Primary squamous cell carcinoma (PSCC) of the thyroid: a case report and review of the literature
Introduction
Primary squamous cell carcinoma (PSCC) in thyroid is a rare cancer with the incidence less than 1% of all neoplasms of the thyroid (1). The typical clinical symptoms are rapidly growing neck mass, common extensions to the adjacent tissues and distant metastasis with mean diagnosis age over 50 and female prevalence. Therefore, thyroid PSCC has a very poor prognosis with a high death rate up-to 80% in three-year follow-up (2). Here, we report a rare case of PSCC of the thyroid and describe a complete diagnosis process, which included cervical ultrasonography, fiber-laryngoscope and positron emission tomography (PET) scan, with standardized treatment, which consisted of a complete total thyroidectomy with central compartment and unilateral neck dissection and postoperative radiation, We also summarize the diagnosis, treatment, and prognosis of thyroid PSCC by reviewing present literatures.
Case presentation
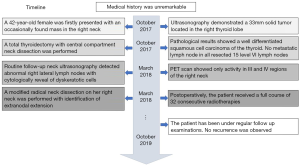
A 42-year-old female was firstly presented with an occasionally found mass in the right anterior neck in 2017 (Figure 1). Her medical history was unremarkable. Ultrasonography demonstrated that a solid, irregular, hypoechoic tumor with 35 mm × 23 mm × 23 mm located in the right thyroid lobe (Figure 2A). Chest X-ray and fiber-laryngoscope were free from advanced disease. She subsequently underwent a total thyroidectomy with central compartment neck dissection. The resected tumor presented as a single, solid, irregular mass with an intact capsule (Figure 2B), and pathological results showed a well differentiated squamous cell carcinoma of the thyroid (Figure 2C). Immunohistochemistry (IHC) showed that tumor cells were positive for CK, p63 and p40, and the Ki-67 labeling index was high (60%). Besides, there was no metastatic lymph node in all resected 15 level VI lymph nodes, and left thyroid lobe was absent from invasion of cancer as well.

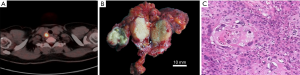
The patient refused local radiotherapy and radioactive iodine therapy (RAI), but only continued with TSH suppression treatment with TSH level below 0.5 mIU/L. 5 months later, abnormal right lateral cervical lymph nodes with cytologically reveal of cell clusters composed of dyskeratotic cells were identified during a routine follow-up neck ultrasonography. A positron emission tomography (PET) scan showed only activity in the III and IV regions of the right neck (Figure 3A). Then a modified radical neck dissection on her right neck was performed. During the surgery, severe extranodal extension was identified with infiltration to the right internal jugular vein and sternocleidomastoid muscle, therefore a comprehensive lymph nodes dissection was performed, along with right internal jugular vein and sternocleidomastoid muscle resection (Figure 3B). Pathological results confirmed the neoplasms to be PSCC of the thyroid origin (Figure 3C). The patient received a full course of 32 consecutive radiotherapies within one month postoperatively. And, no recurrence was observed at the follow-up visits in the next 18 months. Apart from a dry throat and dysphagia, the patient was satisfied at the comprehensive therapy she received.
Discussion
Primary squamous cell carcinoma is a rare cancer of the thyroid. The incidence of pure PSCC ranges from 0.2% to 1.1% of all neoplasms of the thyroid (1). Patients with PSCC routinely presented with rapidly growing neck mass, frequent extensions to the adjacent tissues and distant metastasis. Based on the clinical characteristics, most PSCC shared similar progression and prognosis with anaplastic carcinoma of the thyroid (3). The differential diagnoses of PSCC should include the following possibilities: a primary papillary thyroid carcinoma with squamous differentiation (PTC-SD), a primary PTC coexisted with a PSCC (collision tumor), a SCC of unknown origin metastasized to the thyroid, and a branchiogenic carcinoma in ectopic thyroid tissue. Moreover, a de-differentiation from a pre-existing papillary carcinoma should also be considered (4,5).
In our case, cervical ultrasonography and PET scan excluded extension from the hypopharynx, larynx, or oesophagus or metastasis from lung, nasopharynx, or other primary locations. Typical squamous cell morphology was observed in histopathological tests, with no sign of any other thyroid carcinoma cells. Immunohistochemistry can elucidate the typical cytokeratin pattern (CK) which is crucial to exclude a squamous cell carcinoma deriving or coexisting with a papillary carcinoma of the thyroid (6). A high Ki-67 proliferation index (60% in our case) and overexpression of oncoprotein p63 are associated with poor prognosis and an increased risk of postoperative local recurrence (1).
