The effect of neck dissection on quality of life in patients with differentiated thyroid cancer
Patients with differentiated thyroid cancer (DTC) have an excellent survival rate. As a general they also have a good prognosis. Cervical lymph node metastases occur in 30% to 80% of these and are associated with a significant probability for loco-regional recurrence of the disease, even in low-risk patients. This reflects in a rapid shift in patient care from a focus on overall survival to a focus on recurrence-free survival (1-3).
Tumor free survival has been the most important measure outcome recently, but nowdays it has been realized that the diagnosis and management of cancer can alter every aspect of the quality of life (QOL) of a patient. The main goal of cancer treatment became not only to increase survival but also to preserve QOL, which is considered to be of paramount importance (1,4,5).
Thus the effect of neck dissection on QOL in patients with DTC is a matter of question that has to be reviewed in two aspects.
- The first one is about the indications and extent of neck dissection in patients with DTC;
- The second is about the definition and measurement of QOL in these patients.
According to The American Thyroid Association (ATA) 2009 guidelines the aims of surgical treatment of DTC patients are as follows:
- To remove the primary tumor, disease that has extended beyond the thyroid capsule, and involved cervical lymph nodes. Completeness of surgical resection is an important determinant of outcome, while residual metastatic lymph nodes represent the most common site of disease persistence recurrence;
- To minimize treatment-related morbidity. The extent of surgery and the experience of the surgeon both play important roles in determining the risk of surgical complications;
- To permit accurate staging of the disease. Because disease staging can assist with initial prognostication, disease management, and follow-up strategies, accurate postoperative staging is a crucial element in the management of patients with DTC;
- To facilitate postoperative treatment with radioactive iodine, where appropriate. For patients undergoing RAI remnant ablation, or RAI treatment of residual or metastatic disease, removal of all normal thyroid tissue is an important element of initial surgery. Near total or total thyroidectomy also may reduce the risk for recurrence within the contralateral lobe;
- To permit accurate long-term surveillance for disease recurrence. Both RAI whole-body scanning (WBS) and measurement of serum Tg are affected by residual normal thyroid tissue. Where these approaches are utilized for long-term monitoring, near-total or total thyroidectomy is required;
- To minimize the risk of disease recurrence and metastatic spread. Adequate surgery is the most important treatment variable influencing prognosis, while radioactive iodine treatment, TSH suppression, and external beam irradiation each play adjunctive roles in at least some patients (6).
As a part of adequate surgery, neck dissection play important role for definitive treatment of the cancer. In 1991 a standardized classification of Academy’s Committee for Head and Neck Surgery and Oncology was published by Robbins et al. and was worldwide accepted (7).
This system is based on four concepts:
- Radical neck dissection (RND) is the standard basic procedure for cervical lymphadenectomy against which all other modifications are compared;
- Modifications of the RND which include preservation of any non-lymphatic structures are referred to as modified radical neck dissection (MRND);
- Any neck dissection that preserves one or more groups or levels of lymph nodes is referred to as a selective neck dissection (SND);
- An extended neck dissection refers to the removal of additional lymph node groups or non-lymphatic structures relative to the RND.
As a result of this conceptual approach is the Academy’s classification:
- RND;
- MRND;
- MRND Type I: excision of all lymph nodes routinely removed by radical neck dissection with preservation of the SAN;
- MRND Type II: excision of all lymph nodes routinely removed by radical neck dissection with preservation of the SAN and IJV;
- MRND Type III (functional or comprehensive neck dissection): excision of all lymph nodes routinely removed by radical neck dissection with preservation of the SAN, IJV and SCM.
- SND;
- Supra-omohyoid type;
- Lateral type;
- Posterolateral type;
- Anterior compartment type.
- Extended radical neck dissection.
Due to location of thyroid gland and its lymphatic drainage the first affected lymph nodes are situated in the anterior compartment. In some cases various groups of nodes could be involved.
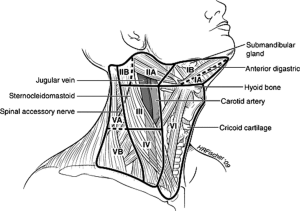
On Figure 1 is presented division of regional neck nodes according to Memorial Sloan-Kettering Cancer Center. It is well visible that anterior compartment and level VI represent the same anatomical region.
But what is the definition of anterior compartment dissection? Which are the anatomic boundaries of anterior compartment? By the Academy’s Committee for Head and Neck Surgery and Oncology the definition of SND Anterior Compartment is: En bloc removal of lymph structures in Level VI including:
- Perithyroidal nodes;
- Pretracheal nodes;
- Precricoid nodes (Delphian);
- Paratracheal nodes along recurrent nerves.
Gradoni et al. emphasize on the location of the thyroid gland which is low in the neck near the thoracic inlet, the lymphatic drainage is contiguous with the anterior superior mediastinum that is accessible via a cervical approach. As a result, the inferior border of the central compartment is defined as the innominate artery on the right and the corresponding axial plane on the left. In terms of Robbins levels, it means that the central neck dissection (CND) should include the VI and VII levels (8).
So the SND anterior compartment type including level VІ, VІІ is equal to so called CND.
In order to better understand complicated terminology in indications of neck dissection I will clarify some of the names most frequently met in the literature. Routine, elective or prophylactic neck dissection. All the terms mean the same—a neck dissection implies that nodal metastasis is not detected clinically or by imaging (clinically N0) pND. Therapeutic neck dissection—a therapeutic neck dissection implies that nodal metastasis is apparent clinically (preoperatively or intraoperatively) or by imaging (clinically N1a) tND (9).
What the guidelines say about the indications and extent of neck dissection in DTC patients?
The ATA guidelines [2009] state that tCND should be offered to clinical N+ patients. In patients with clinically uninvolved lymph nodes, ipsilateral or bilateral pCND may be performed, especially for advanced primary tumours (T3 or T4). It is recognized that for patients with small, noninvasive tumors, the balance of risk and benefit may favour simple near-total thyroidectomy with close inspection of the central compartement with compartmental dissection only in the presence of obviously involved lymph nodes. The level of this recommendation is an expert opinion based one.
Lymph nodes in the lateral neck (compartments II-IV) and posterior triangle (compartment V) may also be involved by DTC. For those patients in whom nodal disease is evident clinically, on preoperative ultrasound, or at the time of surgery, surgical resection may reduce the risk of recurrence and possibly mortality. Functional compartmental en-bloc dissection is favored over selective dissection (berry picking) with limited data suggesting improved mortality. Lateral neck compartmental lymph node dissection should be performed for patients with biopsy-proven metastatic cervical lymphadenopathy detected clinically or by imaging, especially when they are likely to fail radioactive iodine treatment based on lymph node size, number, or other factors, such as aggressive histology of the primary tumor. The recommendation is based on fair evidence that the service or intervention can improve important health outcomes (6).
According to the National Comprehensive Cancer Network guidelines (NCCN v.1.2010) compartment oriented neck dissection has to be performed when lymph nodes are palpable or biopsy positive. If the nodes are negative, prophylactic CND can be considered but is not required in all cases. Features that could call for prophylactic CND are: age <15 and >45; radiation history; known distant metastasis; extrathyroidal extension; tumour >4 cm in diameter and aggressive hystological variant. The recommendation expressed is based on lower-level evidence and there is nonuniform NCCN consensus but no major disagreement (10).
In the British Thyroid Association guidelines (BTA, 2007) is said that in patients with clinically uninvolved nodes but who are deemed high risk (i.e., they have any of the following features: male sex, age >45 years, tumours greater than 4 cm in diameter, extracapsular or extrathyroidal disease), pCND should be performed.
Palpable disease in level VI nodes discovered at surgery is treated by a tCND. When suspicious/clinically involved nodes are apparent pre-operatively or are encountered at surgery in the lateral neck, and confirmed by needle biopsy or frozen section, then a therapeutic SND (levels IIa-Vb) is recommended, preserving the accessory nerve, sternocleidomastoid muscle and internal jugular vein. The recommendation is based on evidence obtained from expert committee reports or opinions and/or clinical experience of respected authorities (11).
The European consensus for the management of differentiated thyroid carcinoma endorsed by the European Thyroid Association in 2006 state that lymph nodes dissections should be performed in patients with pre-operative or intra-operative diagnosis of lymph nodes metastases. The benefits of prophylactic CND is deemed controversial. According to this task force, there is no evidence that the prophylactic CND improves recurrence or mortality rates, but it allows an accurate staging of the disease that may guide subsequent treatment and follow-up (12).
