Essential elements of the preoperative breast reconstruction evaluation
Introduction
Pre-operative planning for breast reconstruction patients is one of the most important aspects of the process and is often overlooked. Appropriate alignment of the patient’s desires and the surgeon’s abilities is critical to ensure realistic expectations and will contribute significantly to the patients overall satisfaction with the process, their surgeon and their final aesthetic result. We will discuss these factors based on our personal experience as well as highlight current literature regarding breast reconstruction.
Preoperative consultation
A proper initial consultation for breast reconstruction is obviously important in the road to a successful reconstruction process. This is often not a quick process and not only involves understanding the patient’s medical history and doing a physical examination, but also involves getting to know the patient from a personal and psychological perspective. A thorough evaluation of multiple factors in the patient’s medical history, physical examination, consideration of psychosocial factors and imaging is necessary to select the appropriate reconstructive technique. Level of education and socio-economic status may be useful as predictors of compliance and ability to successfully complete the reconstructive process. It is important to have an idea of the driving forces and motivations behind why patients are here discussing breast reconstruction (1). If the patient is only in the office because she was sent by her breast surgeon, or her significant other is forcing her to be there, then perhaps a more educational approach should be taken to allow the patient to make her own decision.
Most patients have been referred from an oncologic surgeon with a known diagnosis and a definitive plan for surgery and/or adjuvant therapy. It is important to review the pathological diagnosis to understand the tumor biology beyond simple benign versus malignant potential. Ductal carcinoma in situ behaves differently from lobular carcinoma in situ in contralateral risk. Some “benign” tumors (i.e., Phyllodes) have a high likelihood of locoregional recurrence and reconstruction may be best delayed. The plastic surgeon must consider the possible need for additional surgery (axillary lymph node dissection) and/or chemotherapy or radiation therapy. Patients with diffuse disease or large aggressive tumors (triple negative) may have positive margins despite mastectomy and need postoperative radiation. Lobular carcinoma and patients with BRCA mutation may benefit from bilateral mastectomy. Many surgeons prefer to delay reconstruction if postoperative radiation therapy is definitely indicated. Autologous reconstructions for example are often deferred until completion of radiation therapy and the decision on whether an expander or temporary reconstruction will be performed depends on the surgeon’s preferences, patient’s desires and also breast size/shape. If the patient has already had radiation therapy then this also directly impacts the decision process since prosthetic based reconstructions might be less preferable due to a higher complication rate (2). The reconstructive surgeon must consider individual tumor biology and staging prior to recommending reconstructive options.
A thorough review of the patient’s co-morbidities is crucial to understanding the possible risks of surgery and complications. A history of tobacco use is another important aspect of the preoperative evaluation that needs to be addressed. While smoking is not an absolute contraindication, the rate of mastectomy flap necrosis increases significantly in active smokers. Active heavy smokers with compromised vascularity of the mastectomy flap(s) may benefit from delayed reconstruction. The importance of preoperative smoking cessation is critical and even with being off cigarettes for at least a month prior to the procedure, there are certain procedures that would be less desirable in patients even with a remote history of smoking (3-5). Coagulopathy screening may be indicated in patients with significant family history or a personal history of embolic disease, deep venous thrombosis (DVT), and/or spontaneous abortions. Obesity alone is associated with higher complication rates including wound, medical, infection, major surgical, graft and prosthesis loss, and return to the operating room (6). Older age, smoking, obesity and BMI contribute to delayed wound healing in patients undergoing free tissue reconstruction (7). Patients with multiple co-morbidities are at higher risk for complications associated with increased length of surgery associated with complex autologous reconstruction. While it is often not feasible to have patients lose weight prior to the procedure if immediate reconstruction is planned, it is important to discuss the risk of potential complications with the patient and if deemed to be risky, delay reconstruction to allow for weight loss.
Physical exam
Examination of the patient’s breast size, shape and body habitus is obviously one of the more important parts of the preoperative evaluation. The surgeon needs to determine what they are trying to match if it is a unilateral reconstruction and what options the patient has for autologous reconstruction. The current breast size and desired postoperative breast size must be noted with equal importance. Patients may not have initially considered contralateral procedure for symmetry via mastopexy, augmentation, or reduction, however, this is important since it is often not possible to match a significantly ptotic, large or even small breast. Adjusting the opposite breast will often improve the ability to provide symmetry and needs to be discussed with the patient. It is important that the surgeon guide the patient in terms of breast size. Laterality is also important in determining the most appropriate reconstructive procedure. Some patients may adamantly refuse procedures on the contralateral breast and therefore the goal will be to match the native breast, and realistic expectations need to be presented. In patients with macromastia, reconstruction is often not possible without significant reduction on both sides. Patients desiring reduction in size and have smaller tumors may be amenable to oncoplastic approach (8). Most commonly patients desire matching breast size and therefore selection of implant versus tissue will depend on the volume of tissue available. Patient should be counseled that contralateral symmetry procedures are performed either simultaneously or in a delayed fashion (9).
