
Influence of progesterone receptor on metastasis and prognosis in breast cancer patients with negative HER-2
Introduction
The dramatic increase in breast cancer survival in recent years (since the 1970s) has been attributed to the discovery of hormone receptors (HRs), human epidermal factor growth receptor 2 (HER-2) and the widespread use of endocrine and targeted therapies. Hormone receptor-positive breast cancer, which is referred to as Luminal type breast cancer [estrogen receptor (ER)+ and/or progesterone receptor (PR)+], accounts for 70% of all patients, and is associated with better reactivity to endocrine treatment and better prognosis than hormone receptor-negative breast cancer (1,2). Later, Ki67 was regarded as an important criterion for distinguishing Luminal A and Luminal B breast cancers and guidelines divided Luminal B breast cancer into two categories based on the HER-2 status (3). However, in recent years, much evidence has indicated that ER+/PR− patients experience more invasive clinical pathological characteristics and worse prognosis than ER+/PR+ patients (4,5). The 2013 St. Gallen conference introduced the Luminal B-like subtype, which includes HER-2 negativity, ER positivity and at least one of a ‘negative or low level’ of PR or a ‘high’ Ki67 index (6), emphasizing the important impact of single positive hormone receptor [PR loss or low expression (≤20%)] on breast cancer patient survival. However, clinical immunohistochemical analysis showed another rare single hormone-positive result (ER−/PR+) that was not clearly defined or classified by St. Gallen conference (7). PR was previously thought to be an activated nuclear transcription factor that mediates the action of progesterone, and the activation process depended on the involvement of estrogen and its receptor (8,9). Therefore, there was a controversy that whether ER−/PR+ is an error or entity. Ren et al. analyzed breast cancer in the Surveillance, Epidemiology and End Results (SEER) database and found that ER−/PR+ cases still existed from 1990 to 2015 and maintained a relatively stable proportion after 2010. Moreover, the overall survival (OS) and cancer-specific survival (CSS) of patients with this subtype differed from those with the ER+/PR+ and ER−/PR− subtypes (10). It was confirmed that the ER−/PR+ subtype exists independently of the other subtypes.
At present, for metastatic breast cancer, retrospective and basic studies have been proved that molecular subtypes determine the propensity for metastasis. For example, ER+ breast cancer patients are more prone to bone metastases and prolonged OS than ER− patients (11,12). Patients with TNBC have a poor prognosis because they are likely to develop lung, liver, and brain metastases and there is no effective treatment other than chemotherapy (13,14). Previous studies based on SEER database, neglected the effect of PR negativity or presence alone on the prognosis of stage IV breast cancer patients (15). Single-hormone receptor-positive (ER−/PR+) studies exploring differences in stage IV breast cancer metastatic patterns and prognosis are rare.
Therefore, our cohort study focused on metastasis mode of single positive PR and survival risk from ER−/PR+ subtype in IV stage patients. we examined HER-2 receptor-negative de novo metastatic breast cancer patients in the SEER database from 2010 to 2015, analyzed distribution of sites of metastasis between four HR statues in patients with stage IV breast cancer, and investigated the effect of single HR positivity on the risk of metastasis and the risk factors and protective factors for CSS in a single HR-positive cohort. We present the following article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-21-677/rc).
Methods
Data source and inclusion criteria
The US cancer SEER database is the largest cancer database in North America, accounting for approximately 34.6% of the US population. The cohort study conformed to the provisions of the Declaration of Helsinki (as revised in 2013). We used SEER*Stat 8.3.5 to extract the clinicopathological, therapeutic, and prognostic data in patients diagnosed with breast cancer between 2010 and 2015 for the HER-2 status and specific sites of metastasis in stage IV patients were recorded only after 2010. All included patients were followed up until December 2016. The inclusion criteria were as follows: (I) patients with primary stage I-IV breast cancer; (II) patients not diagnosed with other malignancies before the follow-up deadline; (III) HER-2 status was negative. The exclusion criteria were as follows: (I) male breast cancer patients; (II) breast cancer patients not confirmed by histopathology; (III) an unknown or borderline ER or PR status; (IV) unknown site of distant metastasis; (V) no clear cause of death, an incomplete follow-up status and survival data. Ultimately, 206,187 patients who were diagnosed with HER-2-negative breast cancer between 2010 and 2015 were included (Figure 1).
Variables and endpoints
The following variables extracted from the SEER database as possible risk factors for stage IV breast cancer and prognosis included the year of diagnosis, age at diagnosis, race, marital status, insurance record, tumor site, AJCC T stage, AJCC N stage, pathological type, histological grade, postoperative positive lymph nodes, surgical methods, radiation therapy, and chemotherapy. The main endpoints were overall survival (OS) and cancer specific survival (CSS).
Statistical analysis and ethic statement
We used the ER and PR status for a more detailed breast cancer clinical subtype stratification (ER+/PR+, ER+/PR−, ER−/PR+, ER−/PR−), and descriptive statistics and χ2 tests were used to analyze the baseline characteristics differences of breast cancer patients among the four subtypes (categorical variables are presented as percentages). Meanwhile, the constituent ratios of metastasis modes including single bone or viscera (brain, liver, or lung) metastasis, bone metastasis combined with one site metastasis of viscera and multiple visceral metastases were calculated according to the clinical subtype. Risk factors for bone metastases or visceral metastases in breast cancer patients were investigated by multivariable analysis. Further, Kaplan-Meier survival curves were used to evaluate the OS and CSS of breast cancer patients in different subgroups. The log-rank test was used to test the significant difference in survival curves. A multivariate Cox proportional hazard regression model was used to estimate CSS in subgroups [(I) all HER-2-negative breast cancer patients; (II) stage I–III breast cancer patients; (III) stage IV breast cancer patients including all breast cancer patients with distant metastasis; (IV) breast cancer patients with only one bone metastasis or visceral metastasis; (V) patients with multiple visceral metastases] after adjusting for the diagnosis age at diagnosis, insurance status, marital status, race, tumor size, lymph node status, distant metastasis, tumor grade and histological type, surgical method, radiotherapy, and chemotherapy. At last, we also performed a multivariate Cox analysis in ER+/PR− and ER−/PR+ breast cancer patients to identified independent risk and protective factors for CSS. The P<0.05 indicates statistical significance. All statistical analyses were performed using SPSS 23.0.
This research proposal was reviewed and approved by the Ethics Committee of the Union Hospital, Tongji Medical College of Huazhong University of Science and Technology.
Results
Clinicopathologic features of four breast cancer subtypes
We retrospectively examined 206,187 female patients diagnosed with invasive breast cancer including 198,461 (96.25%) patients with stage I–III breast cancer and 7,726 (3.75%) patients with stage IV breast cancer. And a total of 155,021 (75.18%) patients were ER+/PR+ subtype, 20,755 (10.07%) patients were ER+/PR− subtype, 1,837 (0.89%) patients were ER−/PR+ subtype, 28,574 (13.86%) patients were ER−/PR− subtype. As shown in Table 1, all variables showed significant differences among four hormone receptor status. The clinicopathological features of ER−/PR+ and ER−/PR− subtype are similar. Comparing with ER+/PR+ and ER+/PR− subtypes, the characteristics of subtype with negative ER status had younger age (≤40 years old: respectively, 11.76% and 11.15%), high percentage of black patients (respectively, 20.25% and 20.64%), lower proportion of insured status (respectively, 79.91% and 81.09%), higher proportion of infiltrating ductal carcinoma (respectively, 85.41% and 84.80%), advanced grade (III–IV grade: respectively, 79.64% and 77.37%), larger tumor size (T4: respectively, 6.42% and 6.49%) and worse lymph node status (N3 stage: respectively, 4.41% and 4.75%). Regarding characteristics and treatment, ER−/PR+ and triple negative groups underwent higher percentage of mastectomy (respectively, 21.77% and 22.07%), radical surgery (respectively, 16.93% and 19.23%) and chemotherapy (respectively, 71.64% and 75.29%). However, patients with ER+/PR+ subtype accounted for a highest incidence in radiation (55.50%) and ER+/PR− subtype have a highest proportion of percentage of de novo metastatic breast cancer (5.39%).
Table 1
| ER+/PR+ | ER+/PR− | ER−/PR+ | ER−/PR− | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||||
| Age, years | |||||||||||
| ≤40 | 7,984 | 5.15 | 1,187 | 5.72 | 216 | 11.76 | 3,185 | 11.15 | |||
| 41–55 | 46,984 | 30.31 | 4,962 | 23.91 | 721 | 39.25 | 9,900 | 34.65 | |||
| 55–70 | 62,128 | 40.08 | 9,014 | 43.43 | 602 | 32.77 | 10,179 | 35.62 | |||
| 71–85 | 32,897 | 21.22 | 4,670 | 22.50 | 254 | 13.83 | 4,502 | 15.76 | |||
| >85 | 5,028 | 3.24 | 922 | 4.44 | 44 | 2.40 | 808 | 2.83 | |||
| Race | |||||||||||
| White | 125,545 | 80.99 | 15,823 | 76.24 | 1,319 | 71.80 | 20,317 | 71.10 | |||
| Black | 13,579 | 8.76 | 2,923 | 14.08 | 372 | 20.25 | 5,897 | 20.64 | |||
| Other | 14,751 | 9.52 | 1,879 | 9.05 | 135 | 7.35 | 2,195 | 7.68 | |||
| Marital | |||||||||||
| Yes | 86,767 | 55.97 | 10,950 | 52.76 | 992 | 54.00 | 15,231 | 53.30 | |||
| No | 60,329 | 38.92 | 8,660 | 41.72 | 750 | 40.83 | 11,834 | 41.42 | |||
| Unknown | 7,925 | 5.11 | 1,145 | 5.52 | 95 | 5.17 | 1,509 | 5.28 | |||
| Insurance | |||||||||||
| Insured | 133,365 | 86.03 | 17,540 | 84.51 | 1,468 | 79.91 | 23,170 | 81.09 | |||
| Any Medicaid | 16,704 | 10.78 | 2,546 | 12.27 | 302 | 16.44 | 4,275 | 14.96 | |||
| Uninsured | 2,340 | 1.51 | 344 | 1.66 | 41 | 2.23 | 707 | 2.47 | |||
| Histology | |||||||||||
| IDC | 111,865 | 72.16 | 14,844 | 71.52 | 1,569 | 85.41 | 24,232 | 84.80 | |||
| LC | 17,270 | 11.14 | 2,792 | 13.45 | 23 | 1.25 | 301 | 1.05 | |||
| IDC + LC | 10,593 | 6.83 | 1,075 | 5.18 | 29 | 1.58 | 332 | 1.16 | |||
| Others | 14,690 | 9.48 | 1,830 | 8.82 | 195 | 10.62 | 3,304 | 11.56 | |||
| Grade | |||||||||||
| I–III | 123,641 | 79.76 | 12,048 | 58.05 | 301 | 16.39 | 5,119 | 17.91 | |||
| III–IV | 25,843 | 16.67 | 7,648 | 36.85 | 1,463 | 79.64 | 22,109 | 77.37 | |||
| T | |||||||||||
