
The role of parathyroidectomy in treating hypertension and other cardiac manifestations of primary hyperparathyroidism
Introduction
Primary hyperparathyroidism (PHPT) is a relatively common endocrine disorder characterized by elevated calcium levels along with parathyroid hormone (PTH) levels that are either elevated or inappropriately normal. Detrimental effects of prolonged elevated PTH levels include osteopenia and osteoporosis, development of kidney stones as a result of increased urinary excretion of calcium, decrease in renal function, osteitis fibrosa cystica, and peptic ulcers. There are also multiple subjective symptoms attributable to elevated calcium levels that include depression, constipation, extremity aches, mental fog, fatigue, lethargy, and other neurocognitive symptoms. Other more poorly understood effects of PHPT include higher incidence of hypertension, metabolic syndrome, vascular and valvular calcifications, and other cardiovascular manifestations. The only method of achieving cure of PHPT is through surgical removal of the abnormal gland or glands. It is well-established that successful parathyroid surgery leads to improvement in bone health and can halt the progression of renal damage. Studies have also shown that subjective symptoms improve after successful surgery. There is conflicting data regarding the effect of parathyroid surgery on cardiac manifestations such as hypertension and metabolic syndrome. As such, the most recent guidelines released from the National Institutes of Health (NIH) and the American Association of Endocrine Surgeons (AAES) do not list cardiovascular comorbidities as an indication to operate on patients with PHPT.
Epidemiology and diagnosis
PHPT occurs in 1 to 7 cases per 1,000 adults. It is caused by autonomous secretion of PTH by one or more parathyroid glands. Elevated levels of PTH result in increased absorption of calcium from the gut and resorption of calcium from bone (1). Around 85% of cases are caused by a single adenoma that is functioning autonomously (2). The remaining cases are a result of hyperplasia of multiple glands. Clinical presentation of PHPT can vary widely. A large percentage of patients may be asymptomatic or complain of multiple nonspecific symptoms such as extremity pain, fatigue, weakness, abdominal discomfort, or cognitive dysfunction. Patients with symptoms from PHPT may present with a history of kidney stones, nephrocalcinosis, osteoporosis, fragility fractures, pancreatitis, or peptic ulcer disease. There may also be cardiac manifestations associated with PHPT. These include hypertension, metabolic syndrome, calcific valvular and vascular disease, left ventricular hypertrophy (LVH), and others (1).
The diagnosis of PHPT is made based on biochemical testing. Elevated serum calcium levels are often seen with elevated or inappropriately normal PTH levels. Hypophosphatemia and elevated alkaline phosphatase levels are common but not necessary to make the diagnosis. It is also common to see low 25-OH Vitamin D levels. Twenty-four-hour urine calcium levels are elevated as a result of increased urinary excretion of calcium by the kidneys. The only treatment capable of curing PHPT is parathyroidectomy (1,3). Cure rates with surgery approach greater than 95% (2). Biochemical cure of PHPT has been shown to have a positive impact on bone health and decreased formation of renal stones over time.
Signs and symptoms of PHPT
Objective symptoms related to PHPT are attributed to high levels of serum calcium and the effects of elevated PTH over time. The most common manifestations related to symptomatic PHPT involve the renal and musculoskeletal systems. Increased serum calcium levels stimulate the kidneys to secrete calcium in the urine, which can lead to formation of kidney stones as well as nephrocalcinosis. Over time, overall kidney function can decline (1).
Osteopenia and osteoporosis are common manifestations of parathyroid disease. Normal PTH production results in net bone formation due to intermittent secretion of the hormone, which can act as both an anabolic and catabolic agent. Paradoxically, continuous elevated levels of PTH, like in PHPT, lead to net bone loss (4). PTH acts on osteoclasts to resorb bone and release calcium into the bloodstream. Increased bone turnover leads to loss of bone density classically seen in cortical bone of the distal radius and femoral neck. These patients may have a fracture risk that is 2- to 3-fold higher than individuals without parathyroid disease (1).
Elevated calcium levels are associated with other disease processes such as acute pancreatitis and peptic ulcer disease. These entities are seen less frequently due to the increased use of medications such as proton pump inhibitors. Multiple subjective symptoms of hypercalcemia are seen in patients with PHPT. They are nonspecific and include fatigue, weakness, mild depression, irritability, decreased appetite, abdominal discomfort, extremity aches, and diminished cognitive function (1,3).
The role of parathyroidectomy in treating the cardiovascular manifestations of PHPT is controversial as the data regarding the effects of parathyroidectomy on cardiovascular manifestations is conflicting.
