Surgical decision making in conservative mastectomies
Background
It is well known that the choice between breast conservation and mastectomy has become rather complex over the years, especially once the equivalence in terms of oncological control between breast conservation followed by radiotherapy and mastectomy has been solidly demonstrated (1-6). Thanks to great advancements in breast reconstruction, nowadays we can offer preservation or demolition of the gland obtaining similar results also in terms of quality of life (7). These results were obtained thanks to new kinds of mastectomies that allowed the preservation of the breast envelope possibly including the nipple areola complex (NAC). We named these techniques “conservative mastectomies” (8-10) and we are going to propose indications and techniques to perform envelope preservation safely. Notably we tried to embed elements in our decision-making derived from validated models, such as a quantitative assessment of breast volume and ptosis, an algorithm able to anticipate the risk of complications after breast reconstruction and finally a very advanced calculator of risk of positive margins with breast conservation (11-14).
We candidate all patients with early stage breast cancer (ESBC) to implant based reconstructions irrespective of breast size and shape. We inform all patients in this subset regarding the stability of results with this technique (15). We use autologous flaps only in delayed reconstructions after radiation treatment for locally advance breast cancer, or immediately after salvage mastectomies for recurrence after breast conservation. Autologous flaps can be a good option also in young women diagnosed affected by primary localized extensive disease with a very good prognosis. In view of an expected long-term survival, these women may obtain the maximum benefit from sophisticated techniques based on microsurgery with muscle preservation that we normally recommend.
Clinical elements to be investigated before deciding to candidate patients to conservative mastectomies
Although some oncoplastic techniques have broadened the indication to breast conservation, clinical conditions exist in which the total removal of the mammary gland is still mandatory. This happens in patients affected by ESBC with extensive ductal carcinoma in situ (DCIS) with or without an infiltrating component, multi-centric disease and of course in locally advanced breast cancer (LABC) requiring multimodality treatment. Some more patients with ESBC may lie in a borderline condition in which it is more difficult to decide between mastectomy and breast conservation.
The decision to perform a mastectomy in patients affected by localized cancer is based on a combination of clinical, histological and biological characteristics. We added to this the personal preferences of the patient regarding final appearance, breast shape and volume in order to perform maximum reshape or reduce surgical aggressiveness.
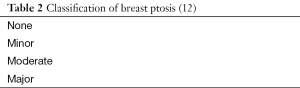
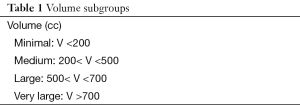
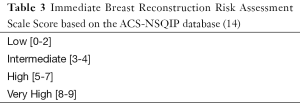
These are normally acquired during the first consultation after a referral for a suspicious lump or infra-clinical disease. The morphological characteristic (breast volume and ptosis) of the patients are acquired either in a visual or in a quantitative way. More specifically, we study the breast volume using a model described by Longo et al. (11) and we create five categories as described in (Table 1). We use a further model to describe ptosis in a reliable and reproducible way (12) with the definition of four subcategories (Table 2). During clinical examination and assessment of imaging we also evaluate the location of the disease in the breast segmented in four areas radial areas and a central one, clearly certain cases may include double or multiple locations (multifocal or multicentric carcinoma). Before surgical treatment, all our patients undergo a core biopsy in order to reach a pre-operative diagnosis. Combined with other information summarized in Table 3, it can be introduced into a validated model named breast conservation (13), in order to get information regarding the risk of positive margins.
Full table
Full table
Investigation of patients’ preferences
We refuse a paternalistic approach to clinical decisions and therefore we tend to share this process with patients (16). This is not always easy, as some patients do not fully understand complex medical languages (17). For this reason, we enhanced the information process using booklets, video of results or surgical operation, videos and photographs of previous patients regarding each possible surgical technique to be employed. Normally this was done after the second consultation once a diagnosis is already known and a cluster of possible surgical options has been already offered. We ask patients that can be treated by either conservation or demolition to express their preference regarding the surgical technique according to three possible sub-categories:
- Mastectomy;
- Minimal aggressiveness;
- Maximum reshape.
