
Metastasis to lymph nodes at the contralateral entrance point to the recurrent laryngeal nerve in unilateral thyroid papillary carcinoma: a case report and literature review
Introduction
Globally, thyroid cancer is the most common endocrine cancer, and accounts for approximately 2.1% of all newly diagnosed cancers (1). In the United States, the incidence of thyroid cancer has been increasing by an estimated 6% per year (2). In 2020, the American Cancer Society reported that thyroid cancer was the fifth leading cause of cancer in women in the United States, accounting for 4% of all newly diagnosed cancers (3).
Papillary thyroid carcinoma (PTC) is the most common type of thyroid cancer. PTC is slow growing, and prognosis after surgery is excellent; however, PTC is associated with a high incidence of cervical lymph node metastasis, especially central lymph node metastasis (4). The thyroid gland and surrounding tissue have an abundant lymphatic network that facilitates tumor dissemination and lymph node metastasis (5). The central lymph node is the most common site of lymphatic metastasis (5). The main methods for the diagnosis of thyroid cancer and cervical lymph nodes metastasis are ultrasound and fine-needle aspiration (FNA) biopsy, in China, guidelines for the management of patients with thyroid nodules and differentiated thyroid cancer (6) recommend ipsilateral central lymph node dissection while effectively preserving the parathyroid and the recurrent laryngeal nerve.
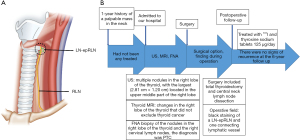
The recurrent laryngeal nerve usually enters the larynx approximately 0.8 cm below the inferior horn of the thyroid cartilage (7). Our clinical experience revealed that the entry point of the recurrent laryngeal nerve is close to the thyroid gland; thus, the recurrent laryngeal nerve is prone to injury during thyroid surgery. Lv et al. identified lymph adipose tissue within 5 mm of the outer edge of the central lymph node to the recurrent laryngeal nerve entrance point as the lymph nodes at the entrance point to the recurrent laryngeal nerve (LNs-epRLN) (8) (Figure 1). Anatomically, the LNs-epRLN are central lymph nodes located in the tracheoesophageal groove, and thus may be overlooked during dissection. Lv et al. showed that the LNs-epRLN are significant in metastasis and recurrence in PTC, and LN-epRLN metastasis was found in 3.76% (33/878) of PTC patients. In this article, we report a rare case of metastasis to the contralateral LN-epRLN in a patient with unilateral thyroid carcinoma.
We present the following article in accordance with the CARE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-46/rc).
Case presentation
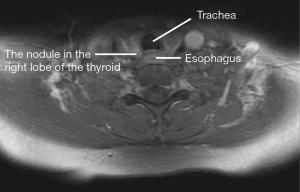
A 45-year-old female was admitted to our hospital with a 1-year history of a palpable mass in the neck that had not been treated. She had no family history of thyroid carcinoma. A cervical ultrasound showed multiple nodules in the right lobe of the thyroid, the largest (2.81 cm × 1.20 cm) of which was located in the upper middle part of the right lobe, and multiple enlarged hypoechoic lymph nodes with an unclear boundary between the cortex and medulla under the inferior pole of the right lobe. Thyroid magnetic resonance imaging showed changes in the right lobe of the thyroid that did not exclude thyroid cancer, and the potential for metastasis to the right lateral lymph node in the bilateral submandibular region (Figure 2). Following a FNA biopsy of the nodules in the right lobe of the thyroid and the right cervical lymph nodes, the patient was diagnosed with PTC.
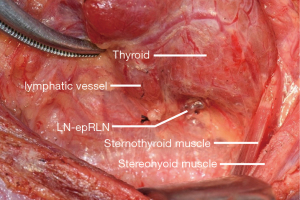
The surgery included a total thyroidectomy and central neck lymph node dissection. 0.2 mL of carbon nanoparticle (CN) suspension was injected into the right lobe of the thyroid. A nerve integrity monitor was used to monitor the electromyography signals of the recurrent laryngeal nerve and vagus nerve. Intraoperative observations showed 3 nodules in the right lobe of the thyroid. Among them, a node in the upper middle part of the right lobe was dorsal to the middle part of the lobe near the recurrent laryngeal nerve entrance point. After the left lobe of the thyroid was removed, the middle thyroid vein was severed and raised inward and upward, which exposed the black staining of a LN-epRLN and 1 connecting lymphatic vessel (Figure 3). The black-stained lymph node was resected, and the pathology results revealed lymph node metastasis from thyroid cancer. Subsequently, the left central lymph nodes and the right lateral lymph nodes were resected.
