
Preoperative diabetes complicates postsurgical recovery but does not amplify readmission risk following pancreatic surgery
Introduction
Diabetes mellitus is growing in prevalence worldwide. In 2014–2015, approximately 420 million people worldwide had diabetes, representing a staggering 8.5–8.8% of the total adult population, and prevalence is predicted to rise to 10.4% by 2040 (1,2). Without proper control, people with diabetes often develop multiple comorbidities, including ophthalmologic, cardiovascular, and renal complications, including renal failure. In addition, patients often develop microvascular complications leading to poor circulation, infection, and peripheral neurologic deficits. In 2012, 3.7 million deaths were attributable to diabetes and diabetic complications (2).
Patients with diabetes are more likely to require surgery in their lifetimes than non-diabetic patients (3,4). Patients with uncontrolled diabetes and hyperglycemia have increased admission rates to the Intensive Care Unit (ICU), in-hospital mortality, risk of infection, re-operative intervention, and death (5,6). Additionally, diabetic patients’ hospital stays are longer and more expensive than non-diabetics (7-9). In 2007, it was estimated that diabetes-related chronic medical problems in the U.S. cost a total of $116 billion in excess medical costs (10). In 2014, total medical care costs of diabetes were estimated at $827 billion globally (1).
This study reviewed postoperative outcomes in diabetic and non-diabetic patients undergoing partial pancreatectomy, total pancreatectomy, or radical pancreaticoduodenectomy. Our focus was on the risks of postoperative complications, length of stay, in-hospital mortality, readmission risk, and hospital costs in diabetic patients compared to non-diabetic patients. We present the following article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-21-648/rc).
Methods
Data source
A cross-sectional analysis of the National Readmission Database (NRD) from 2010 to 2014 was performed. The NRD is sponsored by the Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases. It contains data from over 14 million discharges per year in over 2,000 hospitals in 22 states (11). International Classification of Disease, 9th revision (ICD-9), was used to define diagnoses and procedures of interest. The study conformed to the provisions of the Declaration of Helsinki (as revised in 2013). The data are deidentified and publicly available, and thus exempt from institutional review board approval, and individual consent for this retrospective analysis was waived.
Study population
The study population included adult (≥18 years) inpatients who underwent major elective pancreatectomy: partial (ICD-9: 5200, 5209, 525, 5251, 5253, 5259, 522, 5221, 5222), total (ICD-9: 526), or radical (ICD-9: 527). Indications for pancreatectomy were classified as functional disorder (ICD-9: 2515, 2518, 2519, 5770, 5771, 5772, 5778, 5779), benign disease (ICD-9: 2116), or malignant disease (ICD-9: 1570, 1571, 1572, 1573, 1578, 1579). Missing data for in-hospital mortality or length of stay were excluded.
Identification of readmission cases
Since patients cannot be traced across calendar years, patient and hospital linkage numbers were used to follow-up all discharge records that belong to the same patient throughout the year. To capture readmissions in NRD within 30- or 90-day following discharge, admission records between January to November or January to September were only captured, respectively, to allow for tracing rehospitalization in 30 or 90 days of the calendar year. Index hospitalization data was combined with the closest rehospitalization data.
Study variables
Patient factors included age, gender, state of residence, median annual household income (categorized into four quartiles), primary insurance type (Medicare, Medicaid, private insurance, self-pay, and other), and a number of chronic diseases. The causes of primary admissions (functional, benign, or malignant conditions) and in-hospital procedures (partial or complete resection) were identified. Cumulative comorbidities were assessed using a modified Charlson Comorbidity Index (CCI) score (12). Patients were given a score based on the number of comorbidities (0, 1, ≥2). Hospital characteristics examined were hospital procedure volume, hospital teaching status (metropolitan teaching, metropolitan non-teaching, and non-metropolitan), and hospital bed size (small, medium, and large).
Study outcomes
The main study outcomes included length of stay (LOS), postoperative complications, mortality, readmission rates at 30 and 90 days, and hospital costs in diabetic and non-diabetic patients undergoing partial pancreatectomy, total pancreatectomy, or radical pancreaticoduodenectomy. Postoperative complications were defined as the dichotomized presence or absence of one or more general or specific complications based on secondary diagnoses during the hospital stay. Complications considered were bleeding/shock, infection/sepsis, technical complications, cardiovascular complications, pulmonary complications, renal complications, endocrine complications, and wound complications (Table S1). Any patient with missing data for any of our main outcomes was removed from the study. The database included hospital charges associated with each admission. Additional files specific to the cost-to-charge ratio for each hospital were supplied by the HCUP, which allows for the conversion of charge values to cost values. Based on All Patients Refined Diagnosis Related Group (DRG) defined by the HCUP, we identified the topmost common diagnosis group on readmission.
