
Resecting a solitary cervical vagal nerve neurofibroma via endoscopic surgery: a case report
Introduction
Cervical vagal nerve neurofibroma (VNN) consists of Schwann cells and fibroblasts and is a type of peripheral nerve sheath tumor that correlates with neurofibromatosis type 1 (1). However, solitary cervical VNN has rarely been observed in recent years, and only a few cases have been reported (2,3). As a type of benign neurogenic tumor, the main treatment strategy for VNN is complete surgical resection, which enables accurate definite histologic diagnosis and treatment. However, patients no longer only value the survival and recovery of disease; they now greatly value postoperative cosmetic outcomes, especially in head and neck surgery. Therefore, as one of the novel surgical methods, minimally-invasive neck surgery with multiple approaches including, but not limited to, bilateral axilla-breast approach (BABA) and transoral approach, have been demonstrated to be safe, efficacious, and perfectly meet the requirements of better cosmetic outcomes compared with traditional open approaches (TOA) (4,5). To the best of our knowledge, this was the first case of solitary cervical VNN resection via BABA in the Chinese population, providing a new horizon for the therapeutic indications of endoscopic surgery for neck tumors.
We present the following case following the CARE reporting checklist (available at http://dx.doi.org/10.21037/gs-20-706).
Case presentation
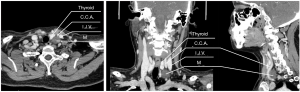
A 49-year-old Chinese female was admitted to the Department of Breast and Thyroid Surgery of the Second Affiliated Hospital of Chongqing Medical University with an unexpected physical examination discovery of a left neck mass 15 days before admission. Before this admission, the patient did not complain of any discomfort or difficulty in cervical function or respiration. Color Doppler ultrasound (CDU) imaging revealed a well-defined round mixed hypoechoic and hyperechoic echogenicity nodule (2.2 cm × 1.5 cm × 2.4 cm), without blood flow signal inside, located posterior to the lower pole of the left thyroid lobe and internal jugular vein (IJV) (Figure 1). The three-dimensional (3D)-computed tomography (CT) scan reconstruction demonstrated a regular shape, clear boundary, and low-density nodule (19 mm × 16 mm) near the left common carotid artery (CCA) and IJV. In the sagittal position, forward displacement of the CCA caused by the mass was observed (Figure 2). Medical history and essential laboratory examinations were performed, revealing that the patient had maintained a good general condition without any history of chronic illness, smoking, or drinking habits, and there was no family history of note. This patient was very health-conscious and concerned about her physical appearance. After comprehensive department internal discussion and consideration of the patient’s preferences, on the third day of hospitalization, the patient underwent mass dissection by endoscopic surgery via BABA (Figure 3A).

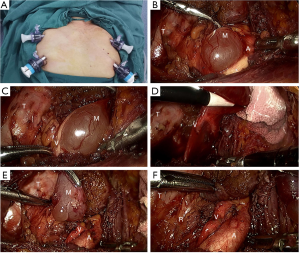
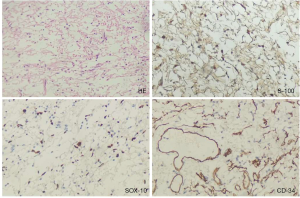
In line with the surgical procedures of endoscopic thyroidectomy (6), the subcutaneous connective tissues and muscles on the ventral surface of the neck were gently retracted with the help of an ultrasonic scalpel (US) and electrocoagulation hook (EH). After establishing the operative field by carbon dioxide insufflation, we exposed the trachea and thyroid (Video S1). The US was then used to dissect the left middle thyroid vein and separate the lateral thyroid space. After exposing the carotid sheath, the left CCAs were clearly separated (Video S1). The mass was found located dorsally from the CCA. Also, the vessels were freed from the lesion’s base and then from the superior edge of the lesion. The fascial attachments covered on the tumor surface were separated, and the tumor capsule was identified. It was a cystic mass with a soft texture and a complete and smooth surface (Figure 3B); the vagus nerve ran along the surface of the mass (Figure 3C). With subtle manipulation, the mass was completely dissected, the cut-section had a gelatinous appearance with minute cystic areas (Figure 3D,E), and preserving the continuity of the vagus nerve and CCA (Figure 3F). After dissection, it was sent for final histological evaluation. The pathological examination revealed long spindle tumor cells with slender nuclei under hematoxylin and eosin (HE) staining. Immunohistochemically, the tumor cells were positive for transcription factor S-100 and vimentin (Vim), partially positive for epithelial membrane antigen (EMA), diffusely positive for SRY-related HMG-box (SOX)-10, and positive for vascular marker CD34 (Figure 4). These pathological features were consistent with the diagnosis of neurofibroma. Although the left vagus nerve was confirmed to be intact and continuous by two surgeons after the lesion was detached, the patient received prophylactic neurotrophic treatment including vitamin B1 [0.1 g, intramuscular injection, once daily (qd)] and mecobalamin [0.5 mg, oral administration, 3 times daily (tid)] for three days to prevent potential mechanical or thermal damage. Fortunately, no complications, such as dyspnea, inflammation, weak voice, or hoarseness, were observed during the postoperative hospital stay. The timeline is described in Table 1.