| ≤ T1 | 99,702 | 64.32 | 10,931 | 52.67 | 743 | 40.45 | 11,775 | 41.21 | |||
| T2 | 41,339 | 26.67 | 6,829 | 32.90 | 789 | 42.95 | 11,811 | 41.33 | |||
| T3 | 7,826 | 5.05 | 1,555 | 7.49 | 151 | 8.22 | 2,562 | 8.97 | |||
| T4 | 3,868 | 2.50 | 968 | 4.66 | 118 | 6.42 | 1,854 | 6.49 | |||
| N | |||||||||||
| N0 | 108,506 | 69.99 | 13,617 | 65.61 | 1,191 | 64.83 | 18,026 | 63.09 | |||
| N1 | 34,520 | 22.27 | 4,862 | 23.43 | 467 | 25.42 | 7,194 | 25.18 | |||
| N2 | 7,275 | 4.69 | 1,234 | 5.95 | 86 | 4.68 | 1,751 | 6.13 | |||
| N3 | 3,717 | 2.40 | 839 | 4.04 | 81 | 4.41 | 1,356 | 4.75 | |||
| Surgery | |||||||||||
| No | 9,024 | 5.82 | 1,782 | 8.59 | 168 | 9.15 | 2,549 | 8.92 | |||
| BCS | 93,935 | 60.60 | 11,187 | 53.90 | 946 | 51.50 | 13,929 | 48.75 | |||
| Mastectomy | 31,624 | 20.40 | 4,270 | 20.57 | 400 | 21.77 | 6,305 | 22.07 | |||
| Radical surgery | 19,287 | 12.44 | 3,364 | 16.21 | 311 | 16.93 | 5,496 | 19.23 | |||
| Radiation | |||||||||||
| Yes | 86,036 | 55.50 | 10,884 | 52.44 | 942 | 51.28 | 14,108 | 49.37 | |||
| No/Unknown | 68,985 | 44.50 | 9,871 | 47.56 | 895 | 48.72 | 14,466 | 50.63 | |||
| Chemotherapy | |||||||||||
| Yes | 43,586 | 28.12 | 9,400 | 45.29 | 1316 | 71.64 | 21,512 | 75.29 | |||
| No/unknown | 111,435 | 71.88 | 11,355 | 54.71 | 521 | 28.36 | 7,062 | 24.71 | |||
| M | |||||||||||
| I–III | 149,955 | 96.73 | 19,637 | 94.61 | 1,744 | 94.94 | 27,125 | 94.93 | |||
| IV | 5,066 | 3.27 | 1,118 | 5.39 | 93 | 5.06 | 1,449 | 5.07 | |||
Grade: I, well differentiated; II, moderately differentiated; III, poorly differentiated; IV, undifferentiated. BCS, breast conserving surgery. ER, estrogen receptor; PR, progesterone receptor; IDC, intraductal carcinoma.
Table 2 showed the proportion of metastatic patterns grouped by the four subtypes (P<0.001). For ER+/PR+, a higher proportion of patients had bone metastases only (2,767; 54.62%), and bone +one site visceral metastasis accounted for the highest percentage of multiple metastases in these patients (1,153, 22.76%). Almost half of the ER+/PR− patients were confirmed to have single bone metastasis (540, 48.30%) and there were 192 (17.17%) patients with only one site visceral metastasis (including lung, liver, and brain). Bone + one site visceral metastasis was also the most common multiple metastasis (257, 22.99%) in such subtype. Patients with ER deficiency (ER−/PR+) had a lower proportion of single bone metastasis but a higher of singe visceral metastasis (39, 41.94%), and two different patterns of multiple metastasis accounted a similar proportion (23.66% versus 20.43%) in those patients. Among the patients with triple-negative breast cancer (TNBC), patients with single visceral metastases (541, 37.34%) had a high proportion of one site metastases. And those patients with bone added one site of visceral metastasis (265, 18.29%) and multiple visceral metastases (283, 19.53%) also accounted for a similar proportion.
Table 2
| ER+/PR+ | ER+/PR− | ER−/PR+ | ER−/PR− | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (N=5,066) | % | (N=1,118) | % | (N=93) | % | (N=1,449) | % | ||||
| One site | |||||||||||
| Bone | 2,767 | 54.62 | 540 | 48.30 | 13 | 13.98 | 360 | 24.84 | |||
| Viscera | 666 | 13.15 | 192 | 17.17 | 39 | 41.94 | 541 | 37.34 | |||
| Multi-sites | |||||||||||
| Bone + one site of viscera | 1,153 | 22.76 | 257 | 22.99 | 22 | 23.66 | 265 | 18.29 | |||
| ≥ Two sites of viscera | 480 | 9.47 | 129 | 11.54 | 19 | 20.43 | 283 | 19.53 | |||
Viscera including liver, brain or lung. *, P values were calculated among all groups using a chi-squared test and P<0.001. ER, estrogen receptor; PR, progesterone receptor.
