Nipple-areola complex reconstruction
Background
Patients with loss of the nipple and areola from cancer excision, trauma, or congenital absence continue to experience psychological distress even long after breast mound reconstruction has taken place. Other conditions requiring nipple areolar complex (NAC) reconstruction include congenital or developmental pathology (athelia, amastia), posttraumatic or burn deformities, and complications from breast surgery such as reduction mammaplasty. In the cases of breast cancer, whole breast reconstruction following mastectomy can provide significant psychosocial benefits for women. Nipple reconstruction can be performed with all types of breast reconstructive procedures and at any time following completion. Nipple reconstruction represents the simplest from a technical perspective but is among the most important from an aesthetic perspective (1).
Studies have shown that recreation of the NAC has a high correlation with overall patient satisfaction and acceptance of body image (2). Thus, completion of the breast reconstruction by creating a nipple-areola complex that matches the contralateral nipple in terms of size, shape, projection, and position adds significantly to the reconstructive result.
In this review, we concentrate only in general principles of NAC reconstruction and do not include any surgical techniques for NAC reconstruction. Readers can find relevant surgical techniques in various standard textbooks of plastic and reconstructive breast surgery.
History of the procedures
The history of nipple reconstruction parallels that of breast reconstruction with autologous tissue, from the development of the latissimus dorsi flap by Tanzini in 1906 to modern transverse rectus abdominis myocutaneous (TRAM) and microvascular-free TRAM breast reconstruction.
The evolution of NAC creation began when Adams initial description of the nipple-areola graft and labial graft in the 1940s (3,4). Following this, Millard proposed the nipple-sharing concept, where the contralateral nipple tissue was used as a composite graft for the reconstructed nipple (5). Later, various other grafts from toe pulp, auricular cartilage, and mucous membranes were also attempted and proven somewhat successful in providing tissue with projection, but at the expense of a significant donor site morbidity (6,7). A paradigm shift occurred in NAC reconstruction with the descriptions of the quadropod flap, dermal fat flap, and T-flaps in the 1980s (8-10). These flaps, based on smaller local flaps, allowed for rearrangement into a nipple configuration. In the 1980s and 1990s, multiple different local flaps were being described using the concepts of local flap rearrangement with and without skin grafts including the skate flap, star flap, CV flap, Bell flap, and the S-flap. Lastly, the increasing use of synthetic materials and allografts in reconstructive surgery has allowed for new, innovative methods for projection augmentation and revisional NAC reconstruction.
Various techniques of nipple reconstruction ensued, allowing use of transferred tissue and scar to form a nipple prominence. Among them are Little’s skate flap and its modifications, Anton and Hartrampf’s star flap and Bostwick’s C-V flap, Cronin’s S-flap, Smith and Nelson’s mushroom flap. Several studies looked at long-term projection of the various reconstructive techniques.
Various authors promoted their own techniques as being superior, but each has to decide which works best for himself. Becker was the first surgeon who introduced the tattooing technique for NAC reconstruction in 1986 (11). Spear popularized it in the years to follow (12). Currently, medical tattooing appliances are ubiquitous and of high quality and offer several tones and hues of pigment to match the color of the native areola. Some pigment fading over time is to be expected, and a few touch-up procedures may be required. Pigment fading was the most common long term complaint, voiced by up to 60%. A few required touch-ups and the majority were satisfied with their outcome.
Nipple reconstruction techniques have evolved significantly over the years. From simple tattooing to the more technologically advanced, although rarely available, tissue engineering, today’s techniques are able to provide long-lasting, satisfactory reconstruction with minimal morbidity (13).
Relevant anatomy of NAC
Nipple-areola anatomy is remarkably variable in dimension, texture, and color across ethnic groups and among individuals. Moreover, an appreciable difference often exists in the two nipple-areola complexes in the same patient. The presence of an elevated structure in the center of a pigmented area on the breast mound usually represents a nipple, yet wide variability exists as to what constitutes the normal dimensions of the complex.
The nipple areola complex is the primary landmark of the breast. As previously stated, it is located at the prominence of the breast mound. The nipple itself may project as much as ≥1 cm, with a diameter of approximately 4-7 mm. The areola consists of pigmented skin surrounding the nipple proper and is on average approximately 4.2-4.5 cm in diameter.