Current state review
Cardiovascular manifestations of PHPT
PHPT has been associated with hypertension and many other cardiovascular risk factors including atherosclerosis, impaired glucose metabolism, arrhythmias, structural heart abnormalities, myocardial infarction, and increased risk of death (5,6). The exact mechanisms are not completely understood. Elevated serum calcium levels as well as direct tissue effects of PTH have been implicated. Prevalence of hypertension in patients with PHPT ranges from 40–65% (6). There are several theories that consider how PHPT may lead to elevated arterial blood pressure. Patients with elevated PTH levels have higher circulating levels of renin, angiotensin, aldosterone, and norepinephrine. Endothelial cells are also more sensitive to pressor hormones, resulting in a more potent vasoconstricting response. Structural changes to the endothelium itself may also lead to increased arterial pressures (7).
Impaired glucose metabolism and type 2 diabetes mellitus are more prevalent among patients with PHPT than the general population. As with arterial hypertension, the exact mechanism behind this is not well understood. Serum calcium alters the affinity of insulin receptors and PTH concentration also plays a role in insulin sensitivity.
Patients with PHPT have been found to have structural changes related to blood vessels and the heart itself. LVH and elevated left ventricular mass index (LVMI) is seen in PHPT (8). Other measures of vascular disease have been associated with PHPT. Walker and colleagues found that patients with PHPT were more likely to have an increased carotid-intima media thickness (IMT) as well as decreased carotid distensibility (9). Echocardiographic examination of patients with PHPT have demonstrated an elevated prevalence of LVH even in those without HTN (7).
In addition to increased incidence of cardiovascular risk factors, a large Swedish study that examined long-term results of surgery versus medical management of over 3,000 patients found that patients in the medical group had higher mortality rates from all causes than patients treated with parathyroidectomy. Patients in the surgical arm did not experience a lower risk of acute cardiac events, however (5).
Surgical management of parathyroid disease
The only definitive treatment for PHPT is surgery. Medications such as calcimimetics and bisphosphonates can be used to treat hypercalcemia and osteoporosis, but they are generally reserved for patients who are unable or unwilling to undergo parathyroidectomy. Patients who are asymptomatic or do not meet criteria for surgery may be observed with periodic laboratory and bone density assessment (1,2).
Recommendations from several societies exist to guide clinicians regarding when patients with PHPT should be considered for surgical management. Guidelines from the Fourth International Workshop for the management of asymptomatic PHPT were released most recently in 2013. These are listed in Table 1 (10). In 2016, the American Association of Endocrine Surgeons also published recommendations concerning surgical management of PHPT. It is widely appreciated that patients and physicians both find it difficult to determine whether the patient is truly asymptomatic. Therefore, even those who do not meet criteria or exhibit symptoms may be referred to an endocrine surgeon to be evaluated for operative treatment.
The specific criteria for making the diagnosis of PHPT is beyond the scope of this article. However, once a biochemical diagnosis is made, that is all that is required to then consider a surgical referral. Imaging modalities such as cervical ultrasound, sestamibi scan, MRI, and 4D computed tomography may be performed to assist with localization of the abnormal parathyroids. They can also be useful in localizing ectopic or supernumerary glands in cases of reoperative surgery. Radiographic studies do not play a role in making the diagnosis of PHPT. Even patients with non-localizing imaging may benefit from consultation with an experienced parathyroid surgeon (1).
The most comprehensive parathyroid operation is bilateral four gland exploration where all 4 parathyroid glands are identified and a decision is made intraoperatively which gland or glands to remove. The cure rate for this procedure in experienced hands is greater than 95% (2). A focused approach is also used in certain cases with comparable results. A more limited dissection is used to excise an abnormal gland identified preoperatively on imaging. PTH levels are then drawn incrementally after excision. If certain criteria are met for decrease in PTH levels, the operation is either terminated or decision to proceed with 4 gland exploration is made (3).
Complications of parathyroid surgery are very low. Infection, bleeding requiring reoperation, vocal cord paralysis, and permanent hypoparathyroidism occur in less than 1% of cases. Surgery has also been found to be more cost-effective than observation and medical management. Outcomes of successful parathyroid surgery result in improvement in multiple end organ systems affected by PHPT (2). The following sections will discuss these effects in more detail.
Effects of parathyroid surgery on end organ systems
Successful parathyroid surgery leads to clinical improvement on several end organ systems. This has been shown and verified in multiple studies. The correction of elevated PTH levels leads to improvement in overall bone health. There is improvement in bone mineral density (BMD) as well as decreased incidence of fragility fractures. This is superior to medical management with bisphosphonates or calcimimetics (2). The incidence of kidney stones decreases after parathyroidectomy. The damage done to the renal parenchyma that results in a diminished glomerular filtration rate is not reversed, but reducing urinary excretion of calcium reduces further decline in renal function. Existing nephrocalcinosis is likewise not reversed with surgery (1,2).