Metastasis risk from single PR negativity or positivity
Table 3 shown the results that potential independent factor for bone metastasis or visceral metastasis in all cases and reference group was M0 group, after adjusting for age at diagnosis, race, histology, grade, T stage, N stage, and HR status, the multivariate regression analysis showed that age >85 years old and mixed duct and lobular carcinoma was a protective factors for the occurrence of bone metastases (including only bone metastasis and bone + other metastasis). Older age but <85 years, black race and ER positivity were risk factors for bone metastasis (55–70 years old: OR 1.27, P<0.001; 71–85 years old: OR 1.31, P<0.001) (Black: OR 1.14, P=0.002) (ER+/PR−: OR 2.03, P<0.001; ER+/PR+: OR 1.97, P<0.001:) Furthermore, as the AJCC stage increased, the risk of bone metastasis also increased (T2: OR 3.89, P<0.001; T3: OR 8.44, P<0.001; T4: OR 35.47, P<0.001; N1: OR 3.07, P<0.001; N2: OR 2.44, P<0.001; N3: OR 4.40, P<0.001). A high grade, invasive lobular carcinoma and single PR positivity had no association with bone metastases. In another cohort, older age (55–70 years: OR 1.50, P<0.001; 71–85 years: OR 1.59, P<0.001;), race (black OR 1.24, P<0.003), a high grade (III-IV: OR 1.19, P<0.001), a large tumor size (T2: OR 3.95, P<0.001; T3: OR 11.21, P<0.001; T4: OR 44.91, P<0.001), a high N stage (N1: OR 3.06, P<0.001; N2: OR 2.13, P<0.001; N3: OR 3.89, P<0.001), were identified as high-risk factors for visceral metastasis. In contrast to bone metastasis, ER and PR positivity, invasive lobular carcinoma, and mixed cancer and lobular carcinoma were protective factors for visceral metastasis (lobular carcinoma: OR 0.52, P<0.001; invasive ductal carcinoma+ lobular carcinoma: OR 0.58, P<0.001).
Table 3
| Bone metastasis | Visceral metastasis | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | ||
| Age at diagnosis (vs. ≤40) | |||||||
| ≤40 [571] | |||||||
| 41–55 [2,013] | 0.93 | 0.83–1.04 | 0.200 | 1.01 | 0.88–1.16 | 0.930 | |
| 55–70 [3,103] | 1.27 | 1.14–1.42 | <0.001 | 1.50 | 1.31–1.71 | <0.001 | |
| 71–85 [1,708] | 1.31 | 1.16–1.48 | <0.001 | 1.59 | 1.6–2.52 | <0.001 | |
| >85 [331] | 0.66 | 0.55–0.79 | <0.001 | 1.06 | 1.62–2.86 | 0.577 | |
| Race recodes (vs. White) | |||||||
| White [5,806] | |||||||
| Black [1,314] | 1.14 | 1.05–1.23 | 0.002 | 1.24 | 1.13–1.35 | <0.001 | |
| Histology (vs. IDC) | |||||||
| IDC [5,280] | |||||||
| LC [945] | 1.07 | 0.99–1.17 | 0.10 | 0.52 | 0.45–0.60 | <0.001 | |
| IDC + LC [356] | 0.87 | 0.77–0.99 | 0.03 | 0.58 | 0.48–0.70 | <0.001 | |
| Grade (vs. I–II) | |||||||
| I–II [3,430] | |||||||
| III–IV [2,857] | 1.03 | 0.96–1.10 | 0.49 | 1.19 | 1.10–1.30 | <0.001 | |
| AJCC T Stage (vs. ≤ T1) | |||||||
| ≤ T1 [889] | |||||||
| T2 [2,277] | 3.89 | 3.55–4.26 | <0.001 | 3.95 | 3.50–4.47 | <0.001 | |
| T3 [1,241] | 8.44 | 7.58–9.41 | <0.001 | 11.21 | 9.78–12.86 | <0.001 | |
| T4 [2,385] | 35.47 | 32.00–39.32 | <0.001 | 44.91 | 39.49–51.07 | <0.001 | |
| AJCC N Stage (vs. N0) | |||||||
| N0 [1,798] | |||||||
| N1 [3,418] | 3.07 | 2.86–3.31 | <0.001 | 3.06 | 2.80–3.35 | <0.001 | |
| N2 [864] | 2.44 | 2.19–2.71 | <0.001 | 2.13 | 1.88–2.43 | <0.001 | |
| N3 [1,035] | 4.40 | 3.96–4.89 | <0.001 | 3.89 | 3.43–4.01 | <0.001 | |
| HR status (vs. TNBC) | |||||||
| TNBC [1,449] | |||||||
| ER+/PR− [1,118] | 2.03 | 1.82–2.27 | <0.001 | 1.01 | 0.90–1.13 | 0.901 | |
| ER−/PR+ [93] | 1.05 | 0.76–1.45 | 0.756 | 1.25 | 0.96–1.61 | 0.097 | |
| ER+/PR+ [5,066] | 1.97 | 1.80–2.17 | <0.001 | 0.84 | 0.77–0.92 | <0.001 | |
ER, estrogen receptor; PR, progesterone receptor; IDC, intraductal carcinoma; TNBC, triple-negative breast cancer.