The central position of the nipple cylinder in the areola also has significant variability, ranging from one fourth to one half of the radius off-center. Nipple projection results from the primary location of the mammary ducts in the central portion of the nipple complex. This arrangement produces a semi-rigid structure with a significantly more fibrotic element than the soft and pliable surrounding areola. The contractile properties of the areola also contribute to the gradual change in nipple projection obtained with direct or neural stimuli.
General principles of NAC reconstruction planning
Ideal reconstruction of the NAC requires symmetry in position, size, shape, texture, and pigmentation and permanent projection. Generally, NAC reconstruction can be safely performed in an outpatient setting under local anaesthesia. The authors proposed the following suggestions general guidelines for the NAC reconstruction.
(I) NAC reconstruction is postponed till the final and stable setting of the reconstructed breast mound, optimally 3-4 months following breast reconstruction (14-17). Timing of NAC reconstruction is crucial to the final aesthetic result. Surgical decisions made too early may result in asymmetric placement of the nipple. Adjuvant therapies need to be taken into consideration as the tissue healing effects of radiation and chemotherapy may compromise final outcomes. The ideal timing for reconstruction is approximately 3-5 months after the last revisional reconstructive surgery. This allows for swelling and inflammation to subside, while allowing for settling of the reconstructed breast mound into its final position (18).
(II) In unilateral reconstruction, the contralateral NAC serves as a template.
(III) In bilateral reconstruction, the surgeon must make use of standard values to create a nipple position, size, and areola size. A review of 600 breasts showed that the mean diameter of the areola is approximately 4 cm, with average nipple diameter being 1.3 cm and the average nipple projection is 0.9 cm (19). The average nipple-areola and areola-breast proportion is approximately 1.3 cm (20).
(IV) Loss of projection of the reconstructed nipple should always be anticipated due to contraction, and overcorrection of 25-50% of the desired result is advisory in NAC reconstruction with local flaps.
(V) The type of previous breast reconstruction is another important factor to consider in patient selection. Patients who undergo prosthetic-based breast reconstruction will have a thin, expanded skin-subcutaneous tissue base, usually with a centrally placed mastectomy scar. On the other hand, in autologous reconstruction, patients will typically have a variable sized donor tissue skin paddle with an elliptical or circular shaped scar with a thick base. These factors are important in eventual NAC reconstruction as thin flaps can potentially decrease nipple projection and poorly located scars can prohibit the use of certain flap techniques due to interference with blood supply.
Classification of nipple reconstruction (according to techniques)
There are many innovative ways to create a NAC. Although many claim some methods are superior to others, each method has unique characteristics that apply to certain breast types (Table 1). In this section, multiple categories of reconstructive techniques will be explored, focusing on the desirable and undesirable aspects of each.
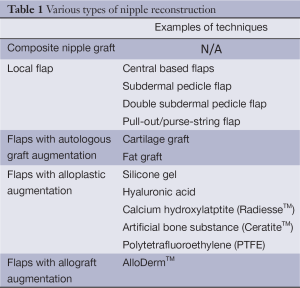
Full table
Composite nipple graft
Initiated by Adams in 1944 and described by Millard in 1972, contralateral nipple grafts have remained as a popular method for nipple reconstruction in patients with excess contralateral nipple projection (21,22). Patients with projection in excess of 5-6 mm are ideal candidates for composite nipple grafts (Figure 1). Many patients have reservations about this method of nipple reconstruction due to: (I) fear of contralateral surgery; (II) donor site morbidity; and (III) decreased contralateral nipple sensation.
Most patients decline to have surgery on the normal breast and NAC, and sharing is only used in selected cases such as hypertrophic contralateral nipple (Excellent option for patients with contralateral nipple >1 cm projection) or thin skin coverage in an alloplastic breast reconstruction (23). Banked nipple grafts for replantation is an alternative, however frequently lose pigmentation and produce variable aesthetic results (24), as cryopreservation causes severe damage to skin components of the nipple, which are seen when examined under electron microscopy (25).
Zenn et al. reviewed 57 patients who underwent composite nipple grafting. They found that only 47% of patients considered donor site sensation as “normal”, but found that 96% of patients were happy with the overall appearance, with 87% retaining erectile function in the donor nipple (26). In contrast, in the grafted nipple, the study found that 35% of patients had sensation in the reconstructed nipple within an average of six months. Interestingly, 42% of patients reported to having erectile function in the reconstructed nipple within an average of three months. In addition, they found complete graft take in both patients that had previous irradiation.