According to Latin American Thyroid Society recommendations, pCND should be considered only for those patients with T3 or T4 and is not warranted in all patients. If at the time of surgery there is obvious metastatic disease in the jugular chain or lateral neck, modified neck dissection with removal of the lymph nodes at levels II, III, IV, and V is generally recommended. Modified neck dissection for thyroid carcinoma preserves all the important structures, such as the sternomastoid muscle, internal jugular vein, and accessory nerve, along with the submandibular salivary gland. The panel does not recommend the pCND in all patients with diagnosis of papillary thyroid cancer; however, it is deserved for any patient with a T3 or T4 (13).
There is no definitive clear statement about the indication and extent of neck dissection in patients with DTC. Summarizing published guidelines I can say that clinically evident lymph nodes metastasis require CND or MRND ІІа-Vв—both therapeutic. Prophylactic MRND is definitely not recommended, till prophylactic CND is preserved for T3, T4 patients with perineural, extracapsular invasion and it is yet deemed controversial. Hence we have to look for the effect of CND or MRND on QOL of the patients.
The second aspect of review is to clarify the definition and measurement of the QOL
Definition given by WHO—QOL 1993 designate QOL as the perceptions of an individual regarding his or her position in life in the context of the culture and value systems in which he or she lives and in relation to his or her goals, expectations, standards, and concerns (14).
Health related quality of life (HR-QOL) has some specifics and it refers to a multidimensional concept that encompasses perception of negative and positive aspects of physical, emotional, social, and cognitive functions, which could be affected by the disease or its treatment (15).
There are increasing number of studies measured QOL as an end point in the evaluation of the effect of the disease and its treatment on the daily life of the patient (5).
However, there have been relatively few HR-QOL studies looking specifically at patients with thyroid cancer (4,5,15) and only one specifically looking for the effect of neck dissection in such a patients (16).
How the neck dissection could affect the QOL of patients and how it could be measured?
Neck dissection could directly affect the QOL of patients by means of postoperative morbidity. There are several structures in the neck put in risk of damage during the procedure. Even in experienced hands neck dissection is associated with increasing incidence of major complications. The complication rate increases as the cervical LND range become more radical (17).
Complications most frequently met in both type of dissection are as follows: hypoparathyroidism, recurrent laryngeal nerves palsy, thoracic duct injury, spinal accessory nerve damage, transection of cervical rootlets, seroma, and wound infection.
Postoperative hypoparathyroidism
Transient hypoparathyroidism is the complication most frequently met after total thyroidectomy and neck dissection. Its incidence could rise up to 24% of the cases especially in bilateral procedures (18).
Roh et al. demonstrated no difference in incidental parathyroidectomy in patients with or without neck dissection after total thyroidectomy, but postoperative hypoparathyroidism was significantly higher in the neck dissection group than those with no dissection (19).
Their study found that increased hypoparathyroidism appeared not to be associated with incidental removal of the parathyroid glands or the number of parathyroid glands preserved during surgery. In addition, selective parathyroid autotransplantation did not appear to solve this problem since, despite more frequent use of this procedure in the node dissection group, a lot of patients experienced permanent hypocalcemia (19).
There is no significant difference between complication in CND or MRND (20). Prevention of permanent hypoparathyroidism is based on parathyroid autotransplantation in sternocleidomastoid muscle. Autotransplantation is a procedure deserved for any devascularized gland. Confirmation of parathyroid gland nature by frozen section is of great importance due to its potential misidentification with metastatic lymph node. Total thyroidectomy and neck dissection include considerable dissection in the paratracheal area, especially along the recurrent laryngeal nerve. This has a direct implication in a higher incidence of nerve injury and injury to the parathyroid glands, leading to temporary or permanent hypoparathyroidism (21).
Recurrent laryngeal nerve palsy
Injury of the recurrent laryngeal nerves is a severe complication that requires artificial airway secure in bilateral cases. The nerves are at risk in both CND and MRND. Although RLN palsy could be met it total thyroidectomy alone, authors reported as much incidence of this complication as more surgery is performed (20,22).