Postoperatively, the patient experienced no hoarseness or numbness of the extremities. The nodules in the right lobe of the thyroid were diagnosed as PTC by paraffin pathology. The nodules in the upper middle part of the right lobe had invaded the thyroid capsule. The left lobe of the thyroid was not affected. Metastasis from thyroid cancer occurred in the bilateral central lymph nodes and the right lateral lymph node. After surgery, the patient was treated with I131 and levothyroxine sodium tablets (125 µg/day). No adverse or unexpected events were observed during treatment. Her prognosis was good, and there were no signs of recurrence at the 6-year follow up appointment. A timeline is shown in Figure 1.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In PTC, the persistence, progression, and recurrence of cancer are usually localized to the cervical lymph nodes (9). Notably, PTC metastasizes from the central lymph nodes to the ipsilateral cervical and mediastinal lymph nodes (10). Anatomic studies have shown that lymphatic drainage around the thyroid gland is extensive, and extends to 20–30% of the lymph nodes in the body located on either side of the neck (10,11). The lymphatic drainage pathways are accompanied by blood vessels that supply the thyroid gland. Specifically, the lymphatic drainage of the upper pole of the thyroid proceeds along the superior thyroid artery, the lymphatic drainage of the lower thyroid proceeds along the inferior thyroid artery, and the lymphatic pathways drain from the central neck directly to several levels of the lateral neck (11).
FNA has been widely utilized as the sensitive and specific tool in the diagnosis of thyroid cancer and cervical lymph nodes metastasis (12). Intraoperative lymph node evaluation also plays an important role in the surgical management of patients with PTC. In 2007, the Chinese Food and Drug Administration approved the application of CN suspension for lymph node imaging. Since then, CNs have been used as a safe and efficacious lymphatic tracer in gastric cancer, colorectal cancer, breast cancer, and thyroid cancer (13-16). CN suspension is an activated carbon product processed by nanotechnology. CNs have a uniform diameter of 21 nm, and the suspending agents form a stable suspension of carbon pellets that are 150 nm in diameter. These pellets can pass through the 100–500 nm gap in the lymphatic capillary endothelial junction, but cannot pass through the endothelium of capillaries that have a gap size of 30–50 nm. After being injected into the submucosal layer around a tumor, the CNs enter the lymphatic vessels and lymph nodes, are engulfed by macrophages, and dye the lymphatic connections and lymph nodes black, allowing the pathways of the lymphatic drainage around the tumor to be visualized (17), and thus improving the efficiency of lymph node dissection (Table 1). In thyroid cancer, CNs negatively develop and protect the parathyroid glands, which remain unstained, as they have a different lymphatic system from the thyroid gland (15). CNs have few harmful effects and are widely used in cancer surgeries (13,14,16,17,27,28).
Table 1
| Author | Year | Metastatic lymph nodes, n/N (%) | Average number of lymph nodes per patient, mean ± SD | |||
|---|---|---|---|---|---|---|
| With CN | Without CN | With CN | Without CN | |||
| Wang (18) | 2015 | 38/193 (19.7) | 19/123 (15.4) | 6.89±4.15 | 4.56±1.58 | |
| Wang (19) | 2016 | 135/640 (31.2) | 178/769 (23.1) | 7.11±5.40 | 5.45±3.53 | |
| Xu (20) | 2017 | 81/342 (23.7) | 27/261 (10.3) | 6.00±0.98 | 4.58±0.60 | |
| Zhao (21) | 2017 | 43/131 (32.8) | 56/234 (23.9) | – | – | |
| Liu (22) | 2018 | 57/211 (27.01) | 35/166 (21.08) | 4.7±3.0 | 3.5±2.3 | |
| Wang (23) | 2018 | 308/770 (40.9) | 342/982 (34.8) | 11.2±5.7 | 7.7±4.0 | |
| Zhang (24) | 2019 | 45/161 (28.0) | 48/192 (25.0) | – | – | |
| Zhang (25) | 2020 | 330/1,059 (31.2) | 213/872 (24.4) | – | – | |
| Li (26) | 2021 | 189/741 (25.5) | 148/575 (25.7) | 7.72±4.98 | 5.87±4.48 | |
CN, carbon nanoparticle; SD, standard deviation.