Composite nipple graft was excellent option for patients with contralateral nipple >1 cm projection and early postoperative discoloration is normal and expected.
Local flaps
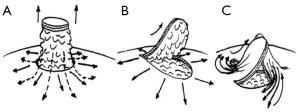
Local flaps for nipple reconstruction can be divided into three groups: centrally based flaps, subdermal pedicle and pull-out/purse-string flap techniques (Figure 2).
Of primary concern in nipple reconstruction is the creation of a long-lasting projection. This is influenced essentially by two factors: (I) retraction forces of surrounding and underlying tissues and (II) tissue contraction of the flap. The power of retraction forces significantly differ between centrally based and subdermal pedicle flaps. Centrally based flaps are subjected to the greatest retraction forces, which act on the entire base of the flap. In subdermal pedicle flaps these forces are significantly reduced, because the major part of the flap is freed from the underlying tissue and thus protected from retraction. Contraction, however, occurs to a variable degree in all local flaps, resulting in loss of flap volume and projection. Contracture of superficial scars adds to this effect. Flaps with complicated design are subjected to more scarring and contracture.
In addition, blood supply is an important determinant of flap shrinkage. Subdermal pedicle flaps are nourished through the rich subdermal plexus and thus have better blood supply compared to central core flaps, which depend on blood supply via the subcutaneous tissue. Scarring or irradiation can significantly compromise blood supply and, therefore, the final result of all flaps. Essential prerequisites to achieve a stable flap size are a wide pedicle, simple flap design, and separation from retractile surrounding tissues.
Local flap techniques have evolved significantly over the past years. Evolution was directed towards improving blood supply, minimizing retraction forces by simplification of flap design and by rejection of centrally based flap techniques. Enhanced vascularization was achieved by widening of the subdermal pedicle base and development of double-pedicled flaps (Figure 2).
One example of subdermal pedicle base flap which is popular amongst the surgeon is Star Flap. This flap has the advantage of eliminating skin graft donor site morbidity by allowing for primary closure and possibly an improved cosmetic result. On the other hand, the main disadvantages of the star flap are the lack of projection (27). Kroll et al. followed 47 patients who underwent star flap nipple reconstruction. He found that mean projection achieved was 1.97 mm after a 2-year follow-up (28). Few et al. used a modified star-dermal fat flap technique on 93 nipple reconstructions. They designed a flap with a blunted central wing and two opposing lateral triangles, or wings. The flap lengths directly correlated to the gain in projection. They found that 1 cm in flap length gave 0.16 cm in projection. In addition, long-term projection loss was 59% using their modification (1).
Shestak et al. used the star flap in patients with 29).
Modifications of the “Star Flap” is also widely used. These flaps can all be assigned to the category of star and wrap flaps (Figure 3). Some surgeons incorporated more subcutaneous fat in the lateral arms of the flap for additional nipple bulk. Wong et al. tattooed the whole area of the future areola 2-3 weeks before nipple reconstruction (30). Eskenazi tattooed the ‘star flap’ only with subsequent dissection of the flap and followed by tattooing of the corrected area of the areola. The flap base was varied as dictated by the direction of local scars.
Pull-out/purse-string flap technique is the last techniques for nipple reconstruction using local flap described in the review. The designs described in the following section represent unique methods to create nipple and/or areolar projection using surrounding tissue mobilization and purse-string techniques. These flaps are best used when the breast mound tissue is supple and able to be mobilized to enhance projection. The techniques include “Bell Flap”, “Double opposing peri-areolar/purse-string Flap” and “Top-hat Flap”.
Flaps with autologous graft augmentation
The concept of using autologous tissue for nipple augmentation is introduced in order to overcome the common problem of late flatting after reconstruction with local flap. The techniques include cartilage graft and fat graft.
Auricular cartilage was first advocated by Brent and Bostwick in 1977 as method to augment nipple reconstruction (31). This method was then modified by Tanabe et al. to be included within a dermal-fat flap to maintain projection (32). Some surgeons believe that the cartilaginous structure provides long lasting results with minimal loss of projection (33,34).
