The use of Patient Reported Outcome Measures in assessing patient outcomes when comparing autologous to alloplastic breast reconstruction: a systematic review
Introduction
Breast reconstruction surgery after mastectomy early on was demonstrated to have positive psychological benefits through improved cosmetic results and perceived body image (1-6), and is reflected in the number of patients undergoing the procedure, rising from 26.94% of patients after mastectomy in 2005, to 43.30% in 2014 (7). Most of this is attributable to implant and expander-based reconstruction, with the rate of free flaps only increasing from 1.25% to 3.96% in this time period (7). As therapies such as targeted chemotherapy have improved, breast cancer patients have higher survival rates.
Although the literature reports improved long-term durability, reduced reconstructive failure and surgical site infection using autologous tissue (8), with shorter recovery period without donor-site morbidity for implant-based reconstruction (6,9), there has been a lack of focus on patient focused outcomes. There is now an emphasis on Value Based Health Care (VBHC), which focusses on outcomes, both short and long term, that are important to the patient, and can be measured by Patient Reported Outcome Measures (PROMs) (10,11). Defined as measurement of any of a patient’s health status that comes directly from the patient, it has been incorporated as an independent parameter for health outcomes in conjunction with clinical outcome measurements (12,13). To date, there has been no systematic review to analyse PROMs between those undergoing autologous or alloplastic reconstruction, using validated measurement tools, to determine if there is a preferred technique from the patient’s perspective.
Materials and methods
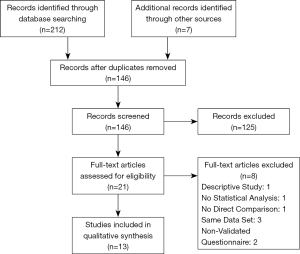
This manuscript analyses the current literature on PROMs with regards to autologous and alloplastic breast reconstruction in accordance with PRISMA guidelines (Figure 1). We performed a systematic search on EMBASE from 1947 until January 2019 to identify all English literature using keywords: “patient reported outcome” and “autologous”/“alloplastic” and “breast”, “patient reported outcome” and “implant”/“expander” and “breast”. We also identified relevant articles through bibliographic linkage. Two reviewers inspected the title and abstract of each citation to identify manuscripts suitable for review, with concordant papers included for review. Abstracts for conferences, letters to the editor and review articles were excluded from review.
Cohort studies reporting PROMs in female mastectomy patients undergoing autologous or alloplastic reconstruction using validated assessment tools were considered eligible. Case report and case series where statistical analysis was not performed were excluded from further consideration.
In total, 146 articles were screened after removal of duplicates. Following article appraisal, 13 articles were included in the systematic review (Figure 1). Excluded articles included those that did not use a validated questionnaire that would make objective comparison between studies difficult, did not provide numerical values or statistical analysis between the autologous and implant groups, or were studies based on the same data set, analyzed prospectively. Of the studies based on the same data set being analyzed prospectively, the article analyzing data across the entire study period was chosen.
Results
Demographics of included studies
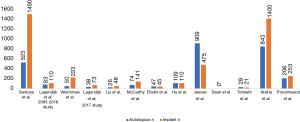
In total, 13 articles were included in the systematic review (Figure 1). Of the studies that discriminated patients been autologous and alloplastic reconstruction, a larger proportion of patients in the studies included underwent alloplastic reconstruction (n=4,389) when compared to those undergoing autologous reconstruction (n=2,937) (Figure 2).
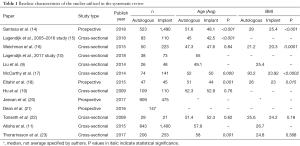
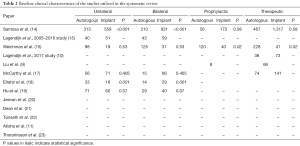
There was a preponderance for patients undergoing autologous reconstruction in the respective studies to be older than those who had implant-based reconstruction, and this was often statistically significant (Tables 1,2). This trend continued into studies that analyzed BMI, with those undergoing autologous reconstruction often having statistically significant higher BMI than those undergoing implant-based reconstruction.
Full table
Full table
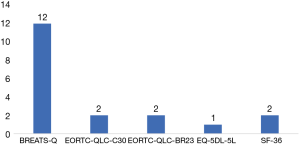
Most studies did not differentiate between type of autologous reconstruction performed in their analysis, with only two papers analyzing reported PROMs between latissimus dorsi (LD), pedicle and/or free transverse rectus abdominis muscle (TRAM) flap and deep inferior epigastric perforator (DIEP) flap (20,23). One study focused exclusively on autologous TRAM flap reconstruction (19), and one on DIEP flap reconstruction (22). For studies using validated PROMs used to gauge mastectomy patients, a significant proportion utilized the BREAST-Q study (Figure 3).
PROMs
BREAST-Q
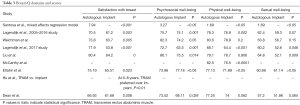
Satisfaction with breast
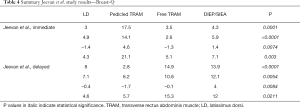
All studies utilizing BREAST-Q reported statistically significant increases in ‘satisfaction with breast’ with autologous when compared to implant reconstruction. Even after mixed-effects regression analysis by Santosa et al. (24), the increase was still statistically significant. Hu et al. (19) reported that TRAM reconstruction was preferred over implant in this regard. Jeevan et al. (20) noted statistically significant increases with those undergoing immediate LD, pedicled and free TRAM, DIEP and SIEA flaps when compared to implant-based reconstruction. This was apparent in both those that underwent immediate and delayed reconstruction. Atisha et al. (11) noted through regression analysis that abdominal and gluteal/thigh based autologous reconstruction had statistically significant increase in satisfaction with breast (Tables 3,4).
Full table
Full table
Psychosocial well-being
Most studies (9,14,15,20,21,25) reported statistically significant increases in psychosocial well-being with autologous reconstruction when comparing to implant reconstruction. On analysis of autologous flap choice, Jeevan et al. noted statistically significant increases with those undergoing immediate LD, pedicled and free TRAM, DIEP and SIEA flaps when compared to implant-based reconstruction. This was apparent in both those that underwent immediate and delayed reconstruction (Table 3,4).
Physical well-being
Half (14,15,17,25) of the studies reported statistically significant increases in physical well-being with autologous reconstruction when comparing to implant reconstruction. Jeevan et al. (20) notes that although pedicled TRAM and DIEP/SIEA patients scored higher, those undergoing immediate LD and free TRAM rated their physical well-being worse than those undergoing implant reconstruction. If the reconstruction was delayed, all but those undergoing DIEP/SIEA flaps rated their physical well-being worse than implant-based reconstruction (Tables 3,4).
Sexual well-being
Only 3 studies (9,14,20) reported statistically significant increases. Jeevan et al. (20) reported that regardless of immediate or delayed reconstruction, LD, pedicled, free TRAM and DIEP/SIEA flap patients reported statistically significant increases when compared to implant-based reconstruction (Tables 3,4).
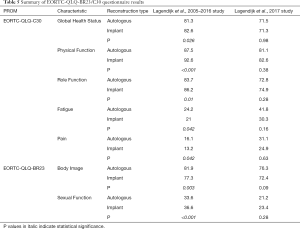
EORTC-QLQ-BR23/C30
Two articles by the same lead author (15,25) found that ‘Physical Function’ for those who underwent implant-based reconstruction was higher than those who underwent autologous reconstruction, however was only statistically significant in one of the two studies. The same trend was noted in the ‘Role Function’ domain of the survey. No difference was detected with regards to ‘Fatigue’ and ‘Pain’ between the two reconstructive groups. A similar trend was noted regarding ‘Sexual Function’. However, no statistically significant difference was noted regarding ‘Body Image’ between the two reconstructive groups (Table 5).
Full table
SF-36
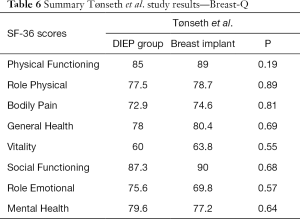
Two articles (22,23) used SF-36 questionnaires, with both noting no statistically significant difference in Physical Functioning, Bodily Pain, General Health, Social Functional or Mental Health between autologous or alloplastic reconstructive methods. One of the two studies identified a statistically significant increase in ‘Vitality’ when comparing expander-based reconstructions over DIEP flap-based reconstructions (Table 6).
Full table
Discussion
With the increasing number of reconstructive options available to the patient and surgeon, and increasing survival rates of breast cancer patients, there is now an increasing number of factors outside of the surgical domain to consider for the surgeon when counseling the patient (26). This is complicated by the statistically significant heterogeneity of patients presenting, as evidenced by the baseline variables that were different between the two groups of patients analyzed (Tables 1,2).
However, the literature is still lacking when analyzing PROMs for patients who develop complications from either autologous or alloplastic reconstruction, and was a population of patients which were excluded from most studies analyzed in this systematic review.