Survival analysis
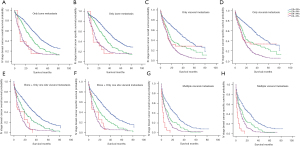
In our cohort study, survival analysis using the Kaplan-Meier curve and log-rank test showed that until December 2016, the average follow-up time was 41.06±21.06 months. In all patients with negative HER-2 status, the 5-year OS and BCSS rates of ER+/PR+ patients were the best (92.65% and 96.07%, respectively), followed by ER+/PR− patients (5-year OS: 85.40%, 5-year BCSS: 89.67%), ER−/PR+ patients (5-year OS: 80.57%, 5-year BCSS: 83.61%), and ER−/PR− patients (5-year OS: 79.42%, 5-year BCSS: 83.12%) (Figure S1). Among all the included 7,726 patients with stage IV breast cancer in Figure S1C,S1D, 4,935 (63.88%) died after an average follow-up time of 23.73±19.33 months, The 5-year OS and BCSS rates were highest in patients with the ER+/PR+ subtype (5-year OS: 45.85%, 5-year BCSS: 50.83%, median survival time of 40.21 months), followed by those with the ER+/PR− subtype (5-year OS: 30.14%, 5-year BCSS: 34.53, median survival time of 28.05 months), ER−/PR+ subtype (5-year OS: 18.28%, 5-year BCSS: 21.51%, median survival time is of 18.42 months) and ER−/PR− subtypes (5-year OS: 13.87%, 5-year BCSS: 18.29%, median survival time is 16.84 of months). There was no significant difference in OS or BCSS between ER−/PR+ and ER−/PR− patients in all breast cancer patients or in stage IV breast cancer patients. In the subgroup analysis including bone metastasis only, one site visceral metastasis, bone metastasis and one site visceral metastasis, as shown in Figure 2, ER+/PR+ breast cancer patients still had the highest 5-year OS (Figure 2A: 52.55%, Figure 2C: 50.15%, Figure 2E: 36.69%,) and CSS rates (Figure 2B: 57.17%, Figure 2D: 57.66%, Figure 2F: 41.37%,), followed by ER+/PR− (OS: Figure 2A: 37.41%, Figure 2C: 32.29%, Figure 2E: 22.57%) (CSS: Figure 2B: 41.85%, Figure 2D: 36.98%, Figure 2F: 26.07%). The 3-year OS (Figure 2A: 15.38%, Figure 2C: 33.33%, Figure 2E: 9.09%) and CSS (Figure 2B: 15.38%, Figure 2D: 38.46%, Figure 2F: 13.64%) of ER−/PR+ patients and the 3-year OS of patients with ER−/PR− (Figure 2A: 24.17%, Figure 2C: 18.85%, Figure 2E: 10.19%,), CSS (Figure 2B: 30%, Figure 2D: 22.55%, Figure 2F: 13.21%) were not significantly different between in the first three subgroups. In the subgroup analysis of multiple visceral metastases, the 3-year OS and CSS of ER−/PR+ patients were significantly lower than those of ER−/PR− patients (Figure 2G,2H).
As shown in Table 4, multivariable analysis was performed in 5 subgroup and adjusting factors included age, race, insured status, marital status, T stage, histology, tumor classification, hormone status, surgery, positive lymph nodes, chemotherapy, radiotherapy, and metastatic mode. All of them were included and adjusted in every subgroup (metastatic mode was included only in all HER-2 negative breast cancer patients), compared with ER+/PR+ patients, single hormone positivity (ER+/PR−) were high-risk factor for CSS in all of the following groups: (I) all HER-2 negative breast cancer patients; (II) breast cancer patients without distant metastasis; (III) breast cancer patients with distant metastasis; (IV) breast cancer patients with only one bone metastasis or visceral metastasis and (V) patients with multiple visceral metastases. However, comparing with TNBC, ER−/PR+ had no significant or worse influence (multi-visceral metastasis subgroup) on CSS.
Table 4
| ER−/PR+ (vs. TNBC) | ER+/PR− (vs. ER+/PR+) | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | ||
| All patients | 0.98 | 0.84–1.14 | 0.756 | 1.97 | 1.88–2.08 | <0.001* | |
| I-III stage | 0.97 | 0.85–1.11 | 0.630 | 2.10 | 1.97–2.23 | <0.001* | |
| IV stage | 0.73 | 0.43–1.25 | 0.252 | 1.67 | 1.54–1.82 | <0.001* | |
| One site metastasis | |||||||
| Bone metastasis | 1.35 | 0.74–2.48 | 0.333 | 1.60 | 1.41–1.81 | <0.001* | |
| Visceral metastasis | 0.80 | 0.58–1.09 | 0.154 | 1.81 | 1.59–2.06 | <0.001* | |
| Multiple visceral metastatic | 2.22 | 1.37–3.59 | 0.001 | 1.69 | 1.34–2.14 | <0.001* | |
The multivariate analysis was adjusted for age, race recode, insurance recode, marital status, T stage, histology, grade, hormone status, surgery, positive lymph nodes, chemotherapy, radiation, metastasis pattern. *, significant P values (P<0.05). Visceral metastasis includes brain metastasis, liver metastasis or lung metastasis. ER, estrogen receptor; PR, progesterone receptor; IDC, intraductal carcinoma; CSS, cancer specific survival; TNBC, triple-negative breast cancer.
As shown in Table 5, the multivariable Cox analysis were performed to explore significant factor beneficial for ER+/PR− and ER−/PR+ patients. After adjusting for age, race, insured status, marital status, T stage, histology, tumor classification, surgery, positive lymph nodes, chemotherapy, radiotherapy, and metastasis mode, in ER+/PR− patients, old age, black race, a poor social support status (unmarried, incomplete social insurance), a high tumor grade, a large tumor, lymph node metastases, distant metastases and no radiation therapy or an unknown status were high-risk factors affecting CSS. In contrast, surgical interventions were protective factors affecting tumor-specific survival. For ER−/PR+ patients, age, an uninsured status, a higher tumor grade, a large primary tumor, lymph node metastases, distant metastases, no chemotherapy, or an unknown status were found to be high-risk factors associated with CSS, and surgical interventions were identified as protective factors affecting tumor-specific survival. Race, marital status, histology, and radiotherapy choices did not show an independent influence on CSS.
