhibitor or PD-L1 inhibitor can stimulate the immune system and restore the activity of T cells by blocking the combination of PD1 and PD-L1, therefore enhancing the anti-tumor immune effect. Currently, PD1/PD-L1 inhibitors have been used in the treatment of lung cancer, melanoma, and renal cell carcinoma. However, a major topic of PD1/PD-L1 blocking therapy is how to enhance the clinical response rate of drugs, improve the therapeutic effect of immunotherapy drugs, establish individual combination therapy, and avoid the side effects of combination therapy. It is also important to explore the mechanism of immunoregulatory molecules and to screen more effective biomarkers to predict the efficacy of PD1/PD-L1 blocking therapy, thereby overcoming side effects and preventing tumor recurrence. At the same time, the establishing a strict evaluation system and a standard immunotherapy, and exploring the mechanism of adverse reactions, may provide a theoretical basis for predicting the prognosis risk and efficacy, and for establishing the corresponding individualized treatment scheme. Molecular approaches based on multi-omics research are promising and will contribute to groundbreaking personalized medicine (8). Immunotherapy is expected to become a routine therapy, as is chemotherapy, for pancreatic cancer patients in the near future.
Conclusions
The treatment of pancreatic cancer starts from early diagnosis, which can improve the surgical resection rate, reduce the invasion of tumor to patients, prolong the overall survival time and improve the quality of life. In clinical practice, pancreatic site examination can be popularized in routine physical examination for patients with family history of pancreatic cancer to improve the early diagnosis rate. Secondly, surgical treatment of pancreatic cancer with metastasis and recurrence combined with multidisciplinary diagnosis and treatment can help patients with symptoms. In this case, patients with gastrointestinal bleeding, ascites and jaundice were actively combined with interventional stent implantation to improve patients’ quality of life and prolong their survival.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-86/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-86/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vincent A, Herman J, Schulick R, et al. Pancreatic cancer. Lancet 2011;378:607-20. [Crossref] [PubMed]
- Burris HA 3rd, Moore MJ, Andersen J, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol 1997;15:2403-13. [Crossref] [PubMed]
- Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 2013;369:1691-703. [Crossref] [PubMed]
- Conroy T, Hammel P, Hebbar M, et al. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N Engl J Med 2018;379:2395-406. [Crossref] [PubMed]
- Ueno H, Ioka T, Ikeda M, et al. Randomized phase III study of gemcitabine plus S-1, S-1 alone, or gemcitabine alone in patients with locally advanced and metastatic pancreatic cancer in Japan and Taiwan: GEST study. J Clin Oncol 2013;31:1640-8. [Crossref] [PubMed]
- Chu QD, Zhou M, Peddi P, et al. Influence of facility type on survival outcomes after pancreatectomy for pancreatic adenocarcinoma. HPB (Oxford) 2017;19:1046-57. [Crossref] [PubMed]
- Li D, Xie K, Wolff R, et al. Pancreatic cancer. Lancet 2004;363:1049-57. [Crossref] [PubMed]
- Barros AG, Pulido CF, Machado M, et al. Treatment optimization of locally advanced and metastatic pancreatic cancer Int J Oncol 2021;59:110. (Review). [Crossref] [PubMed]