Costal cartilage grafts have been advocated by Guerra and colleagues in autologous breast reconstruction (35). They report successful use of the arrow flap in a large series of 454 patients in conjunction with a costal cartilage graft harvested and banked during the initial free flap reconstruction. Their group found a 4% cartilage graft loss attributed to local flap ischemia and infection. Despite these complications, long-term projection was maintained. Cheng et al. also described maintaining nipple projection in Asian females with the use of a modified top-hat flap in combination with costal cartilage banked at the initial flap inset (36). After long-term follow-up of 58 patients, they found an average of 26.1% projection loss after 45 months. In addition, they had a 12% complication rate, mostly related to partial flap loss, nipple malposition, and cartilage exposure (37).
Fat grafting has become an increasingly popular method as a surgical adjunct for soft tissue augmentation in all aspects of plastic surgery. Therefore, the use in nipple reconstruction seems to be a logical step in fat grafting utility. Bernard outlines steps for the use of fat grafting in primary and secondary nipple reconstruction (38).
In primary reconstruction, the proposed neo-nipple location is marked but not incised. Donor fat is harvesting from the abdominal or other donor region using Coleman aspiration cannulas. After concentrating the fat, 1 cc syringes are prepared and instilled into the proposed nipple site. Only 1-2 cc are needed and this process may be repeated in interval settings. After sufficient time passes to allow for partial fat resorption, the original flap is elevated and sutured into place. This technique may be useful in patients who have had tissue expansion leading to thinned dermis and subdermal fat.
Flaps with alloplastic augmentation
Alloplastic grafts have been used for nipple reconstruction to provide stable projection. The main disadvantage to using nonautologous tissue is the risk of infection and extrusion. Fillers can bleed into surrounding tissue and may interfere with oncologic surveillance. Some of the currently used materials include hyaluronic acid and calcium hydroxylapatite (39-41).
Hallock advocated the use of a polyurethane-coated silicone gel implant for nipple creation as a salvage-type procedure. The study reported the use of silicone implants for two nipple reconstructions with no reported capsule contracture at one year (42). This type of implant is only reserved for special cases and is rarely used today.
Evans et al. used RadiesseTM, injectable calcium hydroxylapatite embedded in a cellulose gel, to augment the reconstructed nipple. The gel scaffold allows for tissue ingrowth to aid in stability. The initial study included evaluation of six patients over an average of six months of follow-up. The average time from the original nipple reconstruction to the injection was 237 days. A majority of the group indicated major improvements to the appearance of the nipple and one patient reported a little decrease in projection. Overall, they found that all patients were satisfied with the use of RadiesseTM (39).
Hyaluronic acid is an attractive option for nipple projection augmentation. Panettiere et al. used this to augment nipple reconstruction and performed injections at 2, 4, and 7 months after nipple creation. Reliable projection was maintained at 12 months, but they found that one patient had a false-positive result on PET scan (40).
Yanaga et al. evaluated 100 patients who underwent nipple reconstruction with bilobed dermal flaps an skin graft with an artificial bone substance, CeratiteTM, at the center to provide projection. This group found maintained long-term projection with an average of 80.5% nipple height symmetry to the contralateral side. In addition, there was a 5% exposure rate, which was related to dermal flap tension (43).
Wong et al. used polytetrafluoroethylene (PTFE) as a method to create nipple projection. This method was utilized in selected patients: either is secondary reconstruction or when there was a lack of donor tissue for a local flap. A total of 17 patients underwent placement of PTFE into a subcutaneous pocket at the desired nipple location. An amount of 3.5 mm PTFE are used to create the initial desired projection with 3.0 mm pieces used for added contour. In the series, all patients were reported to be satisfied or very satisfied with their results. One patient had implant extrusion secondary to infection, but was later replaced after the infection subsided. Overall, they found projection of 4-5 mm (44).
Flaps with allograft augmentation
Acellular dermal allografts represent a new and revolutionary product in the field of breast reconstruction. After gaining wide acceptance for the use in implant-based reconstruction, the use of acellular dermis has expanded to all aspects of revisional and secondary breast reconstruction, including nipple reconstruction. Long term projection will likely have mild moderate projection loss.
Allografts have many of the ideal properties of an implantable material, as they have a high rate of incorporation with limited resorption. Because of the ability to incorporate into surrounding tissues, infection is limited.
