The role of the physiotherapy in the plastic surgery patients after oncological breast surgery
Introduction
Breast cancer is the most insidious oncological disease in women all over the world, with an estimate of 1,152,161 new cases each year (1). The improvement of surgical techniques, neo adjuvant and adjuvant treatment enhance the survive time and recovery of these patients (2-6). As surgery has been the first choice for the treatment of breast neoplasm (3,5) reconstructive procedures became more request, helping to reconstruct the mutilation after a radical or conservatory breast treatment and enhance quality of live and physical function of these patients (7).
The most common modalities of reconstructive surgery are the use of expander and prosthesis based implants and the reconstruction using flaps tissues from other sites of the patient’s body (8). Both techniques are not risk free and sequelae like implant capsular contracture (9), swelling, pain, upper limp restriction (8), scar tissues and biomechanical muscular changes are not uncommon and sometimes are over evaluated and over treated.
As part of the rehabilitation regime, physiotherapy can assist in patient’s recovery after these reconstructive procedures, but the small number of specialized physiotherapy in the oncological field and lack of evidence based techniques reduce the trust of the multidisciplinary team in physiotherapy professional.
The objective of this article is to review the scientific literature and examine the available data regarding the role of the physiotherapy in patients underwent plastic reconstruction after oncological breast surgery.
Search strategy and selection criteria
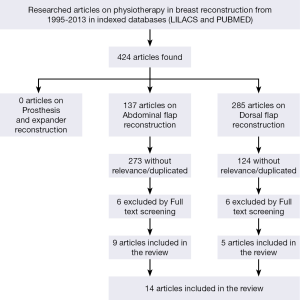
A literature search was carried in October 2013 to identify studies of where physiotherapy had an active role (in pre and post-surgery assessment and with rehabilitation protocols) after oncological breast reconstructive surgery. Our review was obtained by search the PubMed (National Library of Medicine, USA) and LILACS (Latin American and Caribbean Health Sciences) databases using the following search themes: “Physiotherapy and breast reconstructive surgery”, “physiotherapy and prosthesis breast reconstruction”, “physiotherapy and expander breast reconstruction”. For the flaps surgery the search themes were separate by the flaps donor site: “physiotherapy after dorsal flap breast reconstructive surgery”, “recovery After dorsal flap reconstructive surgery”, “rehabilitation after dorsal flap breast reconstruction”, “physiotherapy after abdominal flap breast reconstructive surgery”, “recovery after abdominal flap reconstructive surgery”, “rehabilitation after abdominal flap breast reconstruction”, “physiotherapy after DIEP flap breast reconstructive surgery”, “recovery after DIEP flap reconstructive surgery” and “rehabilitation after DIEP flap breast reconstruction”. In an attempt to minimize the omission of potentially relevant clinical studies, we also reviewed the reference lists of included studies and relevant reviews for additional eligible articles. The time of limit for our search was from 1995 until the present date. Only papers in English were cited. Publications and citations were selected with the remit of this review. The articles were selected according to each subheading purpose in the review.
Results
Fourteen articles were included in our review that matches our search criteria. The results are in Figure 1. Breast cancer surgery and reconstructive surgery can lead to post-surgical sequela and when surgery is concomitant, patients could be diagnosed with different kind of deficit of either axillary surgery or reconstructive surgery. These circumstances difficult the treatment and demand specialized physiotherapy and a multi and inter disciplinary team to manage and follow these patients.
Implant based reconstructive surgery
The implant-based reconstruction is the most common type of reconstruction after oncological breast surgery in many countries and institutions (7). In our clinical practice we are aware that oncological patients underwent reconstruction with expander or prosthesis have more difficult to start the rehabilitation protocol used for patients after breast surgery or axillary surgery without reconstruction, as the reconstruction could lead to more pain and restriction in range of motion of the upper limb (8). We recommend our patients who underwent these procedures to start a rehabilitation protocol in the first postoperative day. Patients and surgeons should be informed that most of exercises protocols found in literature are indicated to patients underwent breast or axillary surgery without concern in reconstruction (10).
