
Inframammary fold subcutaneous cushion assessment using MRI (magnetic resonance imaging)
Introduction
Mastectomy rates for breast cancer have increased in the United States of America, with a parallel increase in prophylactic contralateral mastectomy. Consequently, immediate breast reconstruction has also increased (1). Improvements in breast cancer treatment comprising oncoplastic and less radical surgeries represents an enhancement in quality of life for patients, maintaining or recovering their body image (2).
Because of higher aesthetical outcomes demands in breast reconstruction, surgical techniques have been developed to manipulate breast structures, with or without prosthesis (3). The inframammary fold (IMF) is a critical visual marker for the breast; it is one of the most important elements in the determination of the aesthetic of the female breast (4-6). The maintenance of this anatomical marker is one of the main principles for reaching acceptable results in breast surgery, including breast reduction, augmentation and reconstruction (3-5).
IMF consists in a crest of dense nodular tissue forming an arch in the caudal circumferential border. In this topography, mammary tissue is firmly surrounded by the deep fascia in the chest wall, compressed between the anterior and posterior lamellae of the superficial fascia. IMF is anatomically set as an area where the skin of the inferior pole of glandular breast meets the chest wall (7,8) and it is located in the lower margin of the pectoralis major muscle, lined up to the sixth rib—eventually also to the seventh rib. Because the IMF is a ligamentous structure or a dense collagenous network, its function is to act as an adhesion area between the dermis and the fascia of the underlying pectoralis (3). The IMF presence has been confirmed in 8 months fetus and its position is lifelong maintained (9).
During mastectomies it is important to preserve the subcutaneous portion nearby the IMF, attempting that, this preservation will greatly facilitate reconstruction (8) allowing more satisfying aesthetic results (4).
The quantity of mammary tissue in the IMF was defined as changeable (8). As mastectomy has become less radical, there is reluctance in resecting IMF contents routinely, whereas it can lead to a bad IMF definition or distortion, therefore, prejudicing the aesthetic result after an immediate reconstruction. Traditional total mastectomy description includes the visualization of anterior rectus sheath and of external oblique muscle fibers when the lower mastectomy flap is elevated. The utilization of this statement (resecting all the subcutaneous tissue around the IMF) turns the dissection of the submuscular pocket (for the placement of the implant) almost impossible, especially when dermal matrix is not available. Moreover, this area might be avoided in order to keep adherence zone (8), responsible for and adequate definition of the breast lower pole anatomy.
The aim of the present study is to evaluate the anatomy of the subcutaneous IMF cushion using MRI acquisition images. The thickness of this structure was measured in women with no previous breast surgery. These data were discussed showing that the subcutaneous IMF cushion is present in all patients, it varies regarding its thickness, but surgeons have to be aware of the necessity of preserving it, as this anatomical marker does not have breast parenchyma to indicate its inclusion in the oncological resection.
Methods
We have gauged the right breast IMF subcutaneous cushion from 50 patients who were submitted to magnetic resonance imaging (MRI) in a diagnosis radiology center, between January and February of 2017.
In this study, there were included women without previous surgery in this topography. Nonetheless, women submitted to radiotherapy or previous surgery procedures in any of breast sides and manly cases were excluded. MRI images were analyzed in T1 fat saturated sequences.
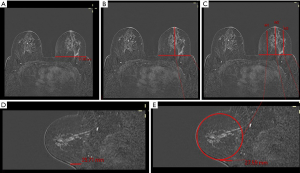
Initially, the breast base was measured in axial slices view, lined up to the mammary bud. Following, the breast meridian was calculated by dividing the gauge of the breast base by 2—that point was named “M2”. The meridian size (“M2”) was also divided by 2, resulting in other two measurements: “M1” and “M3” points (Figure 1).
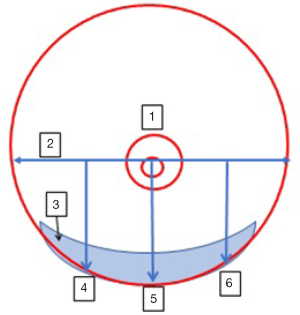
Therefore, the assessment of the fold cushion was realized in the projection of axial measurements in sagittal plane. The gauge was taken in continuity of mammary projection, as the breasts were pendent for the exam (Figure 2).
