Patient satisfaction following thyroidectomy in surgical mission: a prospective study
Introduction
The primary role of iodine deficiency in goitrogenesis and the primary role of endemic goiter in the incidence of thyroid cancers is well-established (1). Iodine deficiency was defined by the WHO as “the single most important preventable cause of brain damage” (2). Although Philippines has been improving the prevention of iodine deficiency through government policies since 1995 (3), endemic goiter, thyroid carcinoma in addition to mental disorders due to iodine deficiency in newborns still exist in most parts of the country. Multinodular or large goiters with compressive symptoms as well as thyroid cancers mandate surgery varying from partial resection to total thyroidectomy.
Thyroid surgery performed in the context of a surgical mission is underreported and comprises a case report and an observational study on fine needle cytology (4,5). Even though safety and efficiency of surgical missions have been reported in the literature, they were never evaluated for thyroid surgery.
Operation Giving Back (OGB) program, a comprehensive platform for volunteers, partners, philanthropists, policy makers, and the public was created by the American College of Surgeons (ACS) in 2004 (6). OGB Bohol is a surgical mission held in Bohol Province, Philippines from 2006 and led by US based surgeons (7). The aim of this study was to evaluate the safety and patient satisfaction of thyroid surgery performed within a surgical mission.
Methods
This was a prospective descriptive cohort study conducted during the surgical mission carried out in Bohol Province, Philippines in 2018. Adults patients >18 years old who underwent thyroid surgery were included. The data including patients’ baseline, intra-, and postoperative variables as well as patient satisfaction were collected to predefined Microsoft Excel spreadsheets. Postoperative complications were defined as any deviation from the normal postoperative course and classified according to Clavien-Dindo system (8). Safety endpoint was observed postoperative complication rate as compared with its observed counterpart. Patient satisfaction was evaluated using a 5-point Likert scale and was collected anonymously by an independent researcher (1 was “very unsatisfied”, 2- “unsatisfied”, 3- “unsure”, 4- “satisfied”, and 5- “very satisfied”). All procedures were performed under general anesthesia after obtaining patients’ consent. Thyroid surgery included partial, subtotal, and total thyroidectomies depending on the type and extent of the disease. Discharge home criteria included no evidence of complications, ambulation and ability for self-care or good family support, tolerance of oral intake, adequate pain control with oral analgesia, and recovery of lower gastrointestinal and urinary functions. The study report complies with the STROCSS criteria (9). American College of Surgeons National Surgical Quality Improvement Program Surgical Risk Calculator (ACS-NSQIP SRC) was used to evaluate the predicted risk of complications (10). Statistical analysis was performed using SPSS software (version 18; SPSS Inc., Chicago, IL, USA). To calculate an expected rate, the mean risk of an outcome was calculated. Chi-squared test was used to compare expected and observed postoperative complication rates. Statistical significance was defined as P<0.05.
Results
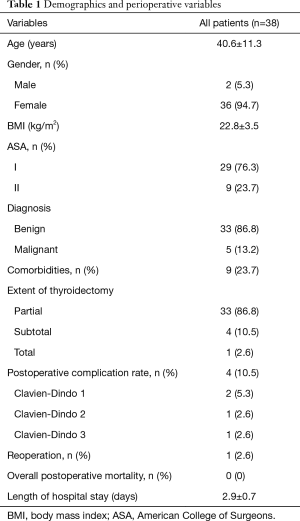
Thirty-eight patients underwent thyroidectomy performed by four surgeons in February 2018 mission. Demographics and perioperative variables are shown in Table 1. Mean age of the patients was 40.6±11.3 years. Male to female ratio was 2:36. Goiter was the indication for surgery in 33 (86.8%) patients, whereas 5 (13.2%) patients had tumors. Extent of thyroidectomy was partial in 33 (87%), subtotal in 4 (10.5%), and total in 1 (2.6%) patients. Four complications were observed, of which only one was Clavien-Dindo class 3. This was a patient with postoperative neck hematoma who underwent re-exploration. There were no Clavien-Dindo 4 complications. Mortality rate was 0.
Full table
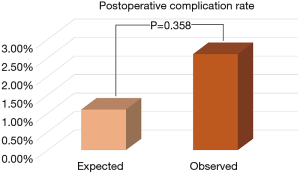
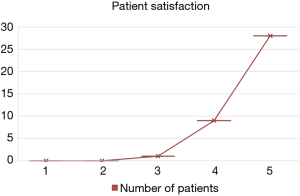
Figure 1 depicts the safety endpoint of the study. Expected complication rate was found to be 1.1% using the ACS-NSQIP SRC. Expected vs. observed complication rate was not found to be significantly different (P=0.358). Figure 2 depicts patient satisfaction. Twenty-eight patients were very satisfied (5 points on the Likert scale), 9 patients were satisfied, and 1 patient was unsure.
Discussion
The main finding of this prospective descriptive cohort study was that thyroid surgery within a surgical mission is safe with comparable serious postoperative complication rates with those predicted by the ACS-NSQIP SRC. Patient satisfaction was excