
Efficacy of continuous neuromonitoring in thyroid surgery: preliminary report of a single-center experience
IntroductionOther Section
The identification and dissection of the recurrent laryngeal nerve (RLN) in thyroid surgery prove to be the only safe method of protecting it from operative injury (1). RLN visualization is considered the gold standard for preventing RLN injury during thyroid surgery (1). Since the introduction of intraoperative neural monitoring in thyroid surgery, by Shedd and Durham in 1965 (2), technology has considerably improved, in particular over the past decade (3). The recent introduction of continuous intraoperative neuromonitoring (CIONM) seems to represent a significant step forward, potentially enabling the surgeon to react before the RLN is irreversibly damaged. Continuous neuromonitoring allows a closer monitoring of the functionality of the RLN. Its aim is to overcome the main methodological limitation of intermittent intraoperative neuromonitoring (IIONM), which can identify malfunction of the RLN only after the occurrence of the nerve damage (4,5). The CIONM technique permits identification of electromyography (EMG) changes, heralding imminent RLN injury, enabling the surgeon to promptly initiate corrective action for preserving the functional integrity of the nerve, by reversing the surgical maneuver associated with these early but adverse EMG changes (6). In order to proceed with continuous vagal monitoring, it is most important to place the endotracheal tube (TET) thoroughly and to expose a segment of the vagus nerve longer than 1 centimeter, so as to correctly position the automatic periodic stimulation (APS) electrode (3). Electrode installation on the vagus nerve is not so technically straightforward. The success of these surgical maneuvers is not to be taken for granted; therefore, this is a technique that requires the hands of experienced surgeons. If this new technique is potentially beneficial in some surgical situations, it is crucial to learn in detail its procedure, which differs significantly from that of the intermittent monitoring. Actually, there are no comparative studies in literature focused on the continuous intraoperative neuromonitoring vs. traditional procedure without neural monitoring: all studies available in scientific literature evaluate and compare both intermittent and continuous nerve monitoring together or describe their experience about the technique. In light of these considerations, the aim of our research is to evaluate the efficacy of CIONM during thyroid surgery, analyzing its impact on functional outcomes, in comparison with traditional surgical procedures.
MethodsOther Section
The study was conducted between January and December 2016 at the Endocrine Surgery Division of Fondazione Policlinico “A. Gemelli” after review and authorization by the Ethics Committee. Patients were initiated in one procedure or another according to the order in the operating room list. The CIONM technique was performed by using the commercially available NIM-response 3.0 nerve monitoring system while patients initiated in traditional technique did not use any devices.
Informed consent was obtained from each patient. All patients underwent preoperative and postoperative otorhinolaryngologist evaluation, laryngoscopy was performed in order to identify possible lesions, or alterations of the preoperative motility. Exclusion criteria were: patients with preoperative vocal cord injuries, patients aged below 18 years, patients with reoperation for postoperative hemorrhage. RLN palsy was defined as the presence of hoarseness or loss of voice quality associated with vocal cord paralysis at laryngoscopy.
Postoperative evaluation was conducted on patients with clinical alterations of voice quality and/or breath threatening and/or swallowing difficulties within 24 hours of surgery. The follow-up of this patient was conducted at the otolaryngology outpatient department, with the first check-up conducted 2 weeks after discharge.
RLN palsy was defined as transient if vocal cord motility was proved normal by laryngoscopy within 6 months from surgery. After this time, RLN palsy was considered permanent. All patients were operated on by a consultant surgeon and surgery was performed under general anesthesia.
Patients’ demographics, EMG signals and clinical findings were tabulated and analysed retrospectively.
CIONM technique
Anesthesia
Cooperation between surgeon and anesthesiologist was the key for successful neuromonitoring.
In the CIONM group, we used polarizing agents in order to reduce the dose of neuroblocking drugs (succinylcholine, or rocuronium, or cisatracurium), and shorten their half-life. In this group, patients were intubated under 0.1 mg per kg body weight for short acting intravenous neuroblocking. We did not use local anaesthetic gel or cream to lubricate the tube, but only physiological solution. TET (Medtronic Xomed) was inserted under visual control, to ensure the proper placement of the recording surface electrode at the level of the vocal cord, and TET size was established by the anesthesiologist, according to the patient’s conformation.
We preferred the larger size tube for a better contact with vocal cords and we kept the tube in the midline and fixed it with tape and cotton roll. Indeed, the correct positioning of the tube is vital to achieve a good EMG response.