Table 5
| ER+/PR− | ER−/PR+ | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | ||
| Age at diagnosis (vs. ≤40) | |||||||
| 41–55 | 1.28 | 1.06–1.55 | 0.011 | 1.13 | 0.74–1.70 | 0.575 | |
| 55–70 | 1.21 | 1.01–1.46 | 0.043 | 1.21 | 0.79–1.86 | 0.380 | |
| 71–85 | 1.91 | 1.56–2.34 | <0.001 | 2.16 | 1.35–3.46 | 0.001 | |
| >85 | 3.39 | 2.65–4.33 | <0.001 | 2.16 | 1.02–4.57 | 0.045 | |
| Race recode (vs. White) | |||||||
| Black | 1.26 | 1.13–1.40 | <0.001 | 0.95 | 0.72–1.27 | 0.747 | |
| Marital status (vs. married) | |||||||
| Unmarried | 1.17 | 1.07–1.29 | 0.001 | 1.09 | 0.84–1.42 | 0.509 | |
| Insurance recode (vs. insured) | |||||||
| Any medicare | 1.19 | 1.06–1.33 | 0.003 | 1.21 | 0.90–1.64 | 0.209 | |
| Uninsured | 1.34 | 1.06–1.70 | 0.013 | 2.11 | 1.04–4.25 | 0.038 | |
| Histology (vs. IDC) | |||||||
| LC | 0.88 | 0.77–1.02 | 0.082 | 1.34 | 0.53–3.35 | 0.534 | |
| IDC + LC | 0.85 | 0.68–1.05 | 0.135 | 1.44 | 0.69–3.00 | 0.333 | |
| Grade (vs. I-II) | |||||||
| III-IV | 1.92 | 1.74–2.12 | <0.001 | 2.36 | 1.52–3.66 | <0.001 | |
| AJCC T stage (vs. ≤T1) | |||||||
| T2 | 2.12 | 1.86–2.42 | <0.001 | 1.36 | 0.97–1.90 | 0.075 | |
| T3 | 2.89 | 2.46–3.40 | <0.001 | 2.44 | 1.57–3.78 | <0.001 | |
| T4 | 3.48 | 2.96–4.10 | <0.001 | 3.24 | 2.13–4.92 | <0.001 | |
| Surgery (vs. no surgery) | |||||||
| Conserving | 0.35 | 0.29–0.42 | <0.001 | 0.25 | 0.16–0.39 | <0.001 | |
| Mastectomy | 0.47 | 0.39–0.56 | <0.001 | 0.31 | 0.19–0.50 | <0.001 | |
| Radical | 0.54 | 0.45–0.64 | <0.001 | 0.45 | 0.28–0.70 | <0.001 | |
| Positive nodes (vs. 0) | |||||||
| 1–3 | 2.31 | 2.00–2.67 | <0.001 | 2.04 | 1.42–2.94 | <0.001 | |
| 4–9 | 4.07 | 3.43–4.83 | <0.001 | 3.67 | 2.30–5.86 | <0.001 | |
| ≥10 | 4.98 | 4.12–6.02 | <0.001 | 4.33 | 2.70–6.93 | <0.001 | |
| Radiation recodes (vs. yes) | |||||||
| No/unknown | 1.17 | 1.07–1.28 | 0.001 | 1.11 | 0.86–1.45 | 0.424 | |
| Chemotherapy recodes (vs. yes) | |||||||
| No/unknown | 0.98 | 0.89–1.09 | 0.732 | 1.65 | 1.23–2.23 | <0.001 | |
| Metastasis site (vs. M0) | |||||||
| Only bone | 3.61 | 3.12–4.18 | <0.001 | 4.99 | 2.61–9.51 | <0.001 | |
| Only visceral | 4.33 | 3.54–5.29 | <0.001 | 3.58 | 2.24–5.72 | <0.001 | |
| Only bone + only visceral | 5.58 | 4.69–6.64 | <0.001 | 6.83 | 3.90–11.96 | <0.001 | |
| Multiple visceral metastasis | 7.95 | 6.38–9.90 | <0.001 | 46.12 | 25.10–84.72 | <0.001 | |
ER, estrogen receptor; PR, progesterone receptor; IDC, intraductal carcinoma; CSS, cancer specific survival; TNBC, triple-negative breast cancer.
Discussion
With the development of immunohistochemistry technology, clinical retrospective studies and experiments cannot deny the existence of the subtype of progesterone receptor positive ER−/PR+ subtype (16). In our study, the single progestin-positive subtype accounted for 0.89% in HER-2 negative patients and the incidence of such rare subtype was reported 1–4% in all breast cancer patients (17). Early studies reported that single-hormone receptor-positive (including ER+/PR− and ER−/PR+) breast malignancies have more aggressive biological characteristics than ER+/PR+ tumors and prognostic differences (18,19). In particular, patients with ER−/PR+ breast cancer have a larger tumor mass (19), a higher histological grade, and higher HER-2 expression (20), but stronger evidence of metastatic patterns in advanced breast cancer is still rare. The difference in metastatic patterns also reflects the aggressive characteristic of patients with single hormone receptor-positive breast cancer. such as the single PR negativity is also an independent risk factor for visceral metastasis. And this conclusion is consistent with previous studies (11,21). Meanwhile, we also ER−/PR+ patients and TNBC patients had a similar metastasis pattern, that is, the two groups of advanced patients tended to develop visceral metastasis, but not bone metastasis. This observation reinforces research evidence from the Chinese Academy of Sciences (19).
The role of estrogen and progesterone in bone metabolism and bone metastasis has been reported in previous studies (22). Estrogen is an important regulator of bone, and ER influence tumor susceptibility. Tumor cells with hormone receptor-positive homing of the bone microenvironment through the RANK-RANKL and CXCL12-CXCR4 signaling pathways (23) adhere to and survive the bone matrix as “soil”, and tumor dormancy or growth depends on the body's estrogen status (12).