In the study of Malgorzata Wierzbicka et al. investigating morbidity of secondary neck dissections in thyroid cancer metastases, in 15.7% of the cases permanent vocal cord paresis was observed; in 5.9% tracheotomy had to be maintained (23).
On the other hand in article of Henry et al. concerning recurrent laryngeal nerve palsies in patients with total thyroidectomy alone and with pCND in one stage, there was no difference between the two groups of patients. This has been reported in other series and it confirms that the dissection of the nerve is no more dangerous during a total thyroidectomy associated with pCND than during a total thyroidectomy alone (24).
Prevention is generally associated with anatomical identification and confirmation of functional integrity of the nerves by the help of magnifying glasses and intraoperative neuromonitoring (25,26).
Thoracic duct injury
Thoracic duct, usually runs into the posterior mediastinum, generally opens up at the junction of the left jugular vein and subclavian vein. Cleaning of nodal metastasis at level IV in thyroid carcinoma may lead to injury of the lymphatic structures. This is manifested by chyle leak. Sometimes, it may be manifested postoperatively as large amount of chylous fluid into the drainage system. In these cases, a conservative approach with observation, pressure dressings, a fat free diet or potentially total parenteral nutrition is successful in most patients. Injection of tetracycline or other sclerosing agents has been proposed by some authors, but may lead to considerable scarring and fibrosis, inflammatory reaction, and pain (27).
If a chyle leak is identified at the time of surgery, it should be corrected by ligation of nonabsorbable ties, silk or prolene, or with hemoclips (28).
Neck anesthesia/neuropathic pain/decreased shoulder mobility
Yatrogenic damage of the cervical rootlets or injury of the spinal accessory nerve during neck dissection may lead to neck sensory abnormality (anesthesia, numbness, and/or neuropathic pain), edema and limitation of neck/shoulder movement, decline in speech and eating abilities. These complications usually are observed following MRND and may alter daily activities, social function, and professional performance. Varying degrees of dysfunction of the spinal accessory nerve are common after level V dissection even with nerve preservation. Indeed, even after complete nerve preservation, shoulder pain has been observed in 79% of patients after radical neck dissection, 65% of patients after MRND and 52% of patients after SND (29,30).
This is due to neuropraxia, caused by excessive traction, extensive dissection and skeletonization, devascularization and ischemia, thermal injury, blunt trauma during dissection, leading to degeneration of the upper trapezius and sternocleidomastoid muscles (31).
Instruments used to measure HR-QOL in patients with DTC are the same as these used in patients with head and neck cancer. Interesting is the fact that investigators of HR-QOL in head and neck cancer patients exclude from theirs research, patients with DTC because of its biologic behavior and specific treatment.
There are limited numbers of data in the literature about the measurement of HR-QOL in DTC patients with neck dissection. The paucity of specific instruments to assess the QOL of patients with thyroid cancer associated with low mortality and morbidity rates of the treatment can explain why there are so few studies in this field.
Validated instruments most widely used for finding clinical predictors of QOL in such a patient are Neck Dissection Impairment Index (NDII), Constant Shoulder Scale, and University of Washington Quality of Life questionnaire (UW-QOL).
NDII was developed and validated by Rodney J. Taylor et al. in 2002 in order to identify the factors that affect QOL following neck dissection due to head and neck cancer (32).
Reliability of the index was evaluated with test-retest correlation and internal consistency using the Cronbach α coefficient. Convergent validity was assessed using the 36-Item Short-Form Health Survey (SF-36) and the Constant Shoulder Scale, a shoulder function test. They used multiple variable regressions to determine variables that most affected QOL following neck dissection.
There is recent survey of Lee J et al. that compare oncological outcomes and QOL after robotic versus conventional open thyroidectomy with MRND in patients with papillary thyroid carcinoma and lateral neck node metastases (16).
They used arm abduction tests and questions from NDII and concluded that the robot technique was associated with improved QOL, including excellent cosmetic results and reductions in neck sensory changes and swallowing discomfort after surgery (16).
UW-QOL questionnaire is a validated, accurate, and internationally accepted survey instrument. In the original description, Hassan and Weymuller stated that ‘the advantages of the UW-QOL head and neck questionnaire are that (I) it is brief and self-administered; (II) it is multi-factorial, allowing sufficient detail to identify subtle change; (III) it provides questions specific to head and neck cancer; and (IV) it allows no input from the health provider, thus reflecting the QOL as indicated by the patient (33).