Results
Among the 50 evaluated patients, the mean age was 42.74 years (varying from 22 to 58 years). The mean measure of breast base was 9.91 cm (varying from 6.61 to 13.7 cm).
The mean measure of the subcutaneous IMF cushion assessment, in projection of M1 point in sagittal plane, was 2.96 (varying from 1.32 to 6.02 cm, with percentile 5% of 1.39 cm and percentile 95% of 5.11 cm). In M2 and M3 points projection in sagittal plane, the mean measures were, respectively, 2.40 cm (varying from 1.34 to 4.05 cm, with percentile 5% of 1.50 cm and percentile 95% of 3.55 cm) and 2.21 cm (varying from 0.9 to 3.69 cm, with percentile 5% of 1.29 cm and percentile 95% of 3.18 cm). Referred data are presented in detail in Table 1.
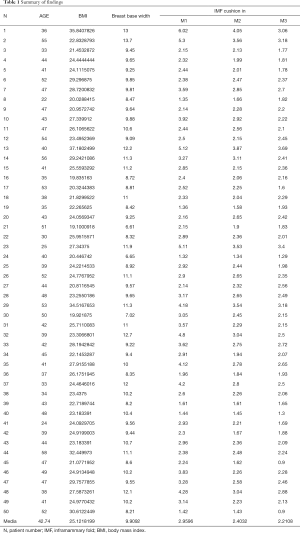
Full table
Discussion
The incidence of breast cancer in the IMF appears to be less than 2% (8). In the literature, there’s only one case of breast cancer forming along the IMF after prophylactic mastectomy of the right breast, in a patient with an original lobular carcinoma in situ in the left breast (10). Confirming this data, Behranwala et al., reviewed 580 patients with a diagnosis of breast cancer and detected four (0.7%) cases of primary breast tumors of the SIM. All the four tumors were clinically palpable and were positive for malignancy in fine needle aspiration biopsy (7).
Gui et al. reported 50 specimens of IMF—from 42 patients who underwent mastectomy—were studied histologically. Nearly a quarter of the resected IMF specimens contained breast tissue (22%), and this was not related to patient age and body mass index (8). Carlson et al. also analyzed 24 mastectomy specimens, in which the IMF was removed separately. The specimens were submitted to histological analysis and to computer image analysis to quantify the mammary tissue present in the IMF. More than half of the analyzed IMF specimens (13/24) contained breast tissue, but the quantitation by computer image analysis found the mean value for breast tissue in the specimens was 0.02%. All the IMF samples were carcinoma negative, but one specimen was positive for focal ductal hyperplasia (9).
The breast is supported by the Cooper’s ligament, which is a peripheral projection of the mammary tissue into fibrous projections that emerges with the superficial lamina of the superficial fascia. Carlson et al. demonstrated that these projections are intimately associated with the skin, and for complete resection of the breast tissue a large amount of skin should be resected (9).
Despite the presence of mammary tissue, even if it is derisory in IMF, its preservation is justified not only by the low rate of neoplastic involvement in this topography, but mainly because there will always be remnants of breast tissue even in the most aggressive mastectomies. This has been previously shown by Barton et al., who compared total glandular mastectomy and modified radical mastectomy for the amount of breast tissue remaining after surgery. To evaluate this, multiple biopsies were taken from the anterior chest wall. They found residual breast tissue after glandular mastectomy in 22% of cases, and in 21% of patients submitted to modify radical mastectomy. Biopsy taken from the IMF found breast tissue in 5.4% of the specimens (11).
The present study is unprecedented in the literature, and we have not similar papers to compare ours results. In those studies that evaluated the volume of IMF in resected specimens, the results of the measurements were disparate, varying from 0.27 to 205.2 cm3 (9). The measurement of the usual thickness of the IMF cushion provides a guidance for the Mastologist during the resection, in order to achieve a desirable amount of remaining subcutaneous (Figure 3). Unlike the calculation of the residual tissue volume, which would not be practicable in the intraoperative routine, the measurement of fold thickness is directly, rapidly and easily taken during surgery.

In this study, the cushion’s measurement made by magnetic draws a broad and undistorted view of the thickness of this tissue, since the measurements were made in patients with no history of previous local surgery.
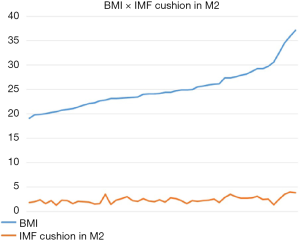
We correlate the cushion’s thickness in the inframammary crease with the patients’ body mass index: overweight patients have higher projections of the measures. Although, the relationship is not a linear one, according to our measures (see Figure 4).
Recreating the IMF is a difficult task, and becomes more complicated when the reconstruction is performed with implants (currently the most common form of immediate reconstruction) rather than with autologous tissues. Several techniques have been developed to recreate IMF, sometimes with failure to recreate reconstructed breast support and shape, or loss of long-term outcome, and sometimes adding local morbidity (such as more extensive scars) (12).
Conclusions
The preservation of the IMF during the mastectomies is an aspect of extremely importance for the next step—the breast reconstruction. Given that the studies indicate the negligible amount of breast tissue and the low incidence of neoplasia in this topography, the preservation of the IMF seems feasible. The measurements of the IMF thickness, evaluated by MRI in this study, provide reference values for maintaining a desirable inframammary crease. This can avoid cases of reconstruction failure, when the shape and support of the breast can sometimes not be satisfactorily rebuilt because there has been loss or violation of the IMF.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Patients’ data was retrieved from an imaging record system. We did not have any contact with the patients, and they were not exposure to risk factors. The study was retrospective and the outcomes will not affect the future management of these patients.
References
- Fowble B, Park C, Wang F, et al. Rates of Reconstruction Failure in Patients Undergoing Immediate Reconstruction With Tissue Expanders and/or Implants and Postmastectomy Radiation Therapy. Int J Radiat Oncol Biol Phys 2015;92:634-41. [Crossref] [PubMed]
- Ismagilov A, Vanesyan A, Kamaletdinov I. Small refinements in breast reconstruction: a technique for inframammary fold creation. Gland Surgery 2017;6:132-40. [Crossref] [PubMed]
- Maclin MM 2nd, Deigni OA, Bengtson BP. The Laminated Nature of the Pectoralis Major Muscle and the Redefinition of the Inframammary Fold: Clinical Implications in Aesthetic and Reconstructive Breast Surgery. Clin Plast Surg 2015;42:465-79. [Crossref] [PubMed]
- Bogetti P, Cravero L, Spagnoli G, et al. Aesthetic role of the surgically rebuilt inframammary fold for implant-based breast reconstruction after mastectomy. J Plast Reconstr Aesthet Surg 2007;60:1225-32. [Crossref] [PubMed]
- Chun YS, Pribaz JJ. A simple guide to inframammary-fold reconstruction. Ann Plast Surg 2005;55:8-11. [Crossref] [PubMed]
- Muntan CD, Sundine MJ, Rink RD, et al. Inframammary fold: a histologic reappraisal. Plast Reconstr Surg 2000;105:549-56. [Crossref] [PubMed]
- Behranwala KA, Gui GP. Breast cancer in the inframammary fold: is preserving the inframammary fold during mastectomy justified? Breast 2002;11:340-2. [Crossref] [PubMed]
- Gui GP, Behranwala KA, Abdullah N, et al. The inframammary fold: contents, clinical significance and implications for immediate breast reconstruction. Br J Plast Surg 2004;57:146-9. [Crossref] [PubMed]
- Carlson GW, Grossl N, Lewis MM, et al. Preservation of the inframammary fold: what are we leaving behind? Plast Reconstr Surg 1996;98:447-50. [Crossref] [PubMed]
- Cederna JP. Preservation of the inframammary fold: a plea for close follow-up. Plast Reconstr Surg 1997;99:2114-5. [Crossref] [PubMed]
- Barton FE Jr, English JM, Kingsley WB, et al. Glandular excision in total glandular mastectomy and modified radical mastectomy: a comparison. Plast Reconstr Surg 1991;88:389-92. [Crossref] [PubMed]
- Tomita K, Yano K, Nishibayashi A, et al. Aesthetic outcomes of inframammary fold recreation in two-stage, implant-based, breast reconstruction. Springerplus 2016;5:1656. [Crossref] [PubMed]