Statistical analysis
Statistical analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA) and SPSS version 27.0. Data analysis was performed using weighted measurements to reflect the national estimate level. The recorded weights are available in the NRD data and were calculated based on the stratification variables used. Based on the HCUP user agreement, some variables with low number of observations were not reported to avoid patient tracking. Unbiased and a priori cut-off value of quantitative variables was set at the 75th percentile levels. Therefore, LOS, hospital charge, and hospital cost were classified at a cutoff of 9 days, $97,775.0, and $45,395.2, respectively. Two-tailed ꭓ2 and student’s t-tests were performed regarding postoperative complications, length of stay, and hospital costs comparing non-diabetic and diabetic patients. Diabetic patients were then stratified by (I) type 1 vs. type 2 diabetes, (II) controlled vs. uncontrolled diabetes, and (III) the presence of pre-existing diabetic complications. A two-tailed ꭓ2 test was performed on a stratification analysis detailing the type of postoperative complication when comparing non-diabetic and diabetic patients. Next, a two-tailed ꭓ2 test compared readmission rates and hospital costs at 30 and 90 days between non-diabetic and diabetic patients. Multivariate logistic regression was then performed to calculate adjusted odds ratios of postoperative complications and readmission rates. Odds ratio (OR) and 95% confidence interval (CI) were estimated. Log-rank test was calculated to compare the days to readmission in non-diabetic and diabetic patients.
Results
Characteristics of the study population
A total of 8,401 eligible patients had undergone pancreatic surgery between 2010 and 2014, 25.05% of whom were diabetic. Of the study population, 1,573 patients (20.38%) and 1,683 patients (27.20%) were readmitted within 30 and 90 days of discharge, respectively (Figure 1). On primary admission, the mean age of pancreatic surgery patients was 58.87±10.78 years, and 51.4% were female. The annual prevalence of diabetic patients who required pancreatectomy rose significantly from 17.1% to 23.8% across the five-year study period. Non-insulin-dependent diabetes was the most common type, represented in 1,937 (92.0%) of the patients. About 200 patients (9.5%) had uncontrolled diabetes, and 88 patients (4.2%) had diabetic complications (Figure 2).


A comparison between diabetic and non-diabetic cohorts is shown in Table 1. The mean age of non-diabetic patients was 58.25±14.39 years, and diabetic patients were 60.74±13.19 years old (P<0.001). Women accounted for 53.2% of non-diabetic patients and 46.3% of the diabetic group (P<0.001). Patients who underwent partial and total pancreatectomy represented 29.5% and 3.6% of the sample, respectively, while 66.9% had radical pancreaticoduodenectomy. Diabetic patients were less likely to have a functional disease as the primary admission diagnosis compared to non-diabetic patients (39.7% vs. 44.1%, P<0.001). Subjects with diabetes were more likely to have postoperative complications (33.2% vs. 27.4%, P<0.001) and to be associated with a higher cost (11.9% vs. 9.1%, P<0.001).