At present, the results from 6-year follow-up showed that the downward trend of OS and CSS in metastatic breast cancer patients was relatively obvious. With the loss of ER and PR, and the increase in visceral metastasis, the prognosis of stage IV breast cancer patients tends to worsen. However, our study was unable to observe the survival difference between ER−/PR+ and TNBC patients, which implied that the single PR positivity breast cancer is similar with TNBC in biological characteristics. This is consistent with the previous study on the prognosis of ER+/PR− breast cancer patients. The 5-year OS, BCSS and recurrence-free survival (RFS) of ER+/PR− breast cancer patients were all between those of Lumina A and TNBC patients (18). Bernoux et al. analyzed all ER−/PR+ and TNBC patients and found that the former group had better disease-free survival (24). However, Rakha et al. did not find an RFS advantage in (25) but did find that its OS was significantly higher in ER−/PR+ patients than in TNBC patients (10), which were enhanced by the evidence from Professor Ren. This difference in survival may be because of the HER-2 on prognosis. Although the SEER lacks the record of related factors such as Ki67 and p53, the absence of HER-2 may affect the expression of biomarkers of breast cancer proliferation. Under the condition of negative HER-2, ER−/PR+ tumors showed higher levels of not only Ki67 expression but also of p53 and EGFR expression (5). Moreover, some studies have found that in patient subgroups receiving endocrine therapy, ER−/PR+ patients could obtain survival benefits. Dr. Ying Fan found that under HER-2 negative conditions, regardless of the 5-year OS or BCSS, there was no significant difference between ER−/PR+ and TNBC patients, but the survival of ER−/PR+ patients receiving endocrine therapy was significantly higher than that in TNBC patients. The survival of patients not receiving endocrine therapy was even worse than that of TNBC patients (19). This result confirms the role of the PR receptor as an independent predictor of the response to endocrine therapy and ER−/PR+ is a distinct subtype.
Single positive hormone receptor was a risk factor for CSS in the multivariate Cox analysis in different groups (all breast cancer groups, stage I-III patients, M1 patients with only bone metastasis, patients with only visceral metastasis, patients with only bone and visceral metastases, and patients with multiple visceral metastases). In M1 patients, the survival advantage associated with receptor positivity may be attributed to a high proportion of bone metastasis. However, even if metastasis occurred at the same site, negative hormone receptor would also lead to a poor outcome. Similar results have been obtained from other studies on the effect of different molecular subtypes on the outcome of lung metastasis (26) and brain metastasis (27). Our study further confirmed the prognostic value of ER and PR in CSS considering the HER-2 status.
We also analyzed the high-risk factors that may lead to cancer-specific death in breast cancer patients with single hormone receptor positivity (ER+/PR− and ER−/PR+). It is worth mentioning that radiotherapy was an independent protective factor in ER+/PR− patients, and chemotherapy was found to be a protective factor in the prognosis of ER−PR+ patients. Previous reports have also found the positive significance of chemotherapy in ER−/PR+ patients in single factor analysis (19). This indicates that ER−/PR+ patients may benefit not only from endocrine therapy but also from chemotherapy. Clinical studies have also shown that CMF is more effective than CA (E)F in the treatment of ER−/PR+ breast cancer (28). Therefore, in the clinic, chemotherapy combined with endocrine therapy may be a better choice for this type of patients.
In conclusion, the number of ER−/PR+ patients is small, and little is known about the clinical characteristics and prognosis of this subgroup, especially in stage IV patients. Our strength of study includes that we analyzed and compared differences in the sites of metastasis and prognosis of patients between ER−/PR− and those with double positivity and negativity. The clinical doctors should pay attention to high rate of metastatic breast cancer from single hormone receptor-positive breast cancer. Meanwhile, comparing with TNBC, the OS and CSS of ER−/PR+ had no significant even worse prognosis. Furthermore, surgery and radiotherapy may improve the CSS of ER+/PR− patients and clinicians should consider the combination of chemotherapy and endocrine therapy for ER−/PR+ patients. The current guidelines don’t include the ER−/PR+ subtype and it was considered a technical error in PR measurement. In clinical work, it is difficult to ensure whether the single PR positivity had independent predictive and prognosis value of and therapy methods such as whether the hormone therapy should be provided. Although our results shown no significant differences even worse prognosis in survival between ER−/PR+ and TNBC. The study from the Chinese Academy of Medical Sciences and Peking Union Medical College shown adjuvant endocrine therapy still benefit this group of patients. (In ER−/PR+/HER-2-group, cases with adjuvant endocrine therapy had significantly better RFS) (19). The single PR status should be accepted and chemotherapy and adjuvant endocrine therapy should be considered.
There are some limitations and shortcomings to this study. First, the SEER database has no records of endocrine therapy and targeted therapy, so to exclude the impact of positive HER-2 and targeted therapy on prognosis, we excluded HER-2-positive patients, but inevitably lost a portion of the study subjects and could not avoid the lack of information on endocrine therapy. Secondly, the SEER database began to record the sites of metastasis in stage IV breast cancer patients after 2010, so a longer follow-up time is needed to verify the current research results. More evidence of endocrine therapy for single hormone receptor-positive breast cancer is needed to confirm the differences between the prognosis of such patients and those with TNBC.