After surgery, collateral effects like prosthesis encapsulation, post-surgery scar tissues, and breast edema are not infrequent (8,9). The indication of upper limb exercise and correction of postural antalgic position are advised. The use of massage therapy techniques, neuromuscular taping and manual lymphatic drainage are usual in the clinical practice, but there is a lack of protocols and studies that prove the efficacy in patients underwent oncological plastic surgery reconstruction with implants.
Autologous based reconstructive surgery
In patients who underwent autologous based reconstructive surgery, the evaluation should be made at preoperative day and that practice should be standard, to compare end evaluate the impairment and patients’ needs after surgery.
The post-operative evaluation should be executed in the range of 4 to 6 weeks. Postoperative condition of the patients and a correct communication between surgeon and physiotherapy should be taken in consideration prior to start any evaluation protocol. The use of the Kendall muscular evaluation (11) or manual muscle strength testing using the Medical Research Council (MRC) Scale (12) are broadly used by physiotherapist, but results tend to be subjective. We suggest the combination of digital dynamometers with the manual evaluation to give a more objective result (13). In literature the more used evaluation using an isokinetic machines (14-16), but they are expensive and most of institutions and physiotherapy have no access to this machinery.
Several studies showed that patients underwent bi-pedicle transverse rectus abdominis myocutaneous (TRAM) flap had a decrease in strength during flexion movement six weeks after surgery. Kind et al. showed the modification in patients underwent unilateral pedicle TRAM flap finding a compensatory rotational strength pattern on the contra lateral side of surgery (14-17). These muscular changes tend to recovery between the three and six months after surgery (16,17). There are no studies that linked the abdominal strength changes with lower or upper back problems, even if it is well know that abdominal muscles is intrinsically related with the stabilization of the human body (18).
Patients underwent latissimus dorsi flap reconstruction had a reduction of rotator cuff and extension force 6 weeks after surgery, with a recovery in 3-6 months (19-23). Nevertheless that recovery did not reach the base lines find in pre-operative evaluation as demonstrated in the study of Forthomme et al. (22).
A small number of studies were found about deep inferior epigastric perforators (DIEP) procedure. All of them showed little reduction of wall strength in the first weeks after surgery when compared with TRAM flaps reconstruction (15,24-26). Nevertheless, the indication of a correct posture after surgery should be given to all patients, as the pain and dyskinesia in the abdominal area could affect the correct imbalance in walk or execute daily activities in the first months. Patients who are more susceptible to venous congestion and fat necrosis (27) should be identified, so any rehabilitation procedure should be carefully discussed among the surgeon and patient.
The literature shows a small probability of embolic events or respiratory complications after TRAM and DIEP surgeries (28). Respiratory physiotherapy should be a concern in the first postoperative day as patients underwent breast reconstruction with abdominal flap tends to be long time in the operation room, bed immobilization and pain in abdominal area. The use of respiratory exercises can help prevent atelectasis and mucus mobilization and early ambulation deep venous thrombosis. Patients should be inform on how assume a correct posture, mobilization from bed to stand position, to walk, and seat (29,30). It’s important to correct any kind of antalgic position after surgery that could evoke muscular contractions and more pain.
As part of the assessment, a validated questionnaire (10,31) could be used to assess the results of the physiotherapy, quality of life and any emotional distress. The physiotherapy must collaborate with the multidisciplinary team, as the collateral effects of reconstructive surgery could be more than only mechanical or physical (32).
During our review, there were no studies regards exercises or postural education protocols aimed to patients underwent TRAM, DIEP or latissimus dorsi procedures. The suggestion of postural global reeducation (33,34), Pilates (35-37), CORE exercise (38) and upper limb exercise (10) could be part of the rehabilitation protocol but these techniques need to be studied and researched in patients underwent reconstructive surgery after breast cancer surgery.
Conclusions
Physiotherapy is a field that still needs evidence based in the daily routine and studies in the breast oncological physiotherapy field are warranted. Evaluation should be standardized. Rehabilitation techniques used are empirical and should be researched in patients underwent plastic reconstruction after breast surgery. The lack of post-surgery exercise protocols difficult the analyses of patient’s evolution and making challenging to prove the real role of the physiotherapy in this population.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol 2006;24:2137-50. [PubMed]
- Fisher B, Jeong JH, Anderson S, et al. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med 2002;347:567-75. [PubMed]
- Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 2011;305:569-75. [PubMed]
- Martelli G, Boracchi P, De Palo M, et al. A randomized trial comparing axillary dissection to no axillary dissection in older patients with T1N0 breast cancer: results after 5 years of follow-up. Ann Surg 2005;242:1-6; discussion 7-9. [PubMed]
- Sanghani M, Balk EM, Cady B. Impact of axillary lymph node dissection on breast cancer outcome in clinically node negative patients: a systematic review and meta-analysis. Cancer 2009;115:1613-20. [PubMed]
- Veronesi U, Orecchia R, Zurrida S, et al. Avoiding axillary dissection in breast cancer surgery: a randomized trial to assess the role of axillary radiotherapy. Ann Oncol 2005;16:383-8. [PubMed]
- Atisha D, Alderman AK, Lowery JC, et al. Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg 2008;247:1019-28. [PubMed]
- Hernandez-Boussard T, Zeidler K, Barzin A, et al. Breast reconstruction national trends and healthcare implications. Breast J 2013;19:463-9. [PubMed]
- Blount AL, Martin MD, Lineberry KD, et al. Capsular contracture rate in a low-risk population after primary augmentation mammaplasty. Aesthet Surg J 2013;33:516-21. [PubMed]
- Segal R, Evans W, Johnson D, et al. Structured exercise improves physical functioning in women with stages I and II breast cancer: results of a randomized controlled trial. J Clin Oncol 2001;19:657-65. [PubMed]
- Kendall FP, McCreary EK, Provance PG, et al. eds. Muscles: testing and function, with posture and pain. Lippincott Williams & Wilkins, 2005.
- Paternostro-Sluga T, Grim-Stieger M, Posch M, et al. Reliability and validity of the Medical Research Council (MRC) scale and a modified scale for testing muscle strength in patients with radial palsy. J Rehabil Med 2008;40:665-71. [PubMed]
- van der Linden ML, Aitchison AM, Hazlewood ME, et al. Test-Retest repeatability of gluteus maximus strength testing using a fixed digital dynamometer in children with cerebral palsy. Arch Phys Med Rehabil 2004;85:2058-63. [PubMed]
- Alderman AK, Kuzon WM Jr, Wilkins EG. A two-year prospective analysis of trunk function in TRAM breast reconstructions. Plast Reconstr Surg 2006;117:2131-8. [PubMed]
- Bonde CT, Lund H, Fridberg M, et al. Abdominal strength after breast reconstruction using a free abdominal flap. J Plast Reconstr Aesthet Surg 2007;60:519-23. [PubMed]
- Dulin WA, Avila RA, Verheyden CN, et al. Evaluation of abdominal wall strength after TRAM flap surgery. Plast Reconstr Surg 2004;113:1662-5; discussion 1666-7.
- Kind GM, Rademaker AW, Mustoe TA. Abdominal-wall recovery following TRAM flap: a functional outcome study. Plast Reconstr Surg 1997;99:417-28. [PubMed]
- Brown SH, Ward SR, Cook MS, et al. Architectural analysis of human abdominal wall muscles: implications for mechanical function. Spine (Phila Pa 1976) 2011;36:355-62. [PubMed]
- Button J, Scott J, Taghizadeh R, et al. Shoulder function following autologous latissimus dorsi breast reconstruction. A prospective three year observational study comparing quilting and non-quilting donor site techniques. J Plast Reconstr Aesthet Surg 2010;63:1505-12. [PubMed]
- de Oliveira RR, do Nascimento SL, Derchain SF, et al. Immediate breast reconstruction with a Latissimus dorsi flap has no detrimental effects on shoulder motion or postsurgical complications up to 1 year after surgery. Plast Reconstr Surg 2013;131:673e-80e. [PubMed]
- de Oliveira RR, Pinto e Silva MP, Gurgel MS, et al. Immediate breast reconstruction with transverse latissimus dorsi flap does not affect the short-term recovery of shoulder range of motion after mastectomy. Ann Plast Surg 2010;64:402-8. [PubMed]
- Forthomme B, Heymans O, Jacquemin D, et al. Shoulder function after latissimus dorsi transfer in breast reconstruction. Clin Physiol Funct Imaging 2010;30:406-12. [PubMed]
- Glassey N, Perks GB, McCulley SJ. A prospective assessment of shoulder morbidity and recovery time scales following latissimus dorsi breast reconstruction. Plast Reconstr Surg 2008;122:1334-40. [PubMed]
- Futter CM, Weiler-Mithoff E, Hagen S, et al. Do pre-operative abdominal exercises prevent post-operative donor site complications for women undergoing DIEP flap breast reconstruction? A two-centre, prospective randomised controlled trial. Br J Plast Surg 2003;56:674-83. [PubMed]
- Hamdi M, Weiler-Mithoff EM, Webster MH. Deep inferior epigastric perforator flap in breast reconstruction: experience with the first 50 flaps. Plast Reconstr Surg 1999;103:86-95. [PubMed]
- Futter CM, Webster MH, Hagen S, et al. A retrospective comparison of abdominal muscle strength following breast reconstruction with a free TRAM or DIEP flap. Br J Plast Surg 2000;53:578-83. [PubMed]
- Kroll SS. Fat necrosis in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg 2000;106:576-83. [PubMed]
- Monteiro M. Physical therapy implications following the TRAM procedure. Phys Ther 1997;77:765-70. [PubMed]
- Kalisch BJ, Lee S, Dabney BW. Outcomes of inpatient mobilization: a literature review. J Clin Nurs 2013. [Epub ahead of print]. [PubMed]
- Pasquina P, Tramèr MR, Granier JM, et al. Respiratory physiotherapy to prevent pulmonary complications after abdominal surgery: a systematic review. Chest 2006;130:1887-99. [PubMed]
- Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996;29:602-8. [PubMed]
- Qiu J, Chen W, Gao X, et al. A randomized controlled trial of group cognitive behavioral therapy for Chinese breast cancer patients with major depression. J Psychosom Obstet Gynaecol 2013;34:60-7. [PubMed]
- Bonetti F, Curti S, Mattioli S, et al. Effectiveness of a ‘Global Postural Reeducation’ program for persistent low back pain: a non-randomized controlled trial. BMC Musculoskelet Disord 2010;11:285. [PubMed]
- Moreno MA, Catai AM, Teodori RM, et al. Effect of a muscle stretching program using the Global Postural Reeducation method on respiratory muscle strength and thoracoabdominal mobility of sedentary young males. J Bras Pneumol 2007;33:679-86. [PubMed]
- Stan DL, Rausch SM, Sundt K, et al. Pilates for breast cancer survivors. Clin J Oncol Nurs 2012;16:131-41. [PubMed]
- Eyigor S, Karapolat H, Yesil H, et al. Effects of pilates exercises on functional capacity, flexibility, fatigue, depression and quality of life in female breast cancer patients: a randomized controlled study. Eur J Phys Rehabil Med 2010;46:481-7. [PubMed]
- Keays KS, Harris SR, Lucyshyn JM, et al. Effects of Pilates exercises on shoulder range of motion, pain, mood, and upper-extremity function in women living with breast cancer: a pilot study. Phys Ther 2008;88:494-510. [PubMed]
- Akuthota V, Ferreiro A, Moore T, et al. Core stability exercise principles. Curr Sports Med Rep 2008;7:39-44. [PubMed]