Table 1
| Characteristics at primary admission | Levels | Pancreatic surgery | P value | |
|---|---|---|---|---|
| Non-diabetic (N=6,296) | Diabetic (N=2,105) | |||
| Age (year) | Mean ± SD | 58.25±14.39 | 60.74±13.19 | <0.001 |
| >18–45 | 1,222 (19.4) | 290 (13.8) | <0.001 | |
| >45–65 | 2,912 (46.3) | 943 (44.8) | ||
| >65 | 2,162 (34.3) | 872 (41.4) | ||
| Gender | Male | 2,945 (46.8) | 1,131 (53.7) | <0.001 |
| Female | 3,351 (53.2) | 974 (46.3) | ||
| Median annual household income | Quartile 1 lowest | 1,349 (21.9) | 582 (28.4) | <0.001 |
| Quartile 2 | 1,493 (24.3) | 467 (22.8) | ||
| Quartile 3 | 1,514 (24.6) | 518 (25.3) | ||
| Quartile 4 highest | 1,799 (29.2) | 484 (23.6) | ||
| Residence in hospital state | Different state | 1,065 (16.9) | 230 (10.9) | <0.001 |
| Same state | 5,231 (83.1) | 1876 (89.1) | ||
| CCI score | 0 | 5,094 (80.9) | 1505 (71.5) | <0.001 |
| 1 | 972 (15.4) | 383 (18.2) | ||
| ≥2 | 230 (3.7) | 217 (10.3) | ||
| Type of surgical procedure | Partial pancreatectomy/excision | 1,612 (30.2) | 464 (27.4) | 0.007 |
| Total pancreatectomy | 183 (3.4) | 68 (4) | ||
| Radical pancreaticoduodenectomy | 3,538 (66.4) | 1,166 (68.6) | ||
| Cause of surgery | Functional disorders | 1,708 (44.1) | 559 (39.7) | <0.001 |
| Benign disorders | 481 (12.4) | 100 (7.1) | ||
| Malignant disorders | 1,682 (43.5) | 750 (53.2) | ||
| Postoperative complications | None | 4,570 (72.6) | 1,406 (66.8) | <0.001 |
| One or more | 1,727 (27.4) | 699 (33.2) | ||
| LOS, days | Mean ± SD | 8.69±11.34 | 8.13±4.95 | 0.028 |
| Short stay* | 4,489 (71.3) | 1,412 (67) | <0.001 | |
| Long stay | 1,807 (28.7) | 694 (33) | ||
| Hospital charge, $ | Mean ± SD | 90,123.28±122,931.75 | 99,369.85±107,073.95 | 0.003 |
| Low charge* | 4,621 (76.7) | 1,434 (71.3) | <0.001 | |
| High charge | 1,400 (23.3) | 578 (28.7) | ||
| Hospital costs, $ | Mean ± SD | 26,797.33±31,066.51 | 28,566.33±24,245.18 | 0.020 |
| Low cost* | 5,471 (90.9) | 1,772 (88.1) | <0.001 | |
| High cost | 550 (9.1) | 240 (11.9) | ||
| Hospital volume | Low | 1,826 (29) | 738 (35) | <0.001 |
| Medium | 2,964 (47.1) | 848 (40.3) | ||
| High | 1,507 (23.9) | 520 (24.7) | ||
| Hospital type | Metropolitan nonteaching | 537 (8.5) | 200 (9.5) | 0.27 |
| Metropolitan teaching | 5,698 (90.5) | 1,880 (89.3) | ||
| Nonmetropolitan hospital | 62 (1) | 25 (1.2) | ||
| Hospital Bed Size | Small | 326 (5.2) | 129 (6.1) | 0.048 |
| Medium | 805 (12.8) | 299 (14.2) | ||
| Large | 5,165 (82) | 1,678 (79.7) | ||
Data is shown as number (percentage) or mean ± standard deviation (SD). All numbers are presented as weighted national estimates. Two-sided Chi-square and Student’s t-tests were used. Statistical significance was set at P<0.05. *, LOS, cost, and charge were classified based on ≤75th and >75th percentile at a cutoff of 9 days, $97,775.0, and $45,395.2, respectively. Hospital volume (surgeries/year) was divided into ≤25th, ≤75th, and >75th percentiles. CCI, Charlson Comorbidity Index; LOS, Length of stay.
Characteristics of the diabetic patients according to the type of diabetes, presence of diabetic complications, and control status are shown in Table 2. Patients with type 1 diabetes were more likely to have a higher comorbidity score (48.2% vs. 7%, P<0.001) and postoperative complications (64.9% vs. 30.5%, P<0.001) than those with type 2 diabetes. Having controlled diabetes rather than uncontrolled diabetes significantly decreased the chance of postoperative complications (31.3% vs. 51.5%, P<0.001) and required a shorter hospital stay (8.03±4.96 vs. 9.17±4.28 days, P=0.001). The presence or absence of diabetic complications was also considered. Patients with complicated diabetes were more likely to have comorbidities compared to patients with uncomplicated diabetes (25.1% vs. 14.3%, P<0.001). Complicated diabetes patients also had an increased risk of postoperative complications (49.4% vs. 28.8%, P<0.001). Controlled diabetes was associated with a significant reduction in hospital costs compared to uncontrolled ($28,182.21±$24,070.27 vs. $34,171.04±$20,846.61, P=0.001). In contrast, subjects with type 1 diabetes ($62,592.76±$36,238.50 vs. $25,511.12±$20,248.92, P<0.001) or those that had diabetic complications ($47,177.01±$35,085.96 vs. $26,530.02±$28,834.56, P<0.001) incurred higher hospital costs.