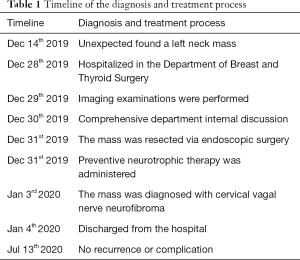
Full table
The patient was very satisfied with the minimally invasive surgery and her neck’s postoperative appearance (Figure 5). She was discharged uneventfully on postoperative day 8. At the 6-month follow-up, there were no complaints or signs of recurrence for this patient. The patient’s husband provided written informed consent according to the institutional guidelines.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was provided by the patient according to institutional guidelines for publication of this case report and any accompanying images.
Discussion
Cervical VNN, as a type of neurogenic tumor with a predominately benign lesion, originates from peripheral nerve sheath cells and is usually sequelae to neurofibromatosis type 1 (1). In contrast, solitary cervical VNNs have been infrequently reported in the past published literature (2,3). To date, the preoperative diagnosis of cervical VNN is challenging due to its chronic, asymptomatic, and insidious onset, and it is often discovered unexpectedly during physical examination. As tumor size increases, it may present as a local neck mass that further causes neck swelling and compression symptoms. However, these clinical manifestations are nonspecific.
Nonetheless, some valuable pathognomonic features may be displayed on the cross-sectional imaging in an early stage of VNN. For instance, diffusion-weighted magnetic resonance (MR) imaging (DWI) offers increased specificity (7,8) in the diagnosis of peripheral nerve sheath tumors with characteristics of increased central and decreased peripheral signal intensity on T1-weighted images (the “target sign”) and an opposite pattern of increased peripheral and decreased central signal intensity on T2-weighted images, as compared with CT scan. Moreover, as Liu et al. reported, CDU could detect low-velocity arterial flows within the mass and the explicit anatomical relationship between the mass and its peripheral vascularization (9). Moreover, the high-resolution images of CDU can help to identify the origin of tumors.
The diagnosis of VNN is mainly based on the pathological examination of postoperative tissues. Pathologically, Schwann cells are the predominant component of VNN, and have characteristics of being slender and spindle-shaped. The long spindle tumor cells are typically arranged in a palisading pattern, resembling waves of a rippling water pattern with a lightly stained cytoplasm (like “shredded carrots”) and slender nucleus, vascularly surrounded, and forming a bundle-like arrangement (Figure 4). Immunohistochemically, the present case’s tumor cells were positive for S-100 and vimentin (Vim), diffusely positive for SOX-10, and positive for vascular marker CD34. Separately, the immunostaining positivity for CD34 and vimentin suggested that the mass was of mesenchymal origin. Besides, SOX-10, as a transcription factor, is essential for the development of Schwann cells, and therefore can also be used as a marker for corresponding tumors, including neurofibroma and schwannomas (10,11).
Further, it’s believed that S-100 expression is responsible for the reconstruction and proliferation of Schwann cells in response to peripheral nerve degeneration, thus it is regarded as a specific diagnostic indicator for neurogenic tumors (12) (Figure 4). Clinically, the differential diagnosis mainly includes enlarged lymph nodes and other neurogenic tumors like schwannomas. Only tumors arising from the vagus nerve can splay the IJV and the carotid artery, and tumors arising from the carotid body will push the vascular structures to the lateral or medial position. Given microanatomy, schwannomas usually grow off one nerve fiber and splay the remaining fibers over the tumor surface, which can displace and press on the other fibers of the parent nerve; whereas neurofibromas are fusiform and arise more centrally from the perineurium of the nerve (13) (Figure 3C). Histologically, two distinct architectural components exist in the schwannomas: Antoni A areas (compact, exhibit high cellularity, and are composed of spindle cells with elongated nuclear palisading) and Antoni B areas (less cellularity, and are composed of fusiform cells in a loose matrix with microcysts) (13,14). In contrast, neurofibromas are lacking in Antoni A areas but display more uniform cellularity and wavy or “comma-shaped” nuclei.