Nahabedian first used AlloDermTM, human-derived acellular dermis, for revisional nipple reconstruction in 2005. A small piece (1 cm × 2 cm) of AlloDermTM is cut and folded upon itself and sutured in place with absorbable suture. The dimensions of the AlloDermTM piece were 2 mm × 6 mm. This piece is then oriented vertically to serve as a strut within the pocket made by the wings of the flap. Among the five secondary nipple reconstructions using AlloDermTM, four of the nipple exhibited 4-5 mm of maintained projection at follow-up, ranging six months to one year. In addition, tertiary nipple reconstruction with AlloDerm occurred in three patients. A total of 4-5 mm of projection was maintained in these patients as well at follow-up ranging from 6-8 months. AlloDermTM was incorporated into the base of the reconstructed nipple using the C-V flap or elongated C-flap (45).
Garramone and Lam evaluated the long-term nipple projection after using AlloDermTM in primary reconstruction. A total of 30 nipple reconstructions (16 implant-based breast mounds and 14 TRAM breast mounds) using a star dermal flap, were evaluated. In contrast to the previous technique, the AlloDermTM piece was cut into a strip measuring 1.5 cm × 4.5 cm. This piece was then rolled upon itself and sutured together. This then was secured into the pocket formed by the flaps. Among the 16 patients who had TRAM flaps, the average initial projection was 1.2 cm, with the average 12-month projection being 0.7 cm. In the implant-based group, the average initial projection was 1.15 cm and the 12-month average projection was 0.5 cm. Maintained projection after 12 months was 56% for the TRAM group and 47% for the implant group. Overall, the average maintained projection was 51.2% after 12 months follow-up (46).
Recently developed, the Cook medical nipple reconstruction cylinder is another good option for acellular dermal augmentation. This cylindrically shaped product is shaped perfectly to fit into a subcu-taneous pocket. This product eliminates the need to shape or roll acellular dermal products and eliminates any size discrepancies that would cause asymmetry.
Areola reconstruction
The major challenges of areola reconstruction are to recreate the pigmentation and texture typically associated with a native areola. The most commonly employed techniques involve using skin grafts, tattooing, and/or a combination of these two techniques. Also, the surgeon must choose an appropriate timing for the reconstruction. Skin grafting is preferentially performed in the immediate setting or at the time of nipple reconstruction. Tattooing usually occurs at 6-8 weeks after nipple reconstruction, but some have good results and advocate for simultaneous nipple creation and tattooing (47).
Skin grafting of the areola
Skin grafting of areola has the advantages of providing a textured, wrinkled surface and distinct pigment differences, both of which resemble a normal areola with Montgomery tubercles. Common donor sites for areola skin grafting include contralateral areola, inner thigh/groin region, revised/excess breast skin, or other body areas, where revisional surgery is needed. In addition, to avoid a donor site, the planned areola can be elevated and raised as a skin graft and re-placed into its original position (48).
Tattooing
Tattooing is the other major adjunct to areola reconstruction. Either used by itself or in conjunction with skin grafting, tattooing can provide excellent areolar color match with limited morbidity. Initially introduced by Rees (49) and Spear et al. (50) in 1975. Tattooing uses intradermal pigments, typically mixtures of iron and titanium oxide chosen from a color plate. These pigments are then electrically deposited revised/excess breast skin, or other body areas, where revisional surgery is needed.
In addition, to avoid a donor into the upper and mid-papillary dermis. Sterile technique is mandatory as disease and viral transmission is possible. Pigment placement too superficially will result in pigment extrusion and sloughing, while deeper placement leads to macrophage processing and removal, both resulting in early pigment fading (51).
In unilateral cases, colors should be chosen that are slightly more pigmented than the contralateral areola. Spear and Arias found that 9.5% of areolas needed touch ups for pigment fading and that 60% of all areolas were described as being too light during the study interval (52). Thus, many patients will likely need touch-up tattooing after several months or years to achieve an aesthetically symmetric color match.
After tattooing is performed, the area will usually undergo sloughing and crusting for 3-5 days. The area should be kept moist with bacitracin or other type of petroleum jelly and dressings should be changed daily. After this period, slight de-pigmentation may occur and many patients will require touch-ups in the next few months.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Few JW, Marcus JR, Casas LA, et al. Long-term predictable nipple projection following reconstruction. Plast Reconstr Surg 1999;104:1321-4. [PubMed]
- Evans KK, Rasko Y, Lenert J, et al. The use of calcium hydroxylapatite for nipple projection after failed nipple-areolar reconstruction: early results. Ann Plast Surg 2005;55:25-9; discussion 29. [PubMed]
- Adams WM. Free transplantation of the nipples and areola. Surgery 1944;15:186.