Table 2
| Characteristics | Levels | Type of diabetes | Diabetic control | Diabetic complications | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1DM (N=168) | T2DM (N=1,937) | P value | Controlled (N=1,905) | Uncontrolled (N=200) | P value | Uncomplicated (N=2,017) | Complicated (N=88) | P value | ||||
| Age (year) | Mean ± SD | 46.73±13.39 | 61.95±12.45 | <0.001 | 60.08±13.59 | 61.32±12.05 | 0.20 | 58.96±14.09 | 54.16±15.37 | <0.001 | ||
| Gender | Male | 101 (60.5) | 1,030 (53.1) | 0.040 | 1,027 (53.9) | 99 (49.3) | 0.21 | 1,080 (53.6) | 51 (57.5) | 0.41 | ||
| Female | 67 (39.5) | 907 (46.9) | 873 (46.1) | 101 (50.7) | 937 (46.4) | 37 (42.5) | ||||||
| CCI score | 0 | 77 (45.8) | 1,428 (73.7) | <0.001 | 1,372 (72.5) | 132 (68.9) | 0.41 | 1,404 (69.6) | 51 (57.4) | 0.015 | ||
| 1 | 10 (6) | 373 (19.2) | 341 (17.9) | 41 (20.3) | 325 (16.1) | 15 (17.5) | ||||||
| ≥2 | 81 (48.2) | 136 (7) | 189 (9.6) | 22 (10.8) | 288 (14.3) | 22 (25.1) | ||||||
| Postoperative complications | None | 59 (35.1) | 1,347 (69.5) | <0.001 | 1,309 (68.7) | 97 (48.5) | <0.001 | 1,367 (71.2) | 40 (50.6) | <0.001 | ||
| One or more | 109 (64.9) | 590 (30.5) | 596 (31.3) | 103 (51.5) | 650 (28.8) | 48 (49.4) | ||||||
| LOS, days | Mean ± SD | 7.96±3.36 | 8.14±5.07 | 0.64 | 8.03±4.96 | 9.17±4.28 | 0.001 | 8.56±10.25 | 8.10±4.08 | 0.39 | ||
| Hospital costs, $ | Mean ± SD | 62,592.76±36,238.50 | 25,511.12±20,248.92 | <0.001 | 28,182.21±24,070.27 | 34,171.04±20,846.61 | 0.001 | 26,530.02±28,834.56 | 47,177.01±35,085.96 | <0.001 | ||
Data is shown as number (percentage) or mean ± standard deviation (SD). All numbers are presented as weighted national estimates. Two-sided Chi-square and Mann-Whitney U tests were used. Statistical significance was set at P<0.05. LOS, number of chronic diseases and cost were classified based on ≤75th and >75th percentile. CCI, Charlson Comorbidity Index; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; LOS, length of stay.
Risk of postoperative complications, mortality, and readmission
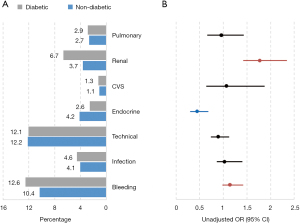
Higher frequencies of postoperative bleeding (12.6% vs. 10.4%, OR: 1.07, 95% CI: 1.25–1.45, P<0.001) and renal complications (6.7% vs. 3.7%, OR: 1.48, 95% CI: 1.84–2.28, P<0.001) were observed in diabetic patients compared to non-diabetic patients (Figure 3), but there was no significant difference in mortality rates at primary admission or within 30 or 90 days after discharge (Figure 4A). However, early and late readmissions were significantly more prevalent among diabetic patients (P=0.014 and <0.001) (Figure 4B). Kaplan-Meier curve showed that both cohort groups had similar readmission times at an average of 10 days (P=0.96). Top causes of readmission are described in Figure 5.

Predictive factors for poor outcomes
As depicted in Table 3, diabetes was associated with a higher risk of postoperative complications (OR: 1.27, 95% CI: 1.08 to 1.49, P=0.003), but posed no significant influence on rehospitalization risk (OR: 1.00, 95% CI: 0.85 to 1.17, P=0.98). Increased length of stay was associated with higher odds of both postoperative complications (OR: 2.50, 95% CI: 2.14 to 2.92, P<0.001) and readmission risk (OR: 1.48, 95% CI: 1.27 to 1.73, P<0.001). Total pancreatectomy (OR: 2.24, 95% CI: 1.50 to 3.35, P<0.001) and admission to nonmetropolitan hospitals (OR: 2.60, 95% CI: 1.06 to 6.40, P=0.037) were found to have an increased risk of readmission. In contrast, having a higher median household income was associated with a lower risk of readmission.