In the current case, the reason why it was challenging to diagnose VNN at the initial preoperative examination definitely might be that the mass was located deeply behind the left CCA and near the left IJV (Figure 2), making it easily mistaken for a simple mass arising from the parathyroid or carotid artery. Besides, relatively little quality information was available from the medical record as the small tumor volume had not caused any obvious symptoms for the patient. When the surgical intervention was performed, the cystic mass was observed to attach to the vagus nerve, and the features of the mass, including soft texture, complete and smooth surface, and gelatinous contents, were consistent with that reported in the previous literature (1,9,13), which partially contributed to the diagnosis of VNN during the operation. The postoperative pathological examination finally determined that the tumor was a neurofibroma that arose from the vagus nerve.
Surgical intervention is currently the major treatment approach for this kind of benign cervical neurogenic tumor (1,9). However, the difficulty of TOA was increased due to the lesion being attached to the nerves. Neurofibromas usually intertwine themselves with several fascicles of surrounding nerves, which may increase the risk of dysfunction of the origin nerve when complete removal of the neurofibroma. For example, vocal cord paralysis was the most frequent postoperative complication in the patients mentioned in previous case reports (1,9). However, our surgical procedure outcomes showed that the mass was not only completely detached under the naked eye, but the vessels and nerves around were well protected. This satisfactory outcome might be accounted for by the following two points. Firstly, the tumor of the current case was relatively small compared to those reported previously. Secondly, are the different surgical strategies employed. With the development of minimally invasive surgery, BABA has become a well-established surgical technique with many reported benefits (4,5,15). Most recently, a large case-based meta-analysis (5) concluded that the efficacies and safety of total endoscopic thyroidectomy (TET) through multiple approaches, including but not limited to BABA, unilateral axillo-breast approach (UABA), anterior chest wall approach, and transoral approach, were similar to TOA for the treatment of thyroid cancer by comparison of the relevant indicators such as the level of surgical completeness, tumor recurrence rates, and postoperative complications. Notably, endoscopic surgery provides 3D vision and a magnified view of the operative field, significantly improving surgical precision. For instance, Zhang et al. (4) determined that TET was more beneficial for avoiding voice fatigue than TOA. Particularly when the tumor size was <4 cm, the rate of voice fatigue and total voice changes in the TET group were both significantly reduced (P1=0.009, P2=0.012, respectively), compared with the traditional group. Another advantage is the invisible incision, which meets the current high demand for satisfactory cosmetic results, compared with TOA groups. Thus, the endoscopic surgery via BABA we used preliminarily in this case has achieved encouraging results. This approach may qualify for other neck tumors, including carotid body tumors, thyroglossal duct cysts, and lipomas, worthy of further exploration.
Despite these advantages, there are still some notable limitations to the wide uptake of this technology. Endoscopic surgery has higher requirements for technical proficiency than TOA on behalf of surgeons (6). Besides, the difficulty of avoiding thermal cumulating is increased, with less tactile and strength feedback for surgeons, which may result in increased thermal damage to surrounding tissues. Lastly, TET’s operation time is relatively longer than TOA, which means patients must tolerate longer operative times under anesthesia. Based on the experience of this case and prior clinical practice in TET, we highly recommended using intraoperative nerve monitoring equipment, as one of the new techniques appearing in recent years, to effectively assist surgeons with determining the localization and preservation of the cervical nerves, such as recurrent laryngeal nerve, superior laryngeal nerve, and cervical sympathetic nerve during the operation (16,17). The major limitation of this case report is that only a single case was included. However, the successful application of endoscopic neck surgery via BABA in this patient can be leveraged to promote the development of this surgical technology for other neck tumors and diseases. Clearly, more evidence is urgently needed to strengthen its feasibility in clinical practice.
