Comparing LigasureTM Exact dissector with other energy devices in total thyroidectomy: a pilot study
Introduction
Thyroidectomy is an operation requiring prime hemostasis in order to avoid, both intra- and post-operative, complications. The golden standard technique of clamps-and-ties tends to be abandoned by most high volume surgeons. Alternatively, in modern clinical practice a large number of devices have been introduced in clinical practice to achieve a safer and faster hemostasis (1-5). The choice of which energy-based device is employed, is more or less a result of the combination of personal preference of the surgeon and of availability (5). Various studies demonstrate marginal differences between the devices concerning hemorrhage, parathyroid function alterations and voice changes. In everyday practice there are 3 major hemostatic devices notably: Focus Harmonic Scalpel, LigasureTM Small Jaw and Thunderbeat. The Focus Harmonic Scalpel uses ultrasound vibration of a blade at 55 Hz. The resulting mechanical energy is transferred to tissue proteins, resulting in their denaturation. Protein denaturation results in a protein coagulum that seals the vessels and assures hemostasis at low temperatures. The LigasureTM Small Jaw is a bipolar coagulation device that denatures the collagen and elastin of the vascular wall. Finally, Thunderbeat® (TB) (Olympus Medical Systems Corp., Tokyo, Japan) is the first device to simultaneously integrate ultrasonically generated frictional heat energy and electrically generated bipolar energy. The ultrasonic technology is used for rapid cutting and precise dissection while the bipolar technology performs reliable vessel sealing. TB is considered advantageous due to its ability to gain a rapid surge in temperature with minimal thermal spreading. Recently, LigasureTM Exact was introduced adding a new instrument in the arsenal of endocrine surgeon (6-8). This instrument works in the same fashion that Ligasure Small Jaw works, but has a special anatomic design that makes it easier to work in tight spaces, by maximizing the line of sight.
The aim of this randomized active comparator-controlled study in patients undergoing total thyroidectomy was to evaluate and compare the effectiveness of the previously existing vessels sealing devices, notably Focus Harmonic Scalpel, LigasureTM Small Jaw and Thunderbeat, to the newly introduced LigasureTM Exact. In the present study classical parameters such as duration of the surgery, blood loss, calcium variations, immediate postoperative complications, and hospitalization were measured, together with visual analogue scale (VAS) quantifications of intraoperative difficulty, postoperative vocal alteration, and postoperative pain.
Methods
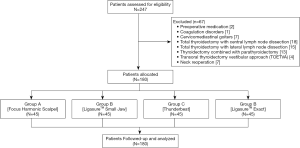
From December 3, 2018 through May 31, 2019, 247 adult patients, with benign or malignant thyroid disease, scheduled for total thyroidectomy at the Unit of Minimally Invasive Endocrine Surgery and 1st Propedeutic Department of AHEPA University Hospital of Thessaloniki, were assessed for elegibility and 180 among them were randomly allocated into 4 groups according to the hemostatic energy device used: Focus Harmonic Scalpel® (group A), LigasureTM Small Jaw (group B), Thunderbeat® (group C), and LigasureTM Exact (group D). Randomization was achieved by creating 180 envelopes containing each one letter (4 times 45 envelopes with each of the four letters) from which the patient chose one and was allocated in the respective group. The study was approved by the ethics committee of AHEPA University Hospital (46432/6.11.2018).
The inclusion criteria were: (I) age >18 years; (II) acceptance to participate in the study (signed informed consent form); and (III) scheduled total thyroidectomy (under euthyroid status). The exclusion criteria were: (I) preoperative medication including opioid or non-opioid analgesics, corticosteroids, or nonsteroidal anti-inflammatory drugs; (II) coagulation disorders; (III) pregnancy; (IV) cervicomediastinal goiters; (V) total thyroidectomy with lymph node dissection; (VI) thyroidectomy combined with parathyroidectomy, (VII) transoral thyroidectomy vestibular approach (TOETVA) and (VIII) neck reoperation. Figure 1 shows the patient flow diagram.