In the present case, the patient had unilateral thyroid carcinoma and metastasis to the contralateral LN-epRLN. In China, guidelines for the management of patients with thyroid nodules and differentiated thyroid cancer (6) recommend ipsilateral central lymph node dissection while effectively preserving the parathyroid and the recurrent laryngeal nerve, lateral cervical lymph nodes dissection should be performed in patients with evidence of lateral cervical lymph node metastasis according to ultrasound or FNA. However, 16–24.2% of patients with unilateral thyroid cancer have metastasis of the contralateral central cervical lymph nodes, particularly if the Delphian lymph node is involved (29-31). The lymphatic network in the neck is complex (10), and includes lymphatic drainage into the pre-tracheal and contralateral cervical (inferior jugular) lymph nodes (32).
CN suspension may not successfully locate metastatic lymph nodes if lymphatic vessels are obstructed (e.g., by a tumor thrombus or infection), which may lead to the formation of a collateral lymphatic circulation and altered lymphatic dynamics (33). Our patient had multiple metastatic lymph nodes in the central and lateral neck that may have obstructed the surrounding lymphatic vessels, formed collateral circulation with the periesophageal lymphatic vessels, and caused metastasis to a contralateral LN-epRLN. Notably, there was no obvious lymphatic bed in the pre-tracheal region that connected to the LN-epRLN, which suggests that the lymphatic spread occurred through a different pathway. During surgery, we observed an isolated small black-stained lymphatic vessel on the dorsal side of the right lobe of the thyroid gland, which appeared to be a skip metastasis, and the pathway of lymphatic spread involved the periesophageal lymph node on the dorsal side of the trachea.
Extra-thyroid invasion is a risk factor for cervical lymph node metastasis, and results in poor prognosis in patients with PTC, reducing the recurrence-free survival rate (34-36). The invasion of the thyroid capsule allows the thyroid cancer to spread to nearby structures and lymph nodes. In the present case, the nodule in the upper middle part of the right lobe had invaded the thyroid capsule, and may have directly involved the periesophageal lymphatic vessels, resulting in metastasis to the contralateral LN-epRLN.
Previous reports suggest that the lymph node adjacent to the recurrent laryngeal nerve is among the most common metastatic sites of esophageal cancer, and can be used as the sentinel lymph node (37,38). Esophageal cancer may metastasize to the thyroid gland and the lymph nodes around the thyroid gland. When lymph node metastasis adjacent to the recurrent laryngeal nerve is found, the presence of a primary malignant tumor other than thyroid cancer should be considered.
Conclusions
Thyroid cancer usually metastasizes from the central lymph nodes to the ipsilateral cervical and mediastinal lymph nodes. However, the lymphatic system draining the thyroid gland has not yet been fully described, and retro-tracheal periesophageal lymph node metastasis may be a rare metastatic pathway.
Thyroid cancer is associated with a risk of cervical lymph node metastasis. We recommend routine ipsilateral central lymph node dissection while considering the potential for contralateral central lymph node metastasis and skip metastasis. When lymph node metastasis is suspected, CN suspension can improve the detection rate of metastatic lymph nodes, but may not accurately identify all lymph nodes. Surgical resection extension in thyroid cancer should be informed by a combination of CN suspension, preoperative imaging, and intraoperative pathology.