Acknowledgments
This study used the linked SEER Regs Custom database. SEER is supported by the Surveillance Research Program (SRP) in NCI’s Division of Cancer Control and Population Sciences (DCCPS). This work was partially supported by the General surgery laboratory, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, China.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-21-677/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-21-677/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-21-677/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Perou CM, Sørlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature 2000;406:747-52. [Crossref] [PubMed]
- Sørlie T. Molecular portraits of breast cancer: tumour subtypes as distinct disease entities. Eur J Cancer 2004;40:2667-75. [Crossref] [PubMed]
- Cheang MC, Chia SK, Voduc D, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 2009;101:736-50. [Crossref] [PubMed]
- Arpino G, Weiss H, Lee AV, et al. Estrogen receptor-positive, progesterone receptor-negative breast cancer: association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst 2005;97:1254-61. [Crossref] [PubMed]
- Bae SY, Kim S, Lee JH, et al. Poor prognosis of single hormone receptor- positive breast cancer: similar outcome as triple-negative breast cancer. BMC Cancer 2015;15:138. [Crossref] [PubMed]
- Goldhirsch A, Winer EP, Coates AS, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol 2013;24:2206-23. [Crossref] [PubMed]
- Curigliano G, Burstein HJ, Winer EP, et al. De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017. Ann Oncol 2017;28:1700-12. [Crossref] [PubMed]
- Yip CH, Rhodes A. Estrogen and progesterone receptors in breast cancer. Future Oncol 2014;10:2293-301. [Crossref] [PubMed]
- Cui X, Schiff R, Arpino G, et al. Biology of progesterone receptor loss in breast cancer and its implications for endocrine therapy. J Clin Oncol 2005;23:7721-35. [Crossref] [PubMed]
- Li Y, Yang D, Yin X, et al. Clinicopathological Characteristics and Breast Cancer-Specific Survival of Patients With Single Hormone Receptor-Positive Breast Cancer. JAMA Netw Open 2020;3:e1918160. [Crossref] [PubMed]
- Arciero CA, Guo Y, Jiang R, et al. ER+/HER2+ Breast Cancer Has Different Metastatic Patterns and Better Survival Than ER−/HER2+ Breast Cancer. Clin Breast Cancer 2019;19:236-45. [Crossref] [PubMed]
- Hofbauer LC, Rachner TD, Coleman RE, et al. Endocrine aspects of bone metastases. Lancet Diabetes Endocrinol 2014;2:500-12. [Crossref] [PubMed]
- Li Y, Su P, Wang Y, et al. Impact of histotypes on preferential organ‐specific metastasis in triple‐negative breast cancer. Cancer Med 2020;9:872-81. [Crossref] [PubMed]
- Yao Y, Chu Y, Xu B, et al. Risk factors for distant metastasis of patients with primary triple-negative breast cancer. Biosci Rep 2019;39:BSR20190288. [Crossref] [PubMed]
- Van Mechelen M, Van Herck A, Punie K, et al. Behavior of metastatic breast cancer according to subtype. Breast Cancer Res Treat 2020;181:115-25. [Crossref] [PubMed]
- Kunc M, Biernat W, Senkus-Konefka E. Estrogen receptor-negative progesterone receptor-positive breast cancer - "Nobody's land" or just an artifact? Cancer Treat Rev 2018;67:78-87. [Crossref] [PubMed]
- Lv M, Mao Y, Song Y, et al. Clinical Features and Survival of Single Hormone Receptor-Positive Breast Cancer: A Population-Based Study of 531,605 Patients. Clin Breast Cancer 2020;20:e589-99. [Crossref] [PubMed]
- Wei JL, Zhang JX, Fu DY. Characterization and prognosis of estrogen receptor-positive/progesterone receptor-negative male breast cancer: a population-based study. World J Surg Oncol 2018;16:236. [Crossref] [PubMed]
- Fan Y, Ding X, Xu B, et al. Prognostic Significance of Single Progesterone Receptor Positivity. Medicine (Baltimore) 2015;94:e2066. [Crossref] [PubMed]
- Chan M, Chang MC, González R, et al. Outcomes of Estrogen Receptor Negative and Progesterone Receptor Positive Breast Cancer. PLoS One 2015;10:e0132449. [Crossref] [PubMed]
- Xiao W, Zheng S, Yang A, et al. Breast cancer subtypes and the risk of distant metastasis at initial diagnosis: a population-based study. Cancer Manag Res 2018;10:5329-38. [Crossref] [PubMed]
- Croucher PI, McDonald MM, Martin TJ. Bone metastasis: the importance of the neighbourhood. Nat Rev Cancer 2016;16:373-86. [Crossref] [PubMed]
- Roodman GD. Mechanisms of bone metastasis. N Engl J Med 2004;350:1655-64. [Crossref] [PubMed]
- Bernoux A, de Cremoux P, Lainé-Bidron C, et al. Estrogen receptor negative and progesterone receptor positive primary breast cancer: pathological characteristics and clinical outcome. Institut Curie Breast Cancer Study Group. Breast Cancer Res Treat 1998;49:219-25. [Crossref] [PubMed]
- Rakha EA, El-Sayed ME, Green AR, et al. Biologic and clinical characteristics of breast cancer with single hormone receptor positive phenotype. J Clin Oncol 2007;25:4772-8. [Crossref] [PubMed]
- Xiao W, Zheng S, Liu P, et al. Risk factors and survival outcomes in patients with breast cancer and lung metastasis: a population-based study. Cancer Med 2018;7:922-30. [Crossref] [PubMed]
- Kim YJ, Kim JS, Kim IA. Molecular subtype predicts incidence and prognosis of brain metastasis from breast cancer in SEER database. J Cancer Res Clin Oncol 2018;144:1803-16. [Crossref] [PubMed]
- Yu KD, Di GH, Wu J, et al. Breast cancer patients with estrogen receptor-negative/progesterone receptor-positive tumors: being younger and getting less benefit from adjuvant tamoxifen treatment. J Cancer Res Clin Oncol 2008;134:1347-54. [Crossref] [PubMed]