All procedures were performed by the same surgical team dedicated to endocrine surgery. In order to assess vocal cord motility, all patients underwent pre- and post- operative (at 24 hours) flexible nasopharyngolaryngoscopy to assess vocal cord motility. For devascularizing the gland the team employed in group A Focus Ultracision Harmonic Scalpel (Ethicon Endo-Surgery Inc., Cincinnati, OH, USA), in group B LigasureTM Small Jaw Open sealer/divider (Covidien, Boulder, CO, USA), in group C Thunderbeat® (Olympus Medical Systems Corp., Tokyo, Japan), and in group D LigasureTM Exact Dissector (Covidien, Boulder, CO, USA) (group D). In the area around the ligament of Berry in all cases we employed 4/0 Vicryl ligations. Both groups received 2 doses of lornoxicam 8 mg (Xefo® TAKEDA Hellas, Greece), at the end of the operation and one 12 hours later.
After preoxygenation, general anesthesia was induced with 3 µg/kg fentanyl and 2 mg/kg propofol, followed by 0.6 mg/kg rocuronium. The ventilator was set in volume-controlled mode for all patients. Anesthesia was maintained with sevoflurane and remifentanil infusion; all the patients were administered 4 mg dexamethasone, 4 mg ondansetron, 1,000 mg paracetamol, and 8 mg lornoxicam.
Postoperative pain was assessed by the visual analogue rating scale (VAS), ranging from 1 (no pain) to 10 (worst imaginable pain). Intraoperative difficulty was rated with a scale ranging from 1 (very easy) to 5 (very difficult).
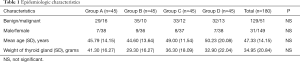
A VAS, ranging from 1 (no voice alteration) to 10 (worst imaginable alteration) was used to assess postoperative voice alteration. Pain and voice changes were self-assessed by the patient. Concerning the operative difficulty was evaluated by an observing physician. Operative difficulty was assessed by a rating scale ranging from 1 (very easy) to 5 (very difficult) (9). All operations started from 3 (normal difficulty) and changed to higher or lower difficulty categories according to intraoperative routine changes, time and effort spend for hemostasis, discomfort of the operating physician etc. The observing physician was constant for all operations, namely an emeritus professor who was performing thyroidectomies on a regular basis. Parathormone (PTH), ionized calcium and phosphorus levels were determined on the first postoperative day. When PTH was less than 14 pg/dL (inferior normal range limit for our laboratory), or the patient had clinical hypocalcemia (calcium level below the lower limit of normal range (8.2 mg/dL) associated with a Chvostek sign or patient complaint of paresthesia), then patients received oral calcium carbonate (1,000 mg three times a day) and vitamin D3 supplementation. The following data were recorded according to our previously published protocols (9,10): age, gender, pathology, thyroid weight, hemostatic technique, duration of the operation, postoperative and preoperative calcemia, pre- and post-operative hemoglobin, pre- and post-operative white blood cell count, pre- and post-operative PTH, pre- and post-operative vocal cord motility, operative difficulty, postoperative vocal alteration, postoperative pain, complications, operating time, gram of gland excised per minute of the operation (weight of gland/duration of the operation), and length of hospital stay. The epidemiologic characteristics of all groups are indicated in Table 1.
Full table
An intention-to-treat analysis has been used in our study. Continuous variables were compared using the Mann-Whitney U test, while categorical variables were compared using the Chi square test. If the expected frequency was smaller than 5, the Fisher exact test was used. Statistical evaluation of the four groups was performed by one-way analysis of variance (ANOVA) with Bonferroni test for post hoc analysis. Continuous data are summarized as mean ± standard deviation. Probability values <0.05 were considered statistically significant. All analyses were performed by SPSS Version 18 software (Chicago, IL, USA).
The mean and standard deviation of duration of surgery in a 40-patient pilot study (n=10 patients per group) were used for power calculations; for P=0.05 and power =0.8, a minimum of 42 patients in each group were required. We employed 45 patients per group taking into consideration that there might be 5% of data lost.
Results
Hospitalization was the same for all groups since all patients stayed for a single day in the hospital (+/−2 hours). The small differences of stay were not due to medical, but mainly due to administrative reasons. No patients were lost in follow-up and all patients were included in statistical analysis.
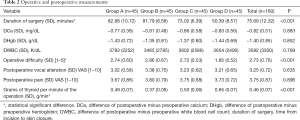
Statistically significant differences between groups were observed concerning duration of the surgery (P<0.001), mean operative difficulty (P<0.001), and the quantity of gland removed per minute of operation (P<0.001). All the other measured parameters were comparable for all four groups. The results concerning all the measured parameters in both groups are displayed in Table 2.