Operation course
The device was NIM-Response 3.0 (Medtronic Xomed, Jacksonville, Florida, USA), with continuous monitoring by automated periodic stimulation (APS), delivering impulses of 100 µs and 1 mA, using 2 or 3 mm vagus electrodes. For the correct installation of the APS electrode, the exposure of a segment about 1 cm long of the vagus nerve was required; after its connection, the amplitude and latency of the baseline electromyogram (EMG) were determined as the mean values on 20 stimulations. We defined amplitude and latency changes as defined by the International Neural Monitoring Study Group (3).
Statistical analysis
The sample was described through means, standard deviations, minimum and maximum values when continuous quantitative variables were considered, and absolute and relative frequencies when qualitative variables were taken into account. Chi-square test was used to compare patients who underwent CIONM and those who did not, with respect to qualitative variables. The t-test was used to compare the mean age of the two groups. Because of the lack of randomization, exposure to the intervention might be influenced by some baseline characteristics independently related to the outcome. Therefore, the propensity score was used to control for confounding. The latter uses a model that allows showing the tendency of receiving an intervention, rather than the other, considering only variables measured at the baseline. Baseline variables considered in the logistic model used for developing the propensity score were: gender, age, diabetes, smoking, professional use of voice, reintervention, type of disease (carcinoma vs. non-carcinoma). Pairs of patients undergoing CIONM and traditional surgical operation were 1:1 matched according to the propensity score. A logistic regression model was run in order to evaluate the impact of CIONM as compared to standard approach on RLN palsy. Results were reported as odds ratio (OR) with 95% confidence interval (95% CI). Statistical analysis was carried out through STATA/SPSS and the P value was set at 0.05.
ResultsOther Section
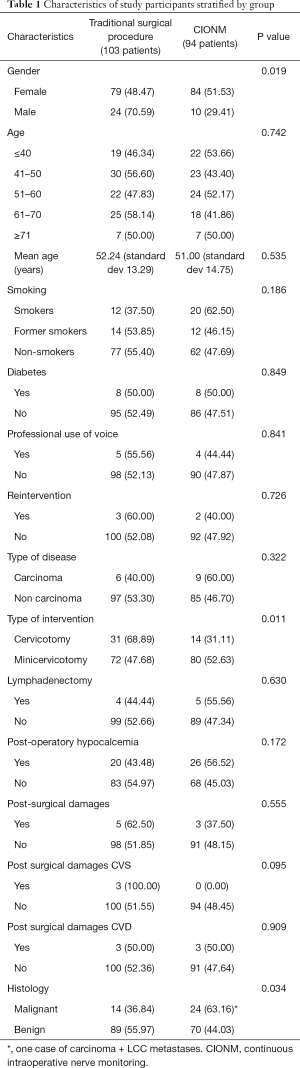
Baseline characteristics of the pre-matching population
In this study, 197 patients were enrolled: 34 males (17.3%) and 163 (82.7%) females. The mean age of the whole sample was 51.7 (SD 14.0; minimum 19; maximum 84). A total of 94 patients underwent CIONM, while 103 controls underwent the traditional surgical procedure. Table 1 shows the differences between CIONM and traditional surgical procedure groups. A total of 8 patients (4.1%) showed mild hypomobility damage [3 (3.2%) and 5 (4.9%) patients respectively in CIONM and traditional surgical procedure] to left or right vocal cords. Only 1 patient (0.5%), who was submitted to the traditional surgical procedure, showed a severe damage with paresis of both left and right vocal cords. As shown in Table 1, the two groups did not show any difference except for gender, type of intervention and type of disease. On the contrary, males were more commonly submitted to traditional surgical procedure as compared to females. Similarly, cervicotomy was performed more frequently in case of traditional monitoring and benign diseases were more commonly managed with this type of approach.
Full table
Propensity score-matched analysis
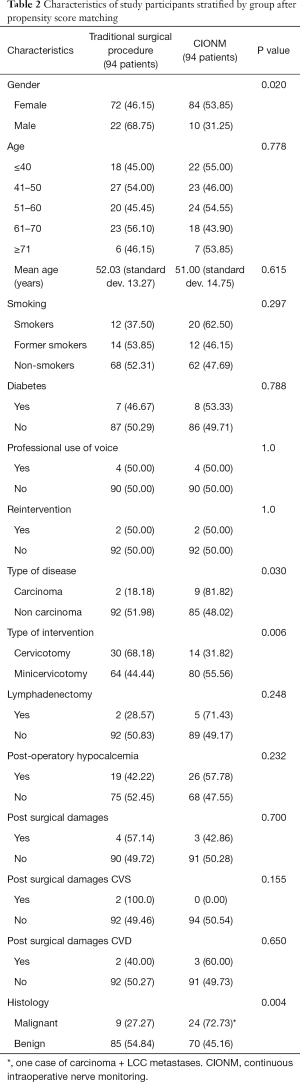
After matching for propensity score, 188 patients, 94 for each group, were considered. Nine patients, all of whom underwent traditional surgical procedure, were excluded from the analysis. Table 2 shows the differences between CIONM and traditional surgical procedure groups after propensity score matching.
Full table
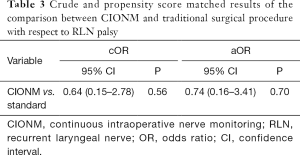
A total of 7 patients (3.7%) out of 188 patients showed mild hypomobility damage [3 (3.2%) and 4 (4.3%) patients respectively in CIONM and traditional surgical procedure] to left or right vocal cords. In the matched population, no patient showed a severe damaged with paralysis to both CVS and CVD. No associations were found between CIONM and damage of vocal cords, neither at the crude nor after propensity-score matching (Table 3).
Full table
DiscussionOther Section
The results of our investigation show that there is no significant difference between the use of CIONM and the traditional surgical procedure in reducing the rate of RLN injuries in thyroid surgery. On the grounds of the present analysis, no association was found between CIONM and vocal cord damage, neither at the crude nor at the adjusted, propensity-score matched, analyses. In our data, a total of 8 patients with transient damage to vocal cords were recorded, 3 in the CIONM group, and 5 in the traditional surgery group. No permanent vocal cord palsy was observed in the CIONM group. With regard to the three cases reported in the CIONM group, in two of them we lost the signal on vagus nerve at the end of the surgery, yet without any dislodgement of the APS electrode during surgery. In the other case, the APS electrode dislodged once. In the traditional surgery group, we recorded 5 cases of vocal cord injury, of the four cases of transient damage two patients had multifocal carcinoma at the definitive histological examination; the other two cases had a voluminous cervical goiter, but all patients had thyroiditis as an underlying condition. However, postoperative laryngoscopy showed a deficit of the vocal cord in abduction. Only one patient, submitted to the traditional surgical procedure, showed severe damage of both vocal cords, with permanent vocal fold palsy. This patient had a multifocal non-encapsulated cancer infiltrating the right RLN. CIONM significantly improved, compared to intermittent intraoperative neural monitoring as device and as intraoperative surgical procedure (3,7,8). In fact, it includes an additional step for the positioning of the APS electrode on the vagus nerve; being CIONM a new technique, it requires a learning curve, unlike IIONM (9). The skillful use of CIONM requires experience; the APS electrode is not very easy to place, and it requires the meticulous dissection of the vagus nerve, without causing any stretching or traction injury (10). Currently, there are no papers that describe experience and management of the possible complications that may occur in installing the APS electrode. In their own series, Phelan et al. (6) did not have any case of intraoperative cardiac, pulmonary, or gastrointestinal adverse events. They reported an average electrode installation time of 21 seconds, and 7 seconds for removal. Among our 94 patients enrolled in the CIONM group, 3 cases of intraoperative bradycardia were recorded during the placement of the APS electrode; therefore, it was necessary to stop the procedure for a few moments. For an optimal placement, after careful dissection of the carotid sheath, the surgeon must access the vagus nerve, circumferentially expose the nerve by ~8 mm along its length, avoiding the dissection of arterial and venous blood supply while preparing the course, and then attach to the drape using clip, wire and adjust the position of the clip by sliding it along the wire, if needed. Furthermore, the key to success is a close collaboration between the surgeon and the anesthesiologist for a correct endotracheal tube positioning, which can affect the EMG signal (11-13). A survey carried out by the AAES in 2006 underlined that, currently, the adoption of the intraoperative RLN monitoring is mostly used in centers with a high flow centers and above all by experienced surgeons (14). In high flow centers, in fact, the percentage of surgical interventions with greater complexity, could define “relatively selected” surveys, requiring an increased adoption of intraoperative RLN monitoring. In our experience, all patients were operated by consultant surgeons, each of whom with an annual operating volume of over 100 thyroid resections. Although CIONM is currently the most important monitoring technique in thyroid surgery, in our study no benefit was found. Different publications in the international literature appraised the role of selective intraoperative monitoring in case of oncologic thyroid surgery, with possible cervical lymph node dissection, autoimmune pathology, of voluminous cervical goiters and/or with mediastinal extension, of reoperations or surgery after cervical radiation (15,16). In the present analysis, we report the preliminary experience of our single center, where all patients with thyroid disease, without distinction between benign and malignant diseases, were enrolled. However, the analyzed population is small indeed, and this may represent a limit to our study as well as the lack of randomization. Nonetheless, with this respect, we have used the propensity score in order to make an unbiased comparison between groups but is should be observed that the power of our study remain very low and that larger studies should be performed in order to better investigate if CIOMN may be reduce the rate of RLN in comparison to traditional approach. The strong point of our investigation was the high level of standardization of the intraoperative neuromonitoring procedure, data collection and rigorous pre- and post-operative controls in all patients.
ConclusionsOther Section
The results of our research show no difference between the use of CONM and of traditional surgical procedures in reducing the rate of RLN injuries. Indeed, further research is required to validate the present findings, by using larger surgical populations. Multicenter studies, or studies that focus on a specific population (such as neoplastic disease), are needed.
AcknowledgmentsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards (ID 7001/14). Informed consent was obtained from all individual participants included in the study.
ReferencesOther Section
- Riddell V. Thyroidectomy: prevention of bilateral recurrent nerve palsy. Results of identification of the nerve over 23 consecutive years (1946-69) with a description of an additional safety measure. Br J Surg 1970;57:1-11. [Crossref] [PubMed]
- Shedd DP, Durham C. Electrical identification of the recurrent laryngeal nerve. I. Response of the canine larynx to electrical stimulation of the recurrent laryngeal nerve. Ann Surg 1966;163:47-50. [Crossref] [PubMed]
- Randolph GW, Dralle H. International Intraoperative Monitoring Study Group, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 2011;121 Suppl 1:S1-16. [Crossref] [PubMed]
- Lombardi CP, Carnassale G, Damiani G, et al. The final countdown": Is intraoperative, intermittent neuromonitoring really useful in preventing permanent nerve palsy? Evidence from a meta-analysis. Surgery 2016;160:1693-706. [Crossref] [PubMed]
- Chiang FY, Lu IC, Kuo WR, et al. The mechanism of recurrent laryngeal nerve injury during thyroid surgery—the application of intraoperative neuromonitoring. Surgery 2008;143:743-9. [Crossref] [PubMed]
- Phelan E, Schneider R, Lorenz K, et al. Continuous vagal IONM prevents recurrent laryngeal nerve paralysis by revealing initial EMG changes of impending neuropraxic injury: a prospective, multicenter study. Laryngoscope 2014;124:1498-505. [Crossref] [PubMed]
- Schneider R, Przybyl J, Pliquett U, et al. A new vagal anchor electrode for real-time monitoring of the recurrent laryngeal nerve. Am J Surg 2010;199:507-14. [Crossref] [PubMed]
- Jonas J. Continuous vagal nerve stimulation for recurrent laryngeal nerve protection in thyroid surgery. Eur Surg Res 2010;44:185-91. [Crossref] [PubMed]
- Dionigi G, Bacuzzi A, Boni L, et al. What is the learning curve for intraoperative neuromonitoring in thyroid surgery? Int J Surg 2008;6 Suppl 1:S7-12. [Crossref] [PubMed]
- Seddon HJ. A Classification of Nerve Injuries. Br Med J 1942;2:237-9. [Crossref] [PubMed]
- Lu IC, Chu KS, Tsai CJ, et al. Optimal depth of NIM EMG endotracheal tube for intraoperative neuromonitoring of the recurrent laryngeal nerve during thyroidectomy. World J Surg 2008;32:1935-9. [Crossref] [PubMed]
- Chu KS, Wu SH, Lu IC, et al. Feasibility of intraoperative neuromonitoring during thyroid surgery after administration of nondepolarizing neuromuscular blocking agents. World J Surg 2009;33:1408-13. [Crossref] [PubMed]
- Schneider R, Sekulla C, Machens A, et al. Postoperative vocal fold palsy in patients undergoing thyroid surgery with continuous or intermittent nerve monitoring. Br J Surg 2015;102:1380-7. [Crossref] [PubMed]
- Sturgeon C, Sturgeon T, Angelos P. Neuromonitoring in thyroid surgery: attitudes, usage patterns, and predictors of use among endocrine surgeons. World J Surg 2009;33:417-25. [Crossref] [PubMed]
- Chan WF, Lang BH, Lo CY. The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery 2006;140:866-72. [Crossref] [PubMed]
- Wu C, Dionigi G, Barczynski M, et al. International Neuromonitoring Study Group Guidelines 2018: Part II: Optimal Recurrent Laryngeal Nerve Management for Invasiv Thyroid Cancer—Incorporation of Surgical, Laryngeal, and Neural Electrophysiologic Data. Laryngoscope 2018;128:S18-27. [Crossref] [PubMed]