The current version 4 of the UW-QOL questionnaire consists of 12 single question domains, these having between three and six response options that are scaled evenly from 0 (worst) to 100 (best) according to the hierarchy of response. The domains are pain, appearance, activity, recreation, swallowing, chewing, speech, shoulder, taste, saliva, mood and anxiety. Another question asks patients to choose up to three of these domains that have been the most important to them. There are also three global questions, one about how patients feel relative to before they developed their cancer, one about their health-related QOL and one about their overall QOL. In regard to their overall QOL patients are asked to consider not only physical & mental health, but also many other factors, such as family, friends, spirituality or personal leisure activities that were important to their enjoyment of life.
In the study of Almeida J et al. there is some data about the clinical predictors of HR-QOL in DTC patients. According to their investigation the main factor that affects QOL of patients is RIT treatment. There is no significant data about the neck dissection as a clinical predictor (34).
Another study that evaluated the results of the adverse effects of surgery and RIT on such patients is a work of Dagan T et al. (35).
This study used an UW-QOL questionnaire that was adapted but not validated. The authors evaluated 20 patients with thyroid cancer and reported that those older than 45 years had worse general health, appearance, and chewing scores but did not show an association of RIT or neck dissection with any domain.
As a conclusion I would say that neck dissection affect the QOL of patients with DTC on two ways: positive and negative.
The positive way is correlated with appropriate neck dissection as a procedure of great importance to achieve the main goals of surgical therapy in patients with DTC.
The negative way is associated with higher risk and greater incidence of postoperative complications as main clinical predictors of impaired QOL of such a patient. Due to limited number of studies and lack of statistically correct data about the effect of neck dissection on QOL of patient with DTC, I recommend following the instructions of worldwide accepted guidelines (ATA, ETA, BTA, and LATG) regarding the indications and extent of neck dissection in DTC patients.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Tan LG, Nan L, Thumboo J, Sundram F, et al. Health-related quality of life in thyroid cancer survivors. Laryngoscope 2007;117:507-10. [PubMed]
- Myers EN. eds. Cancer of the head and neck, 4th ed. Philadelphia, PA: Saunders, 2003:850.
- Cooper DS, Doherty GM, Haugen BR, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2006;16:109-42. [PubMed]
- Huang SM, Lee CH, Chien LY, et al. Postoperative quality of life among patients with thyroid cancer. J Adv Nurs 2004;47:492-9. [PubMed]
- Vartanian JG, Carvalho AL, Yueh B, et al. Long-term quality-of-life evaluation after head and neck cancer treatment in a developing country. Arch Otolaryngol Head Neck Surg 2004;130:1209-13. [PubMed]
- American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, Cooper DS, Doherty GM, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167-214. [PubMed]
- Robbins KT, Medina JE, Wolfe GT, et al. Standardizing neck dissection terminology. Official report of the Academy’s Committee for Head and Neck Surgery and Oncology. Arch Otolaryngol Head Neck Surg 1991;117:601-5. [PubMed]
- Gradoni P, Giordano D, Oretti G, et al. Prophylactic central neck dissection for papillary thyroid carcinoma: the terms of the debate. Acta Biomed 2011;82:14-9. [PubMed]
- American Thyroid Association Surgery Working Group, American Association of Endocrine Surgeons, American Academy of Otolaryngology-Head and Neck Surgery, et al. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid 2009;19:1153-8. [PubMed]
- Available online: www.nccn.org
- British Thyroid Association, Royal College of Physicians. Guidelines for the management of thyroid cancer. Perros P, ed. 2nd edition. Report of the Thyroid Cancer Guidelines Update Group. London: Royal College of Physicians, 2007.