Full table
Post hoc tests for duration of surgery showed no differences between group A (Focus Ultracision Harmonic Scalpel) and group B (LigasureTM Small Jaw Open sealer/divider) (P=1.00), while there was a difference between those two groups and groups C and D (P<0.001). By this, it is confirmed that Thunderbeat® and LigasureTM Exact Dissector are devices that shorten significantly the duration of the operation. Moreover, when comparing those two devices between them, one can see that LigasureTM Exact Dissector is further reducing operative time (P<0.001).
Given the fact that the amount of gland removed per minute of operation is calculated by dividing the weight of the thyroid removed by the time of the operation, and that there was no statistical differences concerning the weight of the gland between groups, it seems logical this parameter also presents statistically significant differences between groups (P<0.001). The greatest quantity of thyroid removed per minute is done by LigasureTM Exact Dissector (P<0.001), followed equally (no statistical difference between groups) by Focus Ultracision Harmonic Scalpel and Thunderbeat®. The least amount of gland removed per minute is by Ligasure Small Jaw Open sealer/divider (P<0.001).
Finally, the objective observer noted that the mean operative difficulty presented statistically significant differences between groups (P<0.001). All three devices (Focus Ultracision Harmonic Scalpel, LigasureTM Small Jaw Open sealer/divider and Thunderbeat®) showed equal level of intraoperative difficulty for the surgeon. However, LigasureTM Exact Dissector was noticed to expose the surgeon to less operative difficulty (P<0.001).
Additionally, one clinical hypocalcemia was present for group A and one for group B. Moreover, low PTH levels were present in 6 patients for groups A and B, while in 7 patients for groups C and D (P=NS). It is important to notice that no recurrent laryngeal nerve (RLN) palsies were observed. Hematomas requiring re-operations were not observed in all groups.
Discussion
Since Kocher, hemostasis was considered of prime importance for a safe thyroidectomy. When performing a classic clamp-and-tying thyroidectomy two parameters may problematize the surgeon; one is post-operative bleeding and the second is the time consumed in tying. Secondarily, some surgeons may also consider the foreign material (sutures) introduced into the operative field (10). Therefore, new technologies have emerged the last 15years and have been introduced in surgical practice, aiming primarily to decrease postoperative complications and to save time (11-17). Since the initial introduction of Harmonic Scalpels to thyroid surgery, several prospective and retrospective studies have been performed comparing either energy devices between them or with the standard clamp-and-tie technique, mainly evaluating duration of the surgery, blood loss, and complications. The present study has two particularities; first it tests a newly introduced energy device (LigasureTM Exact), and second it additionally considers operative difficulty, postoperative pain, and vocal alteration.
Total thyroidectomy is an operation performed frequently, with no mortality and low morbidity. Morbidity mainly results from postoperative RLN palsy (transitory or definite) and hypocalcemia (clinical or nonclinical, transitory or definite). Incidence of RLN palsies varies from 0% to 23%, whereas transient asymptomatic hypocalcemia after total thyroidectomy may reach 63% (18). Those two complications are valuable to be evaluated for all four instruments employed for the present study. Concerning the status of the parathyroid function, this study demonstrated no difference, concerning both clinical hypocalcemia and hypoparathyroidism, for all four instruments. Additionally, there were no RLN palsies for all groups, characterizing all four instruments equally safe. Moreover, by using a VAS to evaluate the patients’ perception of voice alteration as previously described (10), we measured no differences between the 4 compared groups. This seems very logical since all groups had no RLN palsies. However, voice alteration score was not null for all groups, suggesting that even if we cannot identify by laryngoscopy RLN or superior laryngeal nerf (SLN) injury, the patient perceives and quantifies voice alteration. This phenomenon is probably not due to stretching, compression, or ischemia of the nerve (either RLN or SLN) as previously thought (10,19-21), but due to other, mainly muscular elements, that contribute the phonation and are affected by the operation.
Concerning the hematologic changes induced by each instrument, we observed no difference in DHb and DWBC. This means that the intraoperative blood loss—as expressed by changes of the hematocrit—is small and thus clinically not significant, with no impact on everyday clinical practice. Additionally, we observed that there was no difference between the WBC changes in all groups postoperatively. Since WBC is a rough but routinely used in everyday practice indicator of the acute inflammatory response to trauma, by this data one can estimate the acute inflammatory response of all four instruments as equivalent. However, we have to acknowledge that WBC changes provide a rough estimate of the acute inflammatory response. It is well known that the cellular events of acute inflammation are heralded by the tissue influx of large numbers of neutrophils. These cells have a well-established potential to injure tissues by a variety of mechanisms (22,23). However, it is also clear that acute inflammation has evolved as part of the beneficial host response to injury and infection that normally resolves with minimal residual tissue damage (24). In a previous study, we have demonstrated that WBC changes were smaller in total thyroidectomy performed by Ultracision than when performed with the classic clamp-and-tie technique. Nevertheless, the changes of WBC are only a rough marker and might be confounded by differences in the neutrophil response between different individuals. In addition, differences in white blood cell count (or the lack thereof) may be confounded by ongoing infection (which is rare in this type of operations).