There is no way to accurately quantify improvement in neurocognitive symptoms in the setting of PHPT. However, several studies examining quality of life indices demonstrate that patients exhibit less symptoms of fatigue, muscle pain and forgetfulness after parathyroidectomy (11). Other beneficial effects of successful parathyroid surgery include reduction in peptic ulcers as a result of decreased gastric acid secretion. As mentioned earlier, Vestergaard and colleagues found that patients who undergo parathyroidectomy exhibit a lower mortality rate from all causes than those treated conservatively (5).
Effects of parathyroid surgery on cardiovascular risk factors
In contrast to the robust body of data demonstrating the benefits of parathyroidectomy to bone and renal health, reports of improvements in the areas of cardiovascular disease are conflicting. Multiple studies show improvement in blood pressure, insulin resistance, vascular stiffness and cardiac morphology following successful surgery. However, the majority of these studies are retrospective and lack control groups. The few randomized controlled studies on the topic indicate that parathyroid surgery results in modest improvement of cardiac risk factors, if any at all (12).
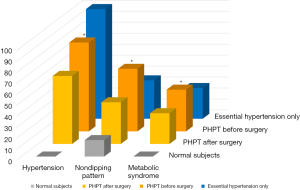
With regard to arterial hypertension in patients with PHPT, there is data suggesting improvement after parathyroidectomy (Figure 1). Luigi and colleagues conducted a prospective, controlled study comparing 3 groups of 30 patients each. The groups examined consisted of healthy subjects, patients with essential hypertension, and newly diagnosed PHPT. Each group was assessed for presence of metabolic syndrome, elevations in arterial blood pressure, including circadian alterations, and structural cardiac anomalies. All patients were re-evaluated 1 year after the hyperparathyroidism group underwent parathyroidectomy. Their results demonstrated statistically significant improvement in hypertension and decreased incidence of metabolic syndrome. However, structural cardiac parameters such as left ventricular thickness remained unchanged (13).
Several other studies show that parathyroidectomy may result in some improvement in cardiovascular risk factors such as arterial compliance, LVMI, and even overall risk of death. The previously mentioned large population-based study by Vestergaard and colleagues analyzed over 3,000 patients with PHPT who were either treated with surgery or by conservative means. Patients were followed over a 19-year period. They found that patients treated surgically had lower mortality rates, but their incidence of cardiovascular events and hypertension did not change significantly after surgery. Two other small studies demonstrated improvement in LVH after parathyroidectomy even though arterial blood pressure did not change (8,14). This supports the hypothesis that PTH itself may play a role in causing structural changes of the myocardium with or without the presence of coexisting hypertension. A recently described form of PHPT characterized by calcium levels in the normal range is also associated with the same cardiovascular risk factors as classical PHPT. There is data suggesting that patients with normocalcemic PHPT may exhibit higher risk of hypertension than those with hypercalcemia. More studies are needed to determine the role of surgery in mitigating the cardiovascular risk factors of this newer clinical entity (15).
Godang and colleagues conducted a randomized controlled trial with 5-year follow-up assessing the effects of parathyroidectomy on cholesterol levels, fasting glucose, fat distribution, and other markers of metabolic syndrome. They concluded that the surgically treated group exhibited higher vitamin D levels, while all other parameters remained unchanged when compared to the medically managed group (16). Another Scandinavian study corroborated these same results with a randomized controlled trial conducted over 2 years. Body mass index, glucose levels, insulin levels, inflammatory markers, and blood pressure did not differ significantly in the surgical or medically managed groups after 2 years (17).
Discussion
PHPT is a relatively common endocrine disorder that can have long term detrimental effects on multiple organ systems. There is ample data to suggest that the cardiovascular system is likewise affected by chronically elevated levels of PTH and calcium via still poorly understood mechanisms. Surgery remains the only treatment capable of definitively curing hyperparathyroidism. Surgical outcomes are excellent and complications are infrequent when performed by experienced parathyroid surgeons. There is strong evidence that successful parathyroid surgery can lead to improved bone density with a lower fracture risk, diminished incidence of kidney stones, improvement in peptic ulcer disease, and improvement in neurocognitive symptoms. To date, recommendations by professional endocrine and surgical societies do not include cardiovascular risk factors as an indication for parathyroid surgery. This seems fitting as the data tends to indicate that there is an association with hyperparathyroidism and cardiovascular risk factors such as hypertension and metabolic syndrome, but successful parathyroid surgery does not consistently lead to improvement. One possible explanation for this is that patients with PHPT and hypertension may have other underlying conditions contributing to their elevated blood pressure that are not treated with parathyroidectomy (7). Another possible explanation may be that structural and physiologic changes caused by chronically elevated PTH may become irreversible with time. More studies in this field are required to determine if earlier parathyroidectomy has more beneficial effect on blood pressure and cardiac outcome. At present, the few studies with promising data are not sufficient to advise parathyroid surgery in order to ameliorate cardiovascular risk alone. The association between parathyroid and cardiovascular diseases and finding possible remedies continue to be important topics for further investigation.
Conclusions
It is likely that PHPT indeed causes end-organ effects on the cardiovascular system, but it is challenging to discern when these effects are coincidental. While the number of published studies dedicated to this topic has increased over the last decade, there is much need for ongoing research. This includes determining with greater clarity and certainty whether parathyroidectomy in fact improves or even reverses some cardiovascular consequences such as hypertension, arterial calcification and metabolic syndrome.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Machado NN, Wilhelm S. Diagnosis and evaluation of primary hyperparathyroidism. Surg Clin N Am 2019;;99:649-66. [Crossref] [PubMed]
- Zhu CY, Nguyen D, Yeh M. Who benefits from treatment of primary hyperparathyroidism? Surg Clin N Am 2019;;99:667-79. [Crossref] [PubMed]
- Wilhelm SM, Wang T, Ruan D, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg 2016;151:959-68. [Crossref] [PubMed]
- Qin L, Raggatt L, Partridge N. Parathyroid hormone: a double-edged sword for bone metabolism. Trends Endocrinol Metab 2004;15:60-5. [Crossref] [PubMed]
- Vestergaard P, Mosekilde L. Cohort study on effects of parathyroid surgery on multiple outcomes in primary hyperparathyroidism. BMJ 2003;327:530-4. [Crossref] [PubMed]
- Pepe J, Cipriani C, Sonato C, et al. Cardiovascular manifestations of primary hyperparathyroidism: A Narrative Review. Eur J Endocrinol 2017;177:R297-308. [Crossref] [PubMed]
- Schiffl H, Lang S. Hypertension secondary to PHPT: Cause or coincidence? Int J Endocrinol 2011;2011:974647. [Crossref] [PubMed]
- Stefenelli T, Abela C, Frank H, et al. Cardiac abnormalities in patients with primary hyperparathyroidism: Implications for follow-up. J Clin Endocrinol Metab 1997;82:106-12. [Crossref] [PubMed]
- Walker MD, Fleischer T, Rundek D, et al. Carotid vascular abnormalities in primary hyperparathyroidism. J Clin Endocrinol Metab 2009;94:3849-56. [Crossref] [PubMed]
- Bilezikian JP, Brandi M, Eastell R, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the fourth international workshop. J Clin Endocrinol Metab 2014;99:3561-9. [Crossref] [PubMed]
- Pasieka JL, Parsons L, Jones J. The long-term benefit of parathyroidectomy in primary hyperparathyroidism: A 10- year prospective surgical outcome study. Surgery 2009;146:1006-13. [Crossref] [PubMed]
- Ejlsmark-Svensson H, Rolighed L, Rejnmark L. Effect of parathyroidectomy on cardiovascular risk factors in primary hyperparathyroidism: A randomized clinical trial. J Clin Endocrinol Metab 2019;104:3223-32. [Crossref] [PubMed]
- Luigi P, Chiara F, Laura Z, et al. Arterial hypertension, metabolic syndrome and subclinical cardiovascular organ damage in patients with asymptomatic primary hyperparathyroidism before and after parathyroidectomy: Preliminary results. Int J Endocrinol 2012;2012:408295. [Crossref] [PubMed]
- Almqvist EG, Bondeson A, Bondeson L, et al. Cardiac dysfunction in mild primary hyperparathyroidism assessed by radionuclide angiography and echocardiography before and after parathyroidectomy. Surgery 2002;132:1126-32. [Crossref] [PubMed]
- Chen G, Xue Y, Zhang Q, et al. Is normocalcemic primary hyperparathyroidism harmful or harmless? J Clin Endocrinol Metab 2015;100:2420-4. [Crossref] [PubMed]
- Godang K, Lundstam K, Mollerup C, et al. The effect of surgery on fat mass, lipid and glucose metabolism in mild primary hyperparathyroidism. Endocr Connect 2018;7:941-8. [Crossref] [PubMed]
- Bollerslev J, Rosen T, Mollerup C, et al. Effect of surgery on cardiovascular risk factors in mild primary hyperparathyroidism. J Clin Endocrinol Metab 2009;94:2255-61. [Crossref] [PubMed]