The BREAST-Q is a newly developed PROM questionnaire that has been validated for patients undergoing breast reconstruction to enable measurement of quality of life (QoL) and satisfaction in this population of patients (27,28). This is in comparison to EORTC QLQ-C30 and QLQ-BR23, which although are validated PROMs, are not specific for breast reconstruction. QLQ-C30 is a cancer specific health-related QoL questionnaire analyzing domains such as physical, emotional, cognitive, social functioning and sequelae of disease such as pain, nausea and fatigue, while QLQ-BR23 is a PROM validated for breast cancer patients, assessing factors such as body image, sexual functioning and enjoyment, cancer symptoms and systemic therapy side effects (29). SF-36 is a questionnaire that measures health on eight QoL domains including functional status, wellbeing and overall evaluation of health in the general population (30). This may explain why only differences between the two groups were detected by cancer specific PROMs, and only then, the results were equivocal, with only the breast-reconstruction specific BREAST-Q detecting differences between the two reconstructive techniques in some domains. This suggests that breast and reconstructive surgeons are treating a particular subset of patients that differ from other cancers, and whose perceptions and preferences for treatment are not adequately captured by the usual methods of determining what is important health-related QoL factors.
It is apparent that physical well-being is not significantly affected by reconstructive method, likely reflecting the fact that in the hands of a competent surgeon, alloplastic and autologous reconstruction are associated with low morbidity.
However, psychosocial well-being and satisfaction with breast are higher in autologous reconstruction compared to implant-based reconstruction, possibly due to implants not behaving like native tissue due to its synthetic nature, and unlike augmentation where normal breast tissue remains, the implant is now expected to replace the space previously occupied by normal tissue. Being an important secondary sexual organ, this new breast may not feel natural to the patient, and hence leading to the reduced psychosocial well-being and satisfaction with the breast when compared with autologous tissue.
A limitation of this study was primarily due to the selection process of the studies analyzed, that being patients who had complications from reconstruction were in most cases excluded from the studies. Complications developed by the patient may lead to one reconstructive technique being favored over the other, something that can be conveyed to the patient, allowing for a more informed decision. Furthermore, several studies did not include subgroup analysis of autologous or alloplastic reconstruction type, hence may under or overstate the true effects reported.
Another limitation was in relation to patient numbers in each study. Only the largest study (14) consisting of 2,013 patients was able to detect statistical significance in all domains of the PROM used. It is possible other studies were not powered adequately to detect these differences.
Conclusions
Undergoing breast reconstruction after mastectomy has been demonstrated to be associated with positive psychological outcomes. When comparing autologous and alloplastic-based reconstruction, it is apparent from the patient perspective that autologous reconstruction is no less favorable, and in fact has a higher satisfaction of breast rate than alloplastic reconstruction techniques. Physical and sexual well-being were equivocal between the two reconstructive groups. This knowledge can be utilized by the surgeon to help council patients so they can develop a more informed individual perception, aiding in decision making and subsequently improved QoL.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Andrade WN, Baxter N, Semple JL. Clinical determinants of patient satisfaction with breast reconstruction. Plast Reconstr Surg 2001;107:46-54. [Crossref] [PubMed]
- Anderson SG, Rodin J, Ariyan S, et al. Treatment considerations in postmastectomy reconstruction: Their relative importance and relationship to patient satisfaction. Ann Plast Surg 1994;33:263-70; discussion 270-1. [Crossref] [PubMed]
- Rowland JH, Dioso J, Holland JC, et al. Breast reconstruction after mastectomy: who seeks it, who refuses? Plast Reconstr Surg 1995;95:812-22; discussion 823. [Crossref] [PubMed]
- Goin MK, Goin JM. Psychological reactions to prophylactic mastectomy synchronous with contralateral breast reconstruction. Plast Reconst Surg 1982;70:355-9. [Crossref] [PubMed]
- Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. Eur J Cancer 2000;36:1938-43. [Crossref] [PubMed]
- Ng SK, Hare RM, Kuang RJ, et al. Breast Reconstruction Post Mastectomy: Patient Satisfaction and Decision Making. Ann Plast Surg 2016;76:640-4. [Crossref] [PubMed]
- Ilonzo N, Tsang A, Tsantes S, et al. Breast reconstruction after mastectomy: A ten-year analysis of trends and immediate postoperative outcomes. Breast 2017;32:7-12. [Crossref] [PubMed]
- Tsoi B, Ziolkowski NI, Thoma A, et al. Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: A systematic review and meta-analysis. Plast Reconstr Surg 2014;133:234-49. [Crossref] [PubMed]
- Liu C, Zhuang Y, Momeni A, et al. Quality of life and patient satisfaction after microsurgical abdominal flap versus staged expander/implant breast reconstruction: A critical study of unilateral immediate breast reconstruction using patient-reported outcomes instrument BREAST-Q. Breast Cancer Res Treat 2014;146:117-26. [Crossref] [PubMed]
- Lagendijk M, van Maaren MC, Saadatmand S, et al. Breast conserving therapy and mastectomy revisited: Breast cancer-specific survival and the influence of prognostic factors in 129,692 patients. Int J Cancer 2018;142:165-75. [Crossref] [PubMed]
- Atisha DM, Rushing CN, Samsa GP, et al. A National Snapshot of Satisfaction with Breast Cancer Procedures. Ann Surg Oncol 2015;22:361-9. [Crossref] [PubMed]
- Lee C, Sunu C, Pignone M. Patient-Reported Outcomes of Breast Reconstruction after Mastectomy: A Systematic Review. J Am Coll Surg 2009;209:123-33. [Crossref] [PubMed]
- Blazeby JM, Avery K, Sprangers M, et al. Health-related quality of life measurement in randomized clinical trials in surgical oncology. J Clin Oncol 2006;24:3178-86. [Crossref] [PubMed]
- Santosa KB, Qi J, Kim HM, et al. Long-term Patient-Reported Outcomes in Postmastectomy Breast Reconstruction. JAMA Surg 2018;153:891-9. [Crossref] [PubMed]
- Lagendijk M, van Egdom LSE, van Veen FEE, et al. Patient-Reported Outcome Measures May Add Value in Breast Cancer Surgery. Ann Surg Oncol 2018;25:3563-71. [Crossref] [PubMed]
- Weichman KE, Broer PN, Thanik VD, et al. Patient-reported satisfaction and quality of life following breast reconstruction in thin patients: A comparison between microsurgical and prosthetic implant recipients. Plast Reconstr Surg 2015;136:213-20. [Crossref] [PubMed]
- McCarthy CM, Mehrara BJ, Long T, et al. Chest and upper body morbidity following immediate postmastectomy breast reconstruction. Ann Surg Oncol 2014;21:107-12. [Crossref] [PubMed]
- Eltahir Y, Werners LL, Dreise MM, et al. Which breast is the best? Successful autologous or alloplastic breast reconstruction: Patient-reported quality-of-life outcomes. Plast Reconstr Surg 2015;135:43-50. [Crossref] [PubMed]
- Hu ES, Pusic AL, Waljee JF, et al. Patient-reported aesthetic satisfaction with breast reconstruction during the long-term survivorship period. Plast Reconstr Surg 2009;124:1-8. [Crossref] [PubMed]
- Jeevan R, Browne JP, Gulliver-Clarke C, et al. Surgical determinants of patient-reported outcomes following postmastectomy reconstruction in women with breast cancer. Plast Reconstr Surg 2017;139:1036e-45e. [Crossref] [PubMed]
- Dean NR, Crittenden T. A five year experience of measuring clinical effectiveness in a breast reconstruction service using the BREAST-Q patient reported outcomes measure: A cohort study. J Plast Reconstr Aesthet Surg 2016;69:1469-77. [Crossref] [PubMed]
- Tønseth KA, Hokland BM, Tindholdt TT, et al. Quality of life, patient satisfaction and cosmetic outcome after breast reconstruction using DIEP flap or expandable breast implant. J Plast Reconstr Aesthet Surg 2008;61:1188-94. [Crossref] [PubMed]
- Thorarinsson A, Fröjd V, Kölby L, et al. Long-Term Health-Related Quality of Life after Breast Reconstruction: Comparing 4 Different Methods of Reconstruction. Plast Reconstr Surg Glob Open 2017;5:e1316. [Crossref] [PubMed]
- Santosa KB, Qi J, Kim HM, et al. Effect of Patient Age on Outcomes in Breast Reconstruction: Results from a Multicenter Prospective Study. J Am Coll Surg 2016;223:745-54. [Crossref] [PubMed]
- Lagendijk M, van Egdom LSE, Richel C, et al. Patient reported outcome measures in breast cancer patients. Eur J Surg Oncol 2018;44:963-8. [Crossref] [PubMed]
- Pusic AL, Matros E, Fine N, et al. Patient-reported outcomes 1 year after immediate breast reconstruction: Results of the Mastectomy Reconstruction Outcomes Consortium study. J Clin Oncol 2017;35:2499-506. [Crossref] [PubMed]
- Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: The BREAST-Q. Plast Reconstr Surg 2009;124:345-53. [Crossref] [PubMed]
- Cano SJ, Klassen AF, Scott AM, et al. The BREAST-Q: Further validation in independent clinical samples. Plast Reconstr Surg 2012;129:293-302. [Crossref] [PubMed]
- Tan ML, Idris DB, Teo LW, et al. Validation of EORTC QLQ-C30 and QLQ-BR23 questionnaires in the measurement of quality of life of breast cancer patients in Singapore. Asia Pac J Oncol Nurs 2014;1:22-32. [Crossref] [PubMed]
- Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 1992;305:160-4. [Crossref] [PubMed]