- Adams WM. Labial transplant for correction of loss of the nipple. Plast Reconstr Surg (1946) 1949;4:295-8. [PubMed]
- Millard DR Jr. Nipple and areola reconstruction by split-skin graft from the normal side. Plast Reconstr Surg 1972;50:350-3. [PubMed]
- Brent B, Bostwick J. Nipple-areola reconstruction with auricular tissues. Plast Reconstr Surg 1977;60:353-61. [PubMed]
- Klatsky SA, Manson PN. Toe pulp free grafts in nipple reconstruction. Plast Reconstr Surg 1981;68:245-8. [PubMed]
- Muruci A, Dantas JJ, Noguerira LR. Reconstruction of the nipple-areola complex. Plast Reconstr Surg 1978;61:558-60. [PubMed]
- Hartrampf CR Jr, Culbertson JH. A dermal-fat flap for nipple reconstruction. Plast Reconstr Surg 1984;73:982-6. [PubMed]
- Chang WH. Nipple reconstruction with a T flap. Plast Reconstr Surg 1984;73:140-3. [PubMed]
- Becker H. The use of intradermal tattoo to enhance the final result of nipple-areola reconstruction. Plast Reconstr Surg 1986;77:673-6. [PubMed]
- Spear SL, Convit R, Little JW 3rd. Intradermal tattoo as an adjunct to nipple-areola reconstruction. Plast Reconstr Surg 1989;83:907-11. [PubMed]
- Cao YL, Lach E, Kim TH, et al. Tissue-engineered nipple reconstruction. Plast Reconstr Surg 1998;102:2293-8. [PubMed]
- Bosch G, Ramirez M. Reconstruction of the nipple: a new technique. Plast Reconstr Surg 1984;73:977-81. [PubMed]
- Gruber RP. Nipple-areola reconstruction: a review of techniques. Clin Plast Surg 1979;6:71-83. [PubMed]
- Hartrampf CR Jr, Culbertson JH. A dermal-fat flap for nipple reconstruction. Plast Reconstr Surg 1984;73:982-6. [PubMed]
- Little JW 3rd. Nipple-areola reconstruction. Clin Plast Surg 1984;11:351-64. [PubMed]
- Nahabedian MY. Nipple reconstruction. Clin Plast Surg 2007;34:131-7. [PubMed]
- Sanuki J, Fukuma E, Uchida Y. Morphologic study of nipple-areola complex in 600 breasts. Aesthetic Plast Surg 2009;33:295-7. [PubMed]
- Hauben DJ, Adler N, Silfen R, et al. Breast-areola-nipple proportion. Ann Plast Surg 2003;50:510-3. [PubMed]
- Adams WM. Free transplantation of the nipples and areola. Surgery 1944;15:186.
- Millard DR Jr. Nipple and areola reconstruction by split-skin graft from the normal side. Plast Reconstr Surg 1972;50:350-3. [PubMed]
- Farhadi J, Maksvytyte GK, Schaefer DJ, et al. Reconstruction of the nipple-areola complex: an update. J Plast Reconstr Aesthet Surg 2006;59:40-53. [PubMed]
- Little JW. Cryopreserved autologous nipple-areola complex transfer to the reconstructed breast. Plast Reconstr Surg 2003;111:148.