Those who are inevitably candidate to mastectomy can indicate their wish between the last two subcategories (minimal aggressiveness-maximum reshape).
The three subcategories of patients’ wishes are created to include all possible surgical techniques that a patient may require.
Regarding the subgroup indicating “mastectomy” we include in this all women that can be candidate either to breast preservation or mastectomy who after a thorough information of possible cosmetic results, risks and benefits of radiotherapy, limitations and impact of breast reconstruction still prefer to undergo breast removal. Patients whose single option was mastectomy cannot be included in this category.
The second subgroup named “minimal aggressiveness” includes women who prefer to receive simple operations with minimal residual deformities without contralateral adjustments if breast conservation is indicated. For patients invariably candidate to mastectomy this subgroup includes women who wish to receive skin or nipple sparing mastectomies with the simplest technique without contralateral reshape possibly in one stage.
Finally, the third subgroup denominated “maximum reshape” includes patients who require bilateral operations to reach the best cosmetic results with minimal asymmetries. If they can be candidated only to mastectomy this will mean that they wish to have contralateral adjustment concurrently with breast reconstruction.
Indication to conservative mastectomies
We offer conservative mastectomies in all patients affected by unifocal breast cancer located in the inner quadrants, or in the central quadrant of a small to medium size breast. In this setting of patient, we tend not to perform breast conservation, unless specifically requested, as this could yield poor cosmetic results. We also encourage the decision to remove the breast in all patients with small gland specifically requiring a mastectomy. This may reduce the need for second operations if positive margins occur, and is especially recommended in case of a demonstrated high risk of leaving residual disease. We also offer a mastectomy to patients with small to medium size breast with moderate or no ptosis affected by unifocal breast cancer located in the lower outer quadrant if specifically requested by the patient after proper consultation.
Multi-centric breast cancers or multifocal breast cancers that are not suitable for breast preservation are always candidate to mastectomy.
We indicate conservative mastectomies in selected cases of LABCs who had very good response to pre-operative systemic treatment with significant reduction of the breast mass and resolution of edema (18-20).
Nipple or skin preservation?
We perform nipple preservation in all cases where the absence of disease is demonstrated by multiple intra-operative biopsies of the retro-areolar ducts. However, nipple preservation is more a technical challenge rather than an oncologic one (18,21-24). The impact on local control of nipple preservation has been demonstrated by several studies, none of which has shown an exceeding risk of local recurrence. However, total preservation of the envelope in large and ptotic breast can create long and ischemic flaps with possible necrotic complications (25).
Skin preservation in ESBC (no infiltration of the skin by definition) can be performed in a large majority of the cases. We discourage preservation of the mammary cutaneous mantel in patients with a high risk score of complications (14).
Surgical techniques in patients with small and medium sized breast and minimal/no ptosis
Patients with small/medium breast and minimal to moderate ptosis (12,13) can safely preserve the breast envelope. The nipple will be removed only in case of presence of neoplastic cells in the major ducts. The reconstruction will be performed according to patients’ preferences either in one stage with permanent implants (possibly with acellular dermal matrices) or in two stages. Depending on patients wishes (“maximum reshape”) a contralateral adjustment can be performed in a single stage or at the second stage with contralateral breast augmentation with or without mastopexy. The mastectomy should be performed through an S-italic incision starting 2-3 cm laterally of the nipple towards the upper-outer quadrants (photo of incision plan). The contralateral adjustment will usually require an augmentation (with implants placed in a dual plane/sub-pectoral/sub glandular position according to the characteristics of the skin, upper pole fullness and of course patients preferences). In selected cases with minor to moderate ptosis, a contralateral mastopexy with authoprotesis could be offered with very natural results. Some patients wishing minimal aggressiveness may require a unilateral procedure possibly in one stage that can be performed once the patient has been clearly informed regarding possible asymmetric results.