Table 3
| Variables | Levels | Post-operative complications | Readmission | |||||
|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | P value | aOR | 95% CI | P value | |||
| Age (year) | >18–45 | Reference | Reference | |||||
| >45–65 | 1.27 | 1.02, 1.60 | 0.035 | 1.26 | 1.01, 1.59 | 0.043 | ||
| >65 | 1.27 | 1.00, 1.62 | 0.049 | 1.21 | 0.95, 1.54 | 0.11 | ||
| Gender | Male | Reference | Reference | |||||
| Female | 1.00 | 0.86, 1.15 | 0.95 | 0.92 | 0.80, 1.06 | 0.24 | ||
| Median annual household income | Quartile 1 lowest | Reference | Reference | |||||
| Quartile 2 | 0.94 | 0.76, 1.15 | 0.52 | 0.79 | 0.65, 0.97 | 0.027 | ||
| Quartile 3 | 0.77 | 0.63, 0.94 | 0.012 | 0.77 | 0.63, 0.94 | 0.011 | ||
| Quartile 4 highest | 0.70 | 0.58, 0.86 | 0.001 | 0.70 | 0.57, 0.85 | <0.001 | ||
| Type of surgical procedure | Partial pancreatectomy/excision | Reference | Reference | |||||
| Total pancreatectomy | 1.56 | 0.98, 2.48 | 0.05 | 2.24 | 1.50, 3.35 | <0.001 | ||
| Radical pancreaticoduodenectomy | 1.10 | 0.90, 1.33 | 0.35 | 1.15 | 0.95, 1.39 | 0.16 | ||
| Cause of surgery | Non-cancer | Reference | Reference | |||||
| Cancer | 0.27 | 0.23, 0.32 | <0.001 | 0.89 | 0.69, 1.14 | 0.36 | ||
| CCI score | 0 | Reference | Reference | |||||
| 1 | 0.93 | 0.77, 1.12 | 0.45 | 1.03 | 0.86, 1.24 | 0.71 | ||
| ≥2 | 1.09 | 0.76, 1.56 | 0.64 | 2.55 | 1.80, 3.60 | <0.001 | ||
| Diabetic state | Non-diabetic | Reference | Reference | |||||
| Diabetic | 1.27 | 1.08, 1.49 | 0.003 | 1.00 | 0.85, 1.17 | 0.98 | ||
| Postoperative complications | None | NA | NA | NA | Reference | |||
| One or more | NA | NA | 0.92 | 0.79, 1.08 | 0.33 | |||
| Length of stay, days | ≤9 | Reference | Reference | |||||
| >9 | 2.50 | 2.14, 2.92 | <0.001 | 1.48 | 1.27, 1.73 | <0.001 | ||
| Hospital volume | Low | Reference | Reference | |||||
| Medium | 1.00 | 0.83, 1.20 | 0.98 | 1.06 | 0.88, 1.27 | 0.54 | ||
| High | 1.22 | 0.99, 1.50 | 0.06 | 1.07 | 0.86, 1.34 | 0.53 | ||
| Hospital type | Metropolitan nonteaching | Reference | Reference | |||||
| Metropolitan teaching | 1.20 | 0.90, 1.59 | 0.21 | 1.04 | 0.77, 1.39 | 0.80 | ||
| Nonmetropolitan hospital | 0.40 | 0.14, 1.19 | 0.10 | 2.60 | 1.06, 6.40 | 0.037 | ||
All numbers are presented as weighted national estimates. Statistical significance was set at P<0.05. CCI, Charlson Comorbidity Index; aOR, adjust odds ratio.
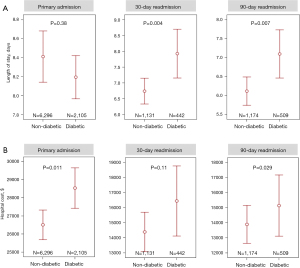
Healthcare burden
Both diabetic and non-diabetic cohorts had similar lengths of stay during primary admission (P=0.38); however, diabetic patients experienced prolonged hospital stays during their 30-day (7.9 days, 95% CI: 7.15–8.64 vs. 6.7 days, 95% CI: 6.35–7.18, P=0.004) and 90-day readmissions (7.1 days, 95% CI: 6.48–7.67 vs. 6.12 days, 95% CI: 5.75–6.5, P=0.007) than non-diabetics, Figure 6A. Conversely, diabetic patients had a higher hospital cost during primary admission than non-diabetic patients (P=0.011) but did not have significantly higher hospital costs during 30- or 90-day readmissions (Figure 6B). National estimates showed an extra 62.7 hospital days and $0.76 million in additional hospital costs per year in diabetic patients.