During the examination attention should be focused on the patient’s breasts to note overall size and shape, location and size of masses in the breast/axilla, the position of the inframammary fold and nipple (grade of ptosis), nipple deformity (i.e., inversion), location of the biopsy scar, any chest wall deformity (i.e., pectus), skin changes (peau d’orange or radiation fibrosis) and any asymmetries. Measurements of the sternum to nipple, nipple to fold, and base diameter are taken to aid in selection of implants.
For patients considering autologous tissue reconstruction, the possible donor sites with adequate volume must be thoroughly examined. The abdomen is commonly used and should be noted for any previous surgical scars which may have damaged the vascularity or caused hernias. The Pfannenstiel scar is commonly encountered nowadays following Caesarian sections or hysterectomy but does not necessarily preclude the use of the abdominal tissue (10). Patients with subcostal scars are at slightly higher risk for abdominal wound healing complications (11). Approaches can be modified in such patients to minimize donor and flap morbidity utilizing preoperative imaging (12). While the back may lack adequate volume in a thinner patient, it may be ideal in obese patients with ample tissue (13). Alternatively if the abdominal donor site and back are not suitable, the inner thigh region can be considered for a transverse upper gracilis (TUG) flap (14) or profunda femoris artery perforator (PAP) flap (15). Also, the gluteal region is available in women using the superior or inferior gluteal artery perforator (SGAP/IGAP) flap (16). Some women may find these specific donor sites less culturally acceptable.
Pre-operative imaging
Any concern for disease in the contralateral breast requires complete evaluation with imaging and or biopsy prior to intervention to avoid missing any pathology. A review of preoperative imaging such as mammogram, ultrasound and MRI studies is useful to understanding tumor size and location. Additional preoperative imaging may be ordered by the reconstructive surgeon in mapping perforator anatomy to expedite surgery (17,18). Both CT angiography (CTA) and MR angiography require specific protocols for obtaining useful mapping of the perforator location (19,20). Preoperative CTA prior to deep inferior epigastric artery perforator (DIEP) flaps demonstrate good correlation between perforator locations to reduce operative time. However, clinical judgment at the time of dissection is still important in final perforator selection and successful flap harvest since the imaging may be inadequate. Keys et al. noted only 62 or 76 planned perforators were ultimately selected, with 23/52 flaps involving intraoperative changes based on clinical findings not apparent on preoperative imaging (21). For patients with prior extensive abdominal surgery, preoperative imaging can confirm the viability of perforators for abdominal based flaps. Preoperative imaging can also improve the chances of successful DIEP versus transverse rectus abdominis muscle (TRAM) flap harvest and decrease partial flap failure (22). The disadvantages include increased preoperative costs, radiation exposure, risk of contrast nephropathy, and a small risk of incidental findings requiring additional intervention. Nonetheless, several studies demonstrate reduced surgeon stress, decreased donor and recipient site complications, and improved operative time (23). Ultimately, the surgeon must use his/her best judgment in utilizing preoperative imaging appropriately to facilitate perforator flap breast reconstruction.
Conclusions
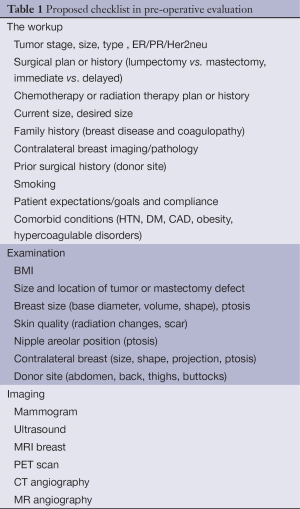
Preoperative evaluation of breast reconstruction is a complex process involving multiple components (Table 1). A successful relationship should be established after thorough evaluation of each individual patient history, imaging, physical exam, goals, and discussion of options to decide on the optimal reconstructive technique.
Full table
Acknowledgments
Disclosure: The authors declare no conflict of interest.