Another indirect way to evaluate the acute inflammatory reaction is patients’ perception of pain. As previously described, a VAS was employed to evaluate differences of postoperative pain between the various energy devices. It is well known from previous studies that postoperative pain after total thyroidectomy is low (10). Additionally to DWBC, the fact that there was no statistical difference between the four instruments as far as pain VAS is concerned, let us suggest that all these devices produce an acute inflammatory reaction of the same magnitude.
Finally, three additional parameters were used to evaluate the operative effectiveness of the four energy devices: (I) duration of the operation; (II) intraoperative difficulty; and (III) grams of gland removed in the unit of time (minute). LigasureTM Exact Dissector seems to have better operative effectiveness concerning all these three parameters. Indeed, the present study demonstrates that LigasureTM Exact Dissector reduces the operative time by approximately 30 minutes. This shortening of the duration of the operation is probably due to the fact that this device provides a better and more precise dissection reducing to absolute minimum the use of a separate dissector. According to Medtronic’s internal report (as it is mentioned in the official site) surgeons say that Ligasure Exact has an enhanced ability to work in tight spaces (when compared to Ligasure Small Jaw and Focus Harmonic Scalpel) (25). Moreover, Ligasure Exact’s tip stays cool even after multiple activations, making it almost directly available for reactivation, property that is not evident when using Focus or Thunderbeat. Additionally, LigasureTM Exact Dissector seems to help the surgeon remove a larger amount of thyroid tissue per minute of operation. Finally, even in surgical instruments, effectiveness it is not always only a matter of speed but also a matter of comfort. According to a 5-grade scale that we have already used in previous studies (10), when the operation is performed with the use of LigasureTM Exact Dissector it seems to have a considerably lower operative difficulty. When comparing operative effectiveness of the other three devices (Focus Ultracision Harmonic Scalpel, LigasureTM Small Jaw Open sealer/divider and Thunderbeat®), Thunderbeat seems to outperforms the other two concerning the duration of surgery. However, measuring operative difficulty is not an easy task. Per se operative difficulty is not an objective term and may by influenced by the case itself (i.e., the size or location of the tumor, the presence of thyroiditis, body habitus of the patient). Moreover, in our study, intraoperative difficulty was evaluated by only one observing physician which may be subject to bias.
The use of energy devices thyroidectomy either total or not, is a reality for most surgeons. The most commonly used are Focus Harmonic Scalpel, LigasureTM Small Jaw and Thunderbeat, while recently LigasureTM Exact Dissector was introduced to the arsenal of surgeons. Compared between them these energy devices seem to be equivalent concerning post-operative complications (both nerf injuries and post-operative parathyroid dysfunction), hemostasis, and acute inflammatory reaction. However, the newly introduced LigasureTM Exact Dissector seems to have better results when coming to duration of surgery, quantity of thyroid tissue removed per minute and intraoperative difficulty. Of course, these results need further exploration by more studies, but for the time being it seems that the new device comes to add something useful into the already existing arsenal.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs.2020.02.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the ethics committee of AHEPA University Hospital (46432/6.11.2018).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Materazzi G, Ambrosini CE, Fregoli L, et al. Prevention and management of bleeding in thyroid surgery. Gland Surg 2017;6:510-5. [Crossref] [PubMed]