Discussion
The data here included 8,401 patients who underwent partial pancreatectomy, complete pancreatectomy, or radical pancreaticoduodenectomy between 2010–2014. The study’s main objective was to investigate correlations between the presence of diabetes in patients undergoing those procedures and the risk of postoperative complications, increased hospital length of stay, increased readmission rates, and hospital cost.
We found that having diabetes, particularly type 1 diabetes that was either uncontrolled or complicated, was a risk factor for postoperative complications. These findings are similar to those of multiple previous studies across a variety of surgical procedures (4,12-16). The sample sizes of these other articles vary greatly; our study has one of the larger patient populations. Additionally, only one of the previous papers included patients that had undergone partial or total pancreatectomy or pancreaticoduodenectomy.
While we did not find an increased LOS during primary admission or risk of 30- or 90-day readmission after regression analysis, we found an increase in LOS during both readmission time points for subjects with diabetes. Furthermore, patients who experienced postoperative complications were more likely to have an increased LOS, and increased primary LOS was correlated with an increased risk of subsequent readmission. The type of surgical procedure performed did not influence the rate of postoperative complications when subjected to multivariate regression. Additionally, those who underwent total pancreatectomy were more likely to be readmitted than partial, whereas those undergoing radical pancreaticoduodenectomy were not. In 2019, Passeri et al. looked at 30-day mortality, 30-day readmission, and long-term survival when comparing partial to total pancreatectomy and total pancreatectomy to pancreaticoduodenectomy. Still, they did not report significant differences between the groups (17). A study by Casadei et al. also showed no differences in postoperative outcomes and overall survival between patients who had undergone total pancreatectomy or pancreaticoduodenectomy (18). There was no correlation between total pancreatectomy and increased risk of postoperative complications. This discrepancy in readmission may be due to the larger sample size of our study compared to the others. Passeri et al. noted an increase in the rate of readmission following their 43 total pancreatectomies (5.3% vs. 3.8%); however, it did not reach significance. Our analysis used the NRD, a multi-institutional dataset that includes different settings and volumes of hospitals, whereas the results presented in Casadei et al. were from a single, high-volume, metropolitan institution. The overall rates of all readmissions were higher at non-metropolitan hospitals in our study when compared to metropolitan hospitals. Further insight into the risk factors for readmission for total pancreatectomy patients in this cohort group would be illuminating.
Multiple studies have found that complex operations in high-volume hospitals with more experienced surgeons were protective against negative postoperative outcomes (19-26) as well as readmission rates (27-29). Similarly, Mehta et al. (30) reported that low-volume hospitals were not associated with either complications or 30-day readmission. The data analyzed here showed no increase in the risk of postoperative complications based on hospital volume or location, in accordance with other studies. It did, however, find an increased risk of readmission in non-metropolitan hospitals. This could potentially be indicative of an expansion of the healthcare gap. We found that patients with diabetes compared to non-diabetics, and complicated diabetes compared to uncomplicated were less likely to travel for care. Additionally, being in the lowest quartile of median household income was identified as a risk factor for diabetes. It was associated with a higher risk for postoperative complications and 30- and 90-day readmission when compared to the third and fourth quartiles. Similar findings were published by Hernandez-Meza et al. (27), who found that bottom quartile income was related to an 8% increase in readmission risk. These data indicate that low-income patients with diabetes currently have less access to quality healthcare and are less likely to afford the costs associated with traveling to receive care. Further regionalization and concentration of surgical procedures into metropolitan and high-volume hospitals could inadvertently cause a worsening of the healthcare gap, as access to quality healthcare has been cited as a cause of the socioeconomic health gap (26,31,32). Further studies using the NRD database should be performed to determine the source of these discrepancies.