Acknowledgments
Funding: This work was supported by the Wu Jieping Medical Foundation (No. 320.6750.2020-06-26).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-46/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-46/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kitahara CM, Sosa JA. The changing incidence of thyroid cancer. Nat Rev Endocrinol 2016;12:646-53. [Crossref] [PubMed]
- Morris LG, Sikora AG, Tosteson TD, et al. The increasing incidence of thyroid cancer: the influence of access to care. Thyroid 2013;23:885-91. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020;70:7-30. [Crossref] [PubMed]
- Dou Y, Hu D, Chen Y, et al. PTC located in the upper pole is more prone to lateral lymph node metastasis and skip metastasis. World J Surg Oncol 2020;18:188. [Crossref] [PubMed]
- Sakorafas GH, Sampanis D, Safioleas M. Cervical lymph node dissection in papillary thyroid cancer: current trends, persisting controversies, and unclarified uncertainties. Surg Oncol 2010;19:e57-70. [Crossref] [PubMed]
- Ya M. Interpretation of the management guidelines for patients with thyroid nodules and differentiated thyroid cancer (2012 Chinese edition). Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2013;27:917-20.
- Uen YH, Chen TH, Shyu JF, et al. Surgical anatomy of the recurrent laryngeal nerves and its clinical applications in chinese adults. Surg Today 2006;36:312-5. [Crossref] [PubMed]
- Lv T, Liu Z, Yan J. Lymph node metastasis around the entrance point to recurrent laryngeal nerve in papillary thyroid carcinoma. Sci Rep 2020;10:5433. [Crossref] [PubMed]
- Robinson TJ, Thomas S, Dinan MA, et al. How Many Lymph Nodes Are Enough? Assessing the Adequacy of Lymph Node Yield for Papillary Thyroid Cancer. J Clin Oncol 2016;34:3434-9. [Crossref] [PubMed]
- Likhterov I, Reis LL, Urken ML. Central compartment management in patients with papillary thyroid cancer presenting with metastatic disease to the lateral neck: Anatomic pathways of lymphatic spread. Head Neck 2017;39:853-9. [Crossref] [PubMed]
- Pai SI, Tufano RP. Central compartment neck dissection for thyroid cancer. Technical considerations. ORL J Otorhinolaryngol Relat Spec 2008;70:292-7. [Crossref] [PubMed]
- Wang TX, Song YT, Xu GH, et al. Fine-needle aspiration for the diagnosis of lymph node metastasis in papillary thyroid carcinoma. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2019;54:23-7. [PubMed]
- Yan J, Zheng X, Liu Z, et al. A multicenter study of using carbon nanoparticles to show sentinel lymph nodes in early gastric cancer. Surg Endosc 2016;30:1294-300. [Crossref] [PubMed]
- Wang R, Mo S, Liu Q, et al. The safety and effectiveness of carbon nanoparticles suspension in tracking lymph node metastases of colorectal cancer: a prospective randomized controlled trial. Jpn J Clin Oncol 2020;50:535-42. [Crossref] [PubMed]
- Huang K, Luo D, Huang M, et al. Protection of parathyroid function using carbon nanoparticles during thyroid surgery. Otolaryngol Head Neck Surg 2013;149:845-50. [Crossref] [PubMed]
- Hao RT, Chen J, Zhao LH, et al. Sentinel lymph node biopsy using carbon nanoparticles for Chinese patients with papillary thyroid microcarcinoma. Eur J Surg Oncol 2012;38:718-24. [Crossref] [PubMed]
- Du J, Zhang Y, Ming J, et al. Evaluation of the tracing effect of carbon nanoparticle and carbon nanoparticle-epirubicin suspension in axillary lymph node dissection for breast cancer treatment. World J Surg Oncol 2016;14:164. [Crossref] [PubMed]
- Wang B, Qiu NC, Zhang W, et al. The role of carbon nanoparticles in identifying lymph nodes and preserving parathyroid in total endoscopic surgery of thyroid carcinoma. Surg Endosc 2015;29:2914-20. [Crossref] [PubMed]
- Wang B, Du ZP, Qiu NC, et al. Application of carbon nanoparticles accelerates the rapid recovery of parathyroid function during thyroid carcinoma surgery with central lymph node dissection: A retrospective cohort study. Int J Surg 2016;36:164-9. [Crossref] [PubMed]