The solitary cervical VNN is a very rare neurogenic tumor type requiring serious consideration. Collaborative diagnosis including imaging examination, pathological examination, and immunohistochemistry can significantly improve the diagnostic accuracy of this disease. Endoscopic surgery via BABA is a potentially feasible and promising method for patients with neck mass.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/gs-20-706
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-20-706). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was provided by the patient according to institutional guidelines for publication of this case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray DP, Chan AK, Chin CT, et al. Large Cervical Vagus Nerve Tumor in a Patient with Neurofibromatosis Type 1 Treated with Gross Total Resection: Case Report and Review of the Literature. J Brachial Plex Peripher Nerve Inj 2016;11:e48-e54. [Crossref] [PubMed]
- Matejcik V, Steno J, Haviarova Z, et al. Neurofibroma of the vagus nerve in the cervical portion. Bratisl Lek Listy 2008;109:455-8. [PubMed]
- Desai KI. The Surgical Management of Symptomatic Benign Peripheral Nerve Sheath Tumors of the Neck and Extremities: An Experience of 442 Cases. Neurosurgery 2017;81:568-80. [Crossref] [PubMed]
- Zhang GL, Zhang GL, Lin YM, et al. Endoscopic thyroidectomy versus traditional open thyroidectomy for identification of the external branch of the superior laryngeal nerve. Surg Endosc. 2020. [Epub ahead of print]. [Crossref] [PubMed]
- Jiang WJ, Yan PJ, Zhao CL, et al. Comparison of total endoscopic thyroidectomy with conventional open thyroidectomy for treatment of papillary thyroid cancer: a systematic review and meta-analysis. Surg Endosc 2020;34:1891-903. [Crossref] [PubMed]
- Berber E, Bernet V, Fahey TJ 3rd, et al. American Thyroid Association Statement on Remote-Access Thyroid Surgery. Thyroid 2016;26:331-7. [Crossref] [PubMed]
- Ahlawat S, Blakeley JO, Rodriguez FJ, et al. Imaging biomarkers for malignant peripheral nerve sheath tumors in neurofibromatosis type 1. Neurology 2019;93:e1076-e1084. [Crossref] [PubMed]
- Singh T, Kliot M. Imaging of peripheral nerve tumors. Neurosurg Focus 2007;22:E6. [Crossref] [PubMed]
- Liu B, Zhang Y, Zhang L, et al. A rare case of bilateral cervical vagal neurofibromas: role of high-resolution ultrasound. BMC Neurol. 2017;17:26. [Crossref] [PubMed]
- Paratore C, Goerich DE, Suter U, et al. Survival and glial fate acquisition of neural crest cells are regulated by an interplay between the transcription factor Sox10 and extrinsic combinatorial signaling. Development 2001;128:3949-61. [PubMed]
- Miettinen M, McCue PA, Sarlomo-Rikala M, et al. Sox10--a marker for not only schwannian and melanocytic neoplasms but also myoepithelial cell tumors of soft tissue: a systematic analysis of 5134 tumors. Am J Surg Pathol 2015;39:826-35. [Crossref] [PubMed]
- Stefansson K, Wollmann R, Jerkovic M. S-100 protein in soft-tissue tumors derived from Schwann cells and melanocytes. Am J Pathol 1982;106:261-8. [PubMed]
- Sandler ML, Sims JR, Sinclair C, et al. Vagal schwannomas of the head and neck: A comprehensive review and a novel approach to preserving vocal cord innervation and function. Head Neck 2019;41:2450-66. [Crossref] [PubMed]
- de Araujo CE, Ramos DM, Moyses RA, et al. Neck nerve trunks schwannomas: clinical features and postoperative neurologic outcome. Laryngoscope. 2008;118:1579-82. [Crossref] [PubMed]
- Qu R, Li J, Yang J, et al. Treatment of differentiated thyroid cancer: can endoscopic thyroidectomy via a chest-breast approach achieve similar therapeutic effects as open surgery? Surg Endosc 2018;32:4749-56. [Crossref] [PubMed]
- Zhang D, Sun H, Tufano R, et al. Recurrent laryngeal nerve management in transoral endoscopic thyroidectomy. Oral Oncol 2020;108:104755. [Crossref] [PubMed]
- Ball JR, Biggs MT. Operative steps in management of benign nerve sheath tumors. Neurosurg Focus 2007;22:E7. [Crossref] [PubMed]