Additionally, we found that hospital charges and costs were significantly higher in patients with diabetes compared to non-diabetic subjects. Further, those with uncontrolled diabetes had higher expenses and costs than those with controlled diabetes. Umpierrez et al. (6) showed that hyperglycemia was associated with higher mortality rates, longer LOS, and increased ICU admissions. We found similar results when we stratified patients with diabetic complications against those without. It stands to reason that patients with uncontrolled and complicated diabetes (i.e., those predisposed to previously mentioned adverse outcomes) would have higher associated hospital charges and costs, a finding that has been reported in multiple studies (7-9). The complications of uncontrolled and complicated diabetes are preventable; however, national estimates show an excess of 62.7 hospital-days and excess $0.76 million in hospital costs per year in diabetic patients. Therefore, tighter glycemic control post-operatively possibly with insulin drips might mitigate these expected complications and extra expenditure. Considering the complex postoperative medical management, improvement in glycemic control and nutritional status after pancreatectomy further reduced pancreatic exocrine and endocrine insufficiency, and were associated with better survival, and prevented early complications and tumor recurrence (33).
Limitations of this study include the limitations of the NRD patient database itself. Since it tracks in-hospital data, it is possible that several subjects had complications treated in an outpatient setting and were thus not included in the data set. To that end, it is possible that by looking only at patients deemed ill enough to readmit, the study may be predisposed to selection bias. Additionally, this dataset did not have the power to assess for differences in mortality rates between the patient populations in question, which we had initially sought to quantify, and detailed perioperative management plan during hospitalization were not available. However, strength is using the NRD patient database, as it provides a broad scope of hospital data from over 2000 hospitals in 22 states. This data is weighted to represent national averages and should provide an approximation of the impact of diabetes mellitus on pancreatectomy or pancreaticoduodenectomy.
Conclusions
Among patients undergoing pancreatic surgery, those with diabetes were more likely to develop postoperative complications than non-diabetics. Additionally, diabetic patients had higher hospital costs during primary admission and higher rates of 30- and 90-day readmissions. A better understanding of the causes would aid in setting up protective therapeutic strategies.
Acknowledgments
A sincere thank you to Loula Burton from Tulane’s Research Proposal Development Office for her diligent editing and proofreading of this paper.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-21-648/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-21-648/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-21-648/coif). Emad Kandil serves as an Editor-in-Chief of Gland Surgery. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The data are deidentified and publicly available, and thus exempt from institutional review board approval, and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roglic G. WHO Global report on diabetes: A summary. International Journal of Noncommunicable Diseases 2016;1:3. [Crossref]
- World Health O. Global report on diabetes. Geneva: World Health Organization, 2016.
- Clement S, Braithwaite SS, Magee MF, et al. Management of diabetes and hyperglycemia in hospitals. Diabetes Care 2004;27:553-91. [Crossref] [PubMed]
- Umpierrez GE, Smiley D, Jacobs S, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care 2011;34:256-61. [Crossref] [PubMed]
- Kwon S, Thompson R, Dellinger P, et al. Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg 2013;257:8-14. [Crossref] [PubMed]
- Umpierrez GE, Isaacs SD, Bazargan N, et al. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 2002;87:978-82. [Crossref] [PubMed]
- Chen D, Liu S, Tan X, et al. Assessment of hospital length of stay and direct costs of type 2 diabetes in Hubei Province, China. BMC Health Serv Res 2017;17:199. [Crossref] [PubMed]
- Kabeya Y, Shimada A, Tsukada N, et al. Diabetes Affects Length of Stay and Hospital Costs for Elderly Patients with Pneumonia: An Analysis of a Hospital Administrative Database. Tokai J Exp Clin Med 2016;41:203-9. [PubMed]
- Valent F, Tonutti L, Grimaldi F. Does diabetes mellitus comorbidity affect in-hospital mortality and length of stay? Analysis of administrative data in an Italian Academic Hospital. Acta Diabetol 2017;54:1081-90. [Crossref] [PubMed]