References
- Duggal CS, Metcalfe D, Sackeyfio R, et al. P Patient motivations for choosing postmastectomy breast reconstruction. Ann Plast Surg 2013;70:574-80. [PubMed]
- Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg 2009;124:395-408. [PubMed]
- Coon D, Tuffaha S, Christensen J, et al. Plastic surgery and smoking: a prospective analysis of incidence, compliance and complications. Plast Reconstr Surg 2013;131:385-91. [PubMed]
- Rinker B. The evils of nicotine: an evidence-based guide to smoking and plastic surgery. Ann Plast Surg 2013;70:599-605. [PubMed]
- Thomsen T, Villebro N, Møller AM. Interventions for preoperative smoking cessation. Cochrane Database Syst Rev 2014;3:CD002294. [PubMed]
- Fischer JP, Nelson JA, Kovach SJ, et al. Impact of obesity on outcomes in breast reconstruction: analysis of 15,937 patients from the ACS-NSQIP datasets. J Am Coll Surg 2013;217:656-64. [PubMed]
- Nelson JA, Chung CU, Fischer JP, et al. Wound healing complications after autologous breast reconstruction: A model to predict risk. J Plast Reconstr Aesthet Surg 2014. pii: S1748-6815(14)00682-2.
- Losken A, Pinell-White X, Hart AM, et al. The oncoplastic reduction approach to breast conservation therapy: benefits for margin control. Aesthet Surg J 2014;34:1185-91. [PubMed]
- Losken A, Carlson GW, Bostwick J 3rd, et al. Trends in unilateral breast reconstruction and management of the contralateral breast: the Emory experience. Plast Reconstr Surg 2002;110:89-97. [PubMed]
- Mahajan AL, Zeltzer A, Claes KE, et al. Are Pfannenstiel scars a boon or a curse for DIEP flap breast reconstructions? Plast Reconstr Surg 2012;129:797-805. [PubMed]
- Losken A, Carlson GW, Jones GE, et al. Importance of right subcostal incisions in patients undergoing TRAM flap breast reconstruction. Ann Plast Surg 2002;49:115-9. [PubMed]
- Hamdi M, Larsen M, Craggs B, et al. Harvesting free abdominal perforator flaps in the presence of previous upper abdominal scars. J Plast Reconstr Aesthet Surg 2014;67:219-25. [PubMed]
- Bailey SH, Saint-Cyr M, Oni G, et al. The low transverse extended latissimus dorsi flap based on fat compartments of the back for breast reconstruction: anatomical study and clinical results. Plast Reconstr Surg 2011;128:382e-394e. [PubMed]
- Arnez ZM, Pogorelec D, Planinsek F, et al. Breast reconstruction by the free transverse gracilis (TUG) flap. Br J Plast Surg 2004;57:20-6. [PubMed]
- Saad A, Sadeghi A, Allen RJ. The anatomic basis of the profunda femoris artery perforator flap: a new option for autologous breast reconstruction--a cadaveric and computer tomography angiogram study. J Reconstr Microsurg 2012;28:381-6. [PubMed]
- LoTempio MM, Allen RJ. Breast reconstruction with SGAP and IGAP flaps. Plast Reconstr Surg 2010;126:393-401. [PubMed]
- Rozen WM, Anavekar NS, Ashton MW, et al. Does the preoperative imaging of perforators with CT angiography improve operative outcomes in breast reconstruction? Microsurgery 2008;28:516-23. [PubMed]
- Nahabedian MY. Overview of perforator imaging and flap perfusion technologies. Clin Plast Surg 2011;38:165-74. [PubMed]
- Rozen WM, Phillips TJ, Stella DL, et al. Preoperative CT angiography for DIEP flaps: ‘must-have’ lessons for the radiologist. J Plast Reconstr Aesthet Surg 2009;62:e650-1. [PubMed]
- Agrawal MD, Thimmappa ND, Vasile JV, et al. Autologous breast reconstruction: preoperative magnetic resonance angiography for perforator flap vessel mapping. J Reconstr Microsurg 2015;31:1-11. [PubMed]
- Keys KA, Louie O, Said HK, et al. Clinical utility of CT angiography in DIEP breast reconstruction. J Plast Reconstr Aesthet Surg 2013;66:e61-5. [PubMed]
- Schaverien MV, Ludman CN, Neil-Dwyer J, et al. Contrast-enhanced magnetic resonance angiography for preoperative imaging in DIEP flap breast reconstruction. Plast Reconstr Surg 2011;128:56-62. [PubMed]
- Casey WJ 3rd, Rebecca AM, Kreymerman PA, et al. Computed tomographic angiography: assessing outcomes. Clin Plast Surg 2011;38:241-52. [PubMed]