- Ruggiero R, Gubitosi A, Conzo G, et al. Sutureless thyroidectomy. Int J Surg 2014;12 Suppl 1:S189-93. [Crossref] [PubMed]
- Teksoz S, Bukey Y, Ozcan M, et al. Sutureless thyroidectomy with energy-based devices: Cerrahpasa experience. Updates Surg 2013;65:301-7. [Crossref] [PubMed]
- Van Slycke S, Gillardin JP, Van Den Heede K, et al. Comparison of the harmonic focus and the Thunderbeat for open thyroidectomy. Langenbecks Arch Surg 2016;401:851-9. [Crossref] [PubMed]
- Bakkar S, Papavramidis T, Aljarrah Q, et al. Energy-based devices in thyroid surgery—an overview. Gland Surg 2020;9:S14-7. [Crossref] [PubMed]
- Papavramidis TS, Anastasiou O, Pliakos I, et al. Parathyroid function after total thyroidectomy: a randomized clinical trial concerning the influence of the surgical technique. Endocr Pract 2018;24:150-5. [Crossref] [PubMed]
- Carlander J, Wagner P, Gimm O, et al. Risk of Complications with Energy-Based Surgical Devices in Thyroid Surgery: A National Multicenter Register Study. World J Surg 2016;40:117-23. [Crossref] [PubMed]
- Park MW, Baek SK, Park EH, et al. Long-term voice outcome after thyroidectomy using energy based devices. Auris Nasus Larynx 2018;45:527-32. [Crossref] [PubMed]
- Papavramidis TS, Sapalidis K, Michalopoulos N, et al. UltraCision harmonic scalpel versus clamp-and-tie total thyroidectomy: a clinical trial. Head Neck 2010;32:723-7. [PubMed]
- Anastasiou OE, Yavropoulou MP, Papavramidis TS, et al. Secretory capacity of the parathyroid glands after total thyroidectomy in normocalcemic subjects. J Clin Endocrinol Metab 2012;97:2341-6. [Crossref] [PubMed]
- Defechereux T, Rinken F, Maweja S, et al. Evaluation of the ultrasonic dissector in thyroid surgery. A prospective randomised study. Acta Chir Belg 2003;103:274-7. [Crossref] [PubMed]
- Manouras A, Lagoudianakis EE, Antonakis PT, et al. Electrothermal bipolar vessel sealing system is a safe and time-saving alternative to classic suture ligation in total thyroidectomy. Head Neck 2005;27:959-62. [Crossref] [PubMed]
- Miccoli P, Berti P, Dionigi GL, et al. Randomized controlled trial of harmonic scalpel use during thyroidectomy. Arch Otolaryngol Head Neck Surg 2006;132:1069-73. [Crossref] [PubMed]
- Kiriakopoulos A, Tsakayannis D, Linos D. Use of a diathermy system in thyroid surgery. Arch Surg 2004;139:997-1000. [Crossref] [PubMed]
- Siperstein AE, Berber E, Morkoyun E. The use of the harmonic scalpel vs conventional knot tying for vessel ligation in thyroid surgery. Arch Surg 2002;137:137-42. [Crossref] [PubMed]
- Ortega J, Sala C, Flor B, et al. Efficacy and cost-effectiveness of the UltraCision Harmonic Scalpel in thyroid surgery: an analysis of 200 cases in a randomized trial. J Laparoendosc Adv Surg Tech A 2004;14:9-12. [Crossref] [PubMed]
- Sartori PV, De Fina S, Colombo G, et al. LigaSureTM versus UltraCisionVR in thyroid surgery: a prospective randomized study. Langenbecks Arch Surg 2008;393:655-8. [Crossref] [PubMed]
- Rosato L, Avenia N, Bernante P, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 2004;28:271-6. [Crossref] [PubMed]
- Spinelli C, Berti P, Miccoli P. Identification of the recurrent nerve in thyroid surgery. Technical note. Minerva Chir 1995;50:93-6. [PubMed]
- Sasson AR, Pingpank JF, Wetherington RW, et al. Incidental parathyroidectomy during thyroid surgery does not cause transient symptomatic hypocalcaemia. Arch Otolaryngol Head Neck Surg 2001;127:304-8. [Crossref] [PubMed]
- Bergamaschi R, Becouarn G, Ronceray J, et al. Morbidity of thyroid surgery. Am J Surg 1998;176:71-5. [Crossref] [PubMed]
- Malech HL, Gallin JI. Current concepts: immunology. Neutrophils in human diseases. N Engl J Med 1987;317:687-94. [Crossref] [PubMed]
- Weiss SJ. Tissue destruction by neutrophils. N Engl J Med 1989;320:365-76. [Crossref] [PubMed]
- Smith JA. Neutrophils, host defense and inflammation: a double edge sword. J Leukoc Biol 1994;56:672-86. [Crossref] [PubMed]
- Introducing the LigasureTM exact dissector. Available online: https://www.medtronic.com/covidien/en-us/products/vessel-sealing/ligasure-exact-dissector.html. [Accessed 13 January 2020].