- American Diabetes Association. Economic costs of diabetes in the U.S. In 2007. Diabetes Care 2008;31:596-615. [Crossref] [PubMed]
- Introduction to the Hcup Nationwide Readmissions Database (NRD) 2010-2017. Secondary Introduction to the Hcup Nationwide Readmissions Database (NRD) 2010-2017 2019. Available online: https://www.hcup-us.ahrq.gov/db/nation/nrd/Introduction_NRD_2010-2017.jsp
- Cruz NI, Santiago E, Abdul-Hadi A. Prevalence of Diabetes Mellitus in the Surgical Population of the University of Puerto Rico Affiliated Hospitals: A Study using the Surgery Database. P R Health Sci J 2016;35:160-4. [PubMed]
- Lanzetti RM, Lupariello D, Venditto T, et al. The role of diabetes mellitus and BMI in the surgical treatment of ankle fractures. Diabetes Metab Res Rev 2018; [Crossref] [PubMed]
- Alfonso AR, Kantar RS, Ramly EP, et al. Diabetes is associated with an increased risk of wound complications and readmission in patients with surgically managed pressure ulcers. Wound Repair Regen 2019;27:249-56. [Crossref] [PubMed]
- Guzman JZ, Iatridis JC, Skovrlj B, et al. Outcomes and complications of diabetes mellitus on patients undergoing degenerative lumbar spine surgery. Spine (Phila Pa 1976) 2014;39:1596-604. [Crossref] [PubMed]
- Qin C, Vaca E, Lovecchio F, et al. Differential impact of non-insulin-dependent diabetes mellitus and insulin-dependent diabetes mellitus on breast reconstruction outcomes. Breast Cancer Res Treat 2014;146:429-38. [Crossref] [PubMed]
- Passeri MJ, Baker EH, Siddiqui IA, et al. Total compared with partial pancreatectomy for pancreatic adenocarcinoma: assessment of resection margin, readmission rate, and survival from the U.S. National Cancer Database. Curr Oncol 2019;26:e346-56. [Crossref] [PubMed]
- Casadei R, Ricci C, Taffurelli G, et al. Is total pancreatectomy as feasible, safe, efficacious, and cost-effective as pancreaticoduodenectomy? A single center, prospective, observational study. J Gastrointest Surg 2016;20:1595-607. [Crossref] [PubMed]
- Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med 2002;346:1128-37. [Crossref] [PubMed]
- Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med 2003;349:2117-27. [Crossref] [PubMed]
- Hata T, Motoi F, Ishida M, et al. Effect of Hospital Volume on Surgical Outcomes After Pancreaticoduodenectomy: A Systematic Review and Meta-analysis. Ann Surg 2016;263:664-72. [Crossref] [PubMed]
- Ho V, Heslin MJ. Effect of hospital volume and experience on in-hospital mortality for pancreaticoduodenectomy. Ann Surg 2003;237:509-14. [Crossref] [PubMed]
- Xia L, Pulido JE, Chelluri RR, et al. Hospital volume and outcomes of robot-assisted partial nephrectomy. BJU Int 2018;121:900-7. [Crossref] [PubMed]
- Finlayson EV, Goodney PP, Birkmeyer JD. Hospital volume and operative mortality in cancer surgery: a national study. Arch Surg 2003;138:721-5; discussion 726. [Crossref] [PubMed]
- Nguyen NT, Paya M, Stevens CM, et al. The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Ann Surg 2004;240:586-93; discussion 593-4. [Crossref] [PubMed]
- Hauch A, Al-Qurayshi Z, Friedlander P, et al. Association of socioeconomic status, race, and ethnicity with outcomes of patients undergoing thyroid surgery. JAMA Otolaryngol Head Neck Surg 2014;140:1173-83. [Crossref] [PubMed]
- Hernandez-Meza G, McKee S, Carlton D, et al. Association of Surgical and Hospital Volume and Patient Characteristics With 30-Day Readmission Rates. JAMA Otolaryngol Head Neck Surg 2019;145:328-37. [Crossref] [PubMed]
- Babadjouni R, Wen T, Donoho DA, et al. Increased Hospital Surgical Volume Reduces Rate of 30- and 90-Day Readmission After Acoustic Neuroma Surgery. Neurosurgery 2019;84:726-32. [Crossref] [PubMed]
- Ricciardi BF, Liu AY, Qiu B, et al. What Is the Association Between Hospital Volume and Complications After Revision Total Joint Arthroplasty: A Large-database Study. Clin Orthop Relat Res 2019;477:1221-31. [Crossref] [PubMed]
- Mehta A, Efron DT, Canner JK, et al. Effect of Surgeon and Hospital Volume on Emergency General Surgery Outcomes. J Am Coll Surg 2017;225:666-675.e2. [Crossref] [PubMed]
- Andrulis DP. Access to care is the centerpiece in the elimination of socioeconomic disparities in health. Ann Intern Med 1998;129:412-6. [Crossref] [PubMed]
- Liu JH, Zingmond DS, McGory ML, et al. Disparities in the utilization of high-volume hospitals for complex surgery. JAMA 2006;296:1973-80. [Crossref] [PubMed]
- Shi HJ, Jin C, Fu DL. Impact of postoperative glycemic control and nutritional status on clinical outcomes after total pancreatectomy. World J Gastroenterol 2017;23:265-74. [Crossref] [PubMed]