Patients with large breast with or without ptosis
These patients may undergo a novel technique described by Nava et al. (8,10,26) named skin reducing mastectomy. This is a modification of type IV skin sparing mastectomies as described by Carlson et al. (27) that uses a de-epithelialized dermal adipose flap sutured to the pectoralis major and the fascia of the serratus anterior as a component of a compound pouch in which a permanent implant could be easily allocated. The final inverted T scars will look symmetric to that of a breast reduction or mastopexy that can be performed on the contralateral side. This operation offers a good chance to have breast reconstruction in one stage with permanent implants in patients in which skin preservation is a non-sense and therefore there is no point to undergo expansion and a second stage operation. Sometimes, as reported in some studies (8) the presence of extra-projection implants may create tension and ischemia of the mastectomy flaps with a little bit higher complication rate. For this reason in selected patients at high risk of complication, we advise to undergo a two-stage skin-reducing mastectomy in order to minimize the tension on critical residual mastectomy flaps. The contralateral adjustment will be performed in the second surgical stage of the operation.
Nipple sparing skin reducing mastectomies are indicated in patients with large breast, but still moderate ptosis. The nipple preservation can be performed in cases in which the nipple to sternal notch distance does not exceed 2-3 cm. In these cases, the NAC can be held on very thin superior dermal flap, if a very radical ablation of the major ducts is performed.
Patients with unifocal breast cancer suitable for breast conservation requiring a mastectomy are discouraged to undergo this operation and diverted to easier techniques of preservation. Depending on tumour size and location, this may include bilateral therapeutic mammoplasties that may generate very good final cosmetic results.
Conclusions
In this paper, we provide some clinical advice to drive the decision process in performing conservative mastectomies. Several factors should be taken into consideration to indicate these techniques (Table 4). First of all, we need to identify patients who need a mastectomy for the extension of the disease. These women cannot be offered breast conservation at any time. In this case we suggest assessing patients’ anthropometric characteristics (breast volume—ptosis), and personal preferences regarding the extension of surgical treatment (Figure 1). Small, medium size, without ptosis or with moderate ptosis can be better served by standard nipple sparing mastectomy if oncological requirements are fulfilled. Large and ptotic breast can be removed and reconstructed in one stage with a proper reshape of the breast envelope. Some patients in this subgroup are at high risk of complication and may be better served by a two-stage procedure with tissue expansion. Mastectomies cannot replace breast conservation and should be discouraged whenever breast-conserving surgery can be performed with good results. However, in some selected cases, especially in patients with small breast, conservative mastectomies with contralateral reshape can yield favourable results.
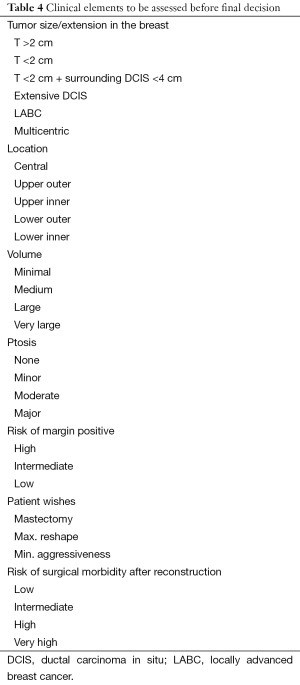
Full table

Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233-41. [PubMed]
- Blichert-Toft M, Rose C, Andersen JA, et al. Danish randomized trial comparing breast conservation therapy with mastectomy: six years of life-table analysis. Danish Breast Cancer Cooperative Group. J Natl Cancer Inst Monogr 1992.19-25. [PubMed]
- van Dongen JA, Bartelink H, Fentiman IS, et al. Randomized clinical trial to assess the value of breast-conserving therapy in stage I and II breast cancer, EORTC 10801 trial. J Natl Cancer Inst Monogr 1992.15-8. [PubMed]
- Sarrazin D, Lê MG, Arriagada R, et al. Ten-year results of a randomized trial comparing a conservative treatment to mastectomy in early breast cancer. Radiother Oncol 1989;14:177-84. [PubMed]