The main treatment is complete surgical resection of the tumor with thyroidectomy, along with infiltrated tissues and regional lymph nodes, while ensuring negative surgical margins, as negative surgical margins have been shown to be the only factor for a good prognosis (2). However, the use of adjuvant therapy is still controversial. The argument is between the viewpoint that thyroid PSCC is poorly responsive to either radiotherapy or chemotherapy and the concern of operation alone is not a sufficient treatment for PSCC because of the high risk of tumor relapse (2,7,8). Nevertheless, almost all described cases with disease free survival received an additional radiotherapy and/or chemotherapy. In this case, our intervention was successful based on the fact of no tumor recurrence. But the process of PSCC diagnosis and treatment can also be improved. A preoperative fine needle aspiration (FNA) biopsy of the primary tumor could be performed, and the PET scan may be scheduled before the first surgery. On the other hand, a right lateral cervical lymph nodes dissection was needed only 5 months after the first surgery verified the poor prognosis of PSCC, a prophylactic lateral cervical lymph nodes dissection and additional radiotherapy may be considered at the primary surgery.
A review by Cho et al. in 2014 reported 89 cases of primary squamous cell carcinoma of the thyroid in 39 publications. Apart from the anterior neck mass, 72% of the patients were presented as adjacent structure infiltration. The median survival was 9.0 months (95% CI, 6.0–23.0 months) and 3-year survival rate was down to 20.1%. Complete resection of tumors was the only significant prognostic factor, and the benefit of adjuvant treatment has not been proved (2). Shrestha et al. indicated in a review in 2013 that the presence of lymph node metastasis is also an important negative prognostic factor, the patients with positive lymph node metastasis have a shorter mean overall survival compared with those without metastasis (10.8 vs. 16.4 months) (1). Unlike papillary thyroid carcinoma, which has a tendency of reginal lymph nodes metastasis but a good prognosis (9), the majority of thyroid PSCC has a poor prognosis apart from occasionally reported patients with thyroid PSCC with a good prognosis (10). Hence, the staging and treatment might be analog to that of anaplastic thyroid carcinoma.
In conclusion, we added one PSCC case with typical presentation and unusual clinical courses to the literature. Although PSCC is rare, it should be taken into consideration in the differential diagnosis of thyroid neoplasms. The management of the disease requires a multi-disciplinary approach.
Acknowledgments
Funding: This work was supported by grants from the National Natural Science Foundation of China (81701921) to BH Sun.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs.2020.02.18). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The information includes examination images and results, surgical photographs, et al., which has been approved by ethical review by the ethics committee of Nanfang Hospital, Southern Medical University. Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shrestha M, Sridhara SK, Leo LJ, et al. Primary squamous cell carcinoma of the thyroid gland: a case report and review. Head Neck 2013;35:E299-303. [PubMed]
- Cho JK, Woo SH, Park J, et al. Primary squamous cell carcinomas in the thyroid gland: an individual participant data meta-analysis. Cancer Med 2014;3:1396-403. [Crossref] [PubMed]
- Booya F, Sebo TJ, Kasperbauer JL, et al. Primary squamous cell carcinoma of the thyroid: report of ten cases. Thyroid 2006;16:89-93. [Crossref] [PubMed]
- Rausch T, Benhattar J, Sutter M, et al. Thyroid carcinoma with papillary and squamous features: report of a case with histogenetic considerations. Pathol Res Pract 2010;206:263-9. [Crossref] [PubMed]
- Syed MI, Stewart M, Syed S, et al. Squamous cell carcinoma of the thyroid gland: primary or secondary disease? J Laryngol Otol 2011;125:3-9. [Crossref] [PubMed]
- Vardar E, Erkan N, Bayol U, et al. Metastatic tumours to the thyroid gland: report of 3 cases and brief review of the literature. Radiol Oncol 2011;45:53-8. [Crossref] [PubMed]
- Ito Y, Hirokawa M, Higashiyama T, et al. Biological behavior of papillary carcinoma of the thyroid including squamous cell carcinoma components and prognosis of patients who underwent locally curative surgery. J Thyroid Res 2012;2012:230283. [Crossref] [PubMed]
- Cook AM, Vini L, Harmer C. Squamous cell carcinoma of the thyroid: outcome of treatment in 16 patients. Eur J Surg Oncol 1999;25:606-9. [Crossref] [PubMed]
- Yu ST, Ge JN, Sun BH, et al. Lymph node metastasis in suprasternal space in pathological node–positive papillary thyroid carcinoma. Eur J Surg Oncol 2019;45:2086-9. [Crossref] [PubMed]
- Wygoda A, Rutkowski T, Szczesniak-Klusek B, et al. Primary squamous-cell thyroid carcinoma - a successful treatment with five-year follow-up. Endokrynol Pol 2017;68:592-6. [PubMed]