- Nakagawa T, Yano K, Hosokawa K. Cryopreserved autologous nipple-areola complex transfer to the reconstructed breast. Plast Reconstr Surg 2003;111:141-7; discussion 148-9. [PubMed]
- Zenn MR, Garofalo JA. Unilateral nipple reconstruction with nipple sharing: time for a second look. Plast Reconstr Surg 2009;123:1648-53. [PubMed]
- Alfano C, Tenna S, Caggiati A, et al. Nipple reconstruction by local flaps: a long-term comparative study between star and skate techniques. Acta Chir Plast 2004;46:127-31. [PubMed]
- Kroll SS, Reece GP, Miller MJ, et al. Comparison of nipple projection with the modified double-opposing tab and star flaps. Plast Reconstr Surg 1997;99:1602-5. [PubMed]
- Shestak KC, Gabriel A, Landecker A, et al. Assessment of long-term nipple projection: a comparison of three techniques. Plast Reconstr Surg 2002;110:780-6. [PubMed]
- Wong RK, Banducci DR, Feldman S, et al. Pre-reconstruction tattooing eliminates the need for skin grafting in nipple areolar reconstruction. Plast Reconstr Surg 1993;92:547-9. [PubMed]
- Brent B, Bostwick J. Nipple-areola reconstruction with auricular tissues. Plast Reconstr Surg 1977;60:353-61. [PubMed]
- Tanabe HY, Tai Y, Kiyokawa K, et al. Nipple-areola reconstruction with a dermal-fat flap and rolled auricular cartilage. Plast Reconstr Surg 1997;100:431-8. [PubMed]
- Collis N, Garrido A. Maintenance of nipple projection using auricular cartilage. Plast Reconstr Surg 2000;105:2276-7. [PubMed]
- Norton S, Akhavani MA, Kang N. The ‘Hamburger’ technique for harvesting cartilage grafts in nipple reconstruction. J Plast Reconstr Aesthet Surg 2007;60:957-9. [PubMed]
- Guerra AB, Khoobehi K, Metzinger SE, et al. New technique for nipple areola reconstruction: arrow flap and rib cartilage graft for long-lasting nipple projection. Ann Plast Surg 2003;50:31-7. [PubMed]
- Cheng MH, Ho-Asjoe M, Wei FC, et al. Nipple reconstruction in Asian females using banked cartilage graft and modified top hat flap. Br J Plast Surg 2003;56:692-4. [PubMed]
- Cheng MH, Rodriguez ED, Smartt JM, et al. Nipple reconstruction using the modified top hat flap with banked costal cartilage graft: long-term follow-up in 58 patients. Ann Plast Surg 2007;59:621-8. [PubMed]
- Bernard RW, Beran SJ. Autologous fat graft in nipple reconstruction. Plast Reconstr Surg 2003;112:964-8. [PubMed]
- Evans KK, Rasko Y, Lenert J, et al. The use of calcium hydroxylapatite for nipple projection after failed nipple-areolar reconstruction: early results. Ann Plast Surg 2005;55:25-9; discussion 29. [PubMed]
- Panettiere P, Marchetti L, Accorsi D. Filler injection enhances the projection of the reconstructed nipple: an original easy technique. Aesthetic Plast Surg 2005;29:287-94. [PubMed]
- Lennox K, Beer KR. Nipple contouring with hyaluronics postmastectomy. J Drugs Dermatol 2007;6:1030-3. [PubMed]
- Hallock GG. Polyurethane nipple prosthesis. Ann Plast Surg 1990;24:80-5. [PubMed]
- Yanaga H. Nipple-areola reconstruction with a dermal-fat flap: technical improvement from rolled auricular cartilage to artificial bone. Plast Reconstr Surg 2003;112:1863-9. [PubMed]
- Wong RK, Wichterman L, Parson SD. Skin sparing nipple reconstruction with polytetrafluoroethylene implant. Ann Plast Surg 2008;61:256-8. [PubMed]
- Nahabedian MY. Secondary nipple reconstruction using local flaps and AlloDerm. Plast Reconstr Surg 2005;115:2056-61. [PubMed]
- Garramone CE, Lam B. Use of AlloDerm in primary nipple reconstruction to improve long-term nipple projection. Plast Reconstr Surg 2007;119:1663-8. [PubMed]
- Vandeweyer E. Simultaneous nipple and areola reconstruction: a review of 50 cases. Acta Chir Belg 2003;103:593-5. [PubMed]
- Chang BW, Slezak S, Goldberg NH. Technical modifications for on-site nipple-areola reconstruction. Ann Plast Surg 1992;28:277-80. [PubMed]
- Rees TD. Reconstruction of the breast areola by intradermal tattooing and transfer. Case report. Plast Reconstr Surg 1975;55:620-1. [PubMed]
- Spear SL, Convit R, Little JW 3rd. Intradermal tattoo as an adjunct to nipple-areola reconstruction. Plast Reconstr Surg 1989;83:907-11. [PubMed]
- Garg G, Thami GP. Micropigmentation: tattooing for medical purposes. Dermatol Surg 2005;31:928-31; discussion 931. [PubMed]
- Spear SL, Arias J. Long-term experience with nipple-areola tattooing. Ann Plast Surg 1995;35:232-6. [PubMed]