- Jacobson JA, Danforth DN, Cowan KH, et al. Ten-year results of a comparison of conservation with mastectomy in the treatment of stage I and II breast cancer. N Engl J Med 1995;332:907-11. [PubMed]
- Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227-32. [PubMed]
- Heneghan HM, Prichard RS, Lyons R, et al. Quality of life after immediate breast reconstruction and skin-sparing mastectomy - a comparison with patients undergoing breast conserving surgery. Eur J Surg Oncol 2011;37:937-43. [PubMed]
- Nava MB, Cortinovis U, Ottolenghi J, et al. Skin-reducing mastectomy. Plast Reconstr Surg 2006;118:603-10; discussion 611-3. [PubMed]
- della Rovere GQ, Nava M, Bonomi R, et al. Skin-reducing mastectomy with breast reconstruction and sub-pectoral implants. J Plast Reconstr Aesthet Surg 2008;61:1303-8. [PubMed]
- Nava MB, Ottolenghi J, Pennati A, et al. Skin/nipple sparing mastectomies and implant-based breast reconstruction in patients with large and ptotic breast: oncological and reconstructive results. Breast 2012;21:267-71. [PubMed]
- Longo B, Farcomeni A, Ferri G, et al. The BREAST-V: a unifying predictive formula for volume assessment in small, medium, and large breasts. Plast Reconstr Surg 2013;132:1e-7e. [PubMed]
- Kim MS, Reece GP, Beahm EK, et al. Objective assessment of aesthetic outcomes of breast cancer treatment: measuring ptosis from clinical photographs. Comput Biol Med 2007;37:49-59. [PubMed]
- Pleijhuis RG, Kwast AB, Jansen L, et al. A validated web-based nomogram for predicting positive surgical margins following breast-conserving surgery as a preoperative tool for clinical decision-making. Breast 2013;22:773-9. [PubMed]
- Fischer JP, Wes AM, Tuggle CT, et al. Risk analysis and stratification of surgical morbidity after immediate breast reconstruction. J Am Coll Surg 2013;217:780-7. [PubMed]
- Atisha DM, Rushing CN, Samsa GP, et al. A national snapshot of satisfaction with breast cancer procedures. Ann Surg Oncol 2015;22:361-9. [PubMed]
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008;27:759-69. [PubMed]
- Krumholz HM. Informed consent to promote patient-centered care. JAMA 2010;303:1190-1. [PubMed]
- Burdge EC, Yuen J, Hardee M, et al. Nipple skin-sparing mastectomy is feasible for advanced disease. Ann Surg Oncol 2013;20:3294-302. [PubMed]
- Fortunato L, Loreti A, Andrich R, et al. When mastectomy is needed: is the nipple-sparing procedure a new standard with very few contraindications? J Surg Oncol 2013;108:207-12. [PubMed]
- Prabhu R, Godette K, Carlson G, et al. The impact of skin-sparing mastectomy with immediate reconstruction in patients with Stage III breast cancer treated with neoadjuvant chemotherapy and postmastectomy radiation. Int J Radiat Oncol Biol Phys 2012;82:e587-93. [PubMed]
- Petit JY, Veronesi U, Rey P, et al. Nipple-sparing mastectomy: risk of nipple-areolar recurrences in a series of 579 cases. Breast Cancer Res Treat 2009;114:97-101. [PubMed]
- Rusby JE, Brachtel EF, Taghian A, et al. George Peters Award. Microscopic anatomy within the nipple: implications for nipple-sparing mastectomy. Am J Surg 2007;194:433-7. [PubMed]
- Gerber B, Krause A, Reimer T, et al. Skin-sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction is an oncologically safe procedure. Ann Surg 2003;238:120-7. [PubMed]
- Caruso F, Ferrara M, Castiglione G, et al. Nipple sparing subcutaneous mastectomy: sixty-six months follow-up. Eur J Surg Oncol 2006;32:937-40. [PubMed]
- Chirappapha P, Petit JY, Rietjens M, et al. Nipple sparing mastectomy: does breast morphological factor related to necrotic complications? Plast Reconstr Surg Glob Open 2014;2:e99. [PubMed]
- della Rovere GQ, Nava M, Bonomi R, et al. Skin-reducing mastectomy with breast reconstruction and sub-pectoral implants. J Plast Reconstr Aesthet Surg 2008;61:1303-8. [PubMed]
- Losken A, Carlson GW, Bostwick J 3rd, et al. Trends in unilateral breast reconstruction and management of the contralateral breast: the Emory experience. Plast Reconstr Surg 2002;110:89-97. [PubMed]