- Pacini F, Schlumberger M, Dralle H, et al. European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol 2006;154:787-803. [PubMed]
- Pitoia F, Ward L, Wohllk N, et al. Recommendations of the Latin American Thyroid Society on diagnosis and management of differentiated thyroid cancer. Arq Bras Endocrinol Metabol 2009;53:884-7. [PubMed]
- Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Qual Life Res 1993;2:153-9. [PubMed]
- Crevenna R, Zettinig G, Keilani M, et al. Quality of Life in patients with non-metastatic differentiated thyroid Cancer under thyroxine supplementation therapy. Support Care Cancer 2003;11:597-603. [PubMed]
- Lee J, Kwon IS, Bae EH, et al. Comparative analysis of oncological outcomes and quality of life after robotic versus conventional open thyroidectomy with modified radical neck dissection in patients with papillary thyroid carcinoma and lateral neck node metastases. J Clin Endocrinol Metab 2013;98:2701-8. [PubMed]
- Sakorafas GH, Sampanis D, Safioleas M. Cervical lymph node dissection in papillary thyroid Cancer: current trends, persisting controversies, and unclarified uncertainties. Surg Oncol 2010;19:e57-70. [PubMed]
- Cheah WK, Arici C, Ituarte PH, et al. Complications of neck dissection for thyroid cancer. World J Surg 2002;26:1013-6. [PubMed]
- Roh JL, Park JY, Park CI. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg 2007;245:604-10. [PubMed]
- Palestini N, Borasi A, Cestino L, et al. Is central neck dissection a safe procedure in the treatment of papillary thyroid cancer? Our experience. Langenbecks Arch Surg 2008;393:693-8. [PubMed]
- Shaha AR. Complications of neck dissection for thyroid cancer. Ann Surg Oncol 2008;15:397-9. [PubMed]
- Mazzaferri EL, Doherty GM, Steward DL. The pros and cons of prophylactic central compartment lymph node dissection for papillary thyroid carcinoma. Thyroid 2009;19:683-9. [PubMed]
- Wierzbicka M, Gurgul E, Wasniewska-Okupniak E, et al. The feasibility and efficacy of secondary neck dissections in thyroid cancer metastases. Eur Arch Otorhinolaryngol 2013. [Epub ahead of print]. [PubMed]
- Henry JF, Gramatica L, Denizot A, et al. Morbidity of prophylactic lymph node dissection in the central neck area in patients with papillary thyroid carcinoma. Langenbecks Arch Surg 1998;383:167-9. [PubMed]
- Kim MK, Mandel SH, Baloch Z, et al. Morbidity following central compartment reoperation for recurrent or persistent thyroid cancer. Arch Otolaryngol Head Neck Surg 2004;130:1214-6. [PubMed]
- Dimov RS, Deenichin GP, Damianliev RA, et al. Safety and efficacy of modified radical lymph nodes dissection in patients with papillary thyroid cancer and clinically evident lymph nodes metastasis. Folia Med (Plovdiv) 2006;48:17-22. [PubMed]
- Shaha AR. Complications of neck dissection for thyroid cancer. Ann Surg Oncol 2008;15:397-9. [PubMed]
- Roh JL, Kim DH, Park CI. Prospective identification of chyle leakage in patients undergoing lateral neck dissection for metastatic thyroid cancer. Ann Surg Oncol 2008;15:424-9. [PubMed]
- Dijkstra PU, van Wilgen PC, Buijs RP, et al. Incidence of shoulder pain after neck dissection: a clinical explorative study for risk factors. Head Neck 2001;23:947-53. [PubMed]
- Cheng PT, Hao SP, Lin YH, et al. Objective comparison of shoulder dysfunction after three neck dissection techniques. Ann Otol Rhinol Laryngol 2000;109:761-6. [PubMed]
- Kupferman ME, Weinstock YE, Santillan AA, et al. Predictors of level V metastasis in well-differentiated thyroid cancer. Head Neck 2008;30:1469-74. [PubMed]
- Taylor RJ, Chepeha JC, Teknos TN, et al. Development and validation of the neck dissection impairment index: a quality of life measure. Arch Otolaryngol Head Neck Surg 2002;128:44-9. [PubMed]
- Hassan SJ, Weymuller EA Jr. Assessment of quality of life in head and neck cancer patients. Head Neck 1993;15:485-96. [PubMed]
- Almeida JP, Vartanian JG, Kowalski LP. Clinical predictors of quality of life in patients with initial differentiated thyroid cancers. Arch Otolaryngol Head Neck Surg 2009;135:342-6. [PubMed]
- Dagan T, Bedrin L, Horowitz Z, et al. Quality of Life of well-differentiated thyroid carcinoma patients. J Laryngol Otol 2004;118:537-42. [PubMed]