- Xu XF, Gu J. The application of carbon nanoparticles in the lymph node biopsy of cN0 papillary thyroid carcinoma: A randomized controlled clinical trial. Asian J Surg 2017;40:345-9. [Crossref] [PubMed]
- Zhao WJ, Luo H, Zhou YM, et al. Preoperative ultrasound-guided carbon nanoparticles localization for metastatic lymph nodes in papillary thyroid carcinoma during reoperation: A retrospective cohort study. Medicine (Baltimore) 2017;96:e6285. [Crossref] [PubMed]
- Liu Y, Li L, Yu J, et al. Carbon nanoparticle lymph node tracer improves the outcomes of surgical treatment in papillary thyroid cancer. Cancer Biomark 2018;23:227-33. [Crossref] [PubMed]
- Wang B, Su AP, Xing TF, et al. The function of carbon nanoparticles to improve lymph node dissection and identification of parathyroid glands during thyroid reoperation for carcinoma. Medicine (Baltimore) 2018;97:e11778. [Crossref] [PubMed]
- Zhang X, Shen YP, Li JG, et al. Clinical feasibility of imaging with indocyanine green combined with carbon nanoparticles for sentinel lymph node identification in papillary thyroid microcarcinoma. Medicine (Baltimore) 2019;98:e16935. [Crossref] [PubMed]
- Zhang D, Fu Y, Dionigi G, et al. A Randomized Comparison of Carbon Nanoparticles in Endoscopic Lymph Node Dissection Via the Bilateral Areola Approach for Papillary Thyroid Cancer. Surg Laparosc Endosc Percutan Tech 2020;30:291-9. [Crossref] [PubMed]
- Li T, Ma Z, Lu C, et al. Application of carbon nanoparticles combined with intraoperative neuromonitoring in papillary thyroid microcarcinoma surgery. Am J Otolaryngol 2021;42:102790. [Crossref] [PubMed]
- Xie P, Xin Q, Yang ST, et al. Skeleton labeled 13C-carbon nanoparticles for the imaging and quantification in tumor drainage lymph nodes. Int J Nanomedicine 2017;12:4891-9. [Crossref] [PubMed]
- Cai HK, He HF, Tian W, et al. Colorectal cancer lymph node staining by activated carbon nanoparticles suspension in vivo or methylene blue in vitro. World J Gastroenterol 2012;18:6148-54. [Crossref] [PubMed]
- Chen Q, Wei T, Wang XL, et al. The total number of prelaryngeal and pretracheal lymph node metastases: is it a reliable predictor of contralateral central lymph node metastasis in papillary thyroid carcinoma? J Surg Res 2017;214:162-7. [Crossref] [PubMed]
- Wada N, Duh QY, Sugino K, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 2003;237:399-407. [Crossref] [PubMed]
- Kim WW, Park HY, Jung JH. Surgical extent of central lymph node dissection in clinically node-negative papillary thyroid cancer. Head Neck 2013;35:1616-20. [Crossref] [PubMed]
- Sahin M, Yapici O, Dervisoglu A, et al. Evaluation of lymphatic drainage of cold thyroid nodules with intratumoral injection of Tc-99m nanocolloid. Clin Nucl Med 2001;26:602-5. [Crossref] [PubMed]
- Som PM. Lymph nodes of the neck. Radiology 1987;165:593-600. [Crossref] [PubMed]
- Lin JD, Chao TC, Weng HF, et al. Prognostic variables of papillary thyroid carcinomas with local invasion. Endocr J 1999;46:91-8. [Crossref] [PubMed]
- Hotomi M, Sugitani I, Toda K, et al. A novel definition of extrathyroidal invasion for patients with papillary thyroid carcinoma for predicting prognosis. World J Surg 2012;36:1231-40. [Crossref] [PubMed]
- Chéreau N, Buffet C, Trésallet C, et al. Does extracapsular extension impact the prognosis of papillary thyroid microcarcinoma? Ann Surg Oncol 2014;21:1659-64. [Crossref] [PubMed]
- Ma L, Xiang J, Zhang Y, et al. Characteristics and clinical significance of recurrent laryngeal nerve lymph node metastasis in esophageal squamous cell carcinoma. J BUON 2017;22:1533-9. [PubMed]
- Xu J, Zheng B, Zhang S, et al. The clinical significance of the intraoperative pathological examination of bilateral recurrent laryngeal nerve lymph nodes using frozen sections in cervical field lymph node dissection of thoracic esophageal squamous cell carcinoma. J Thorac Dis 2019;11:3525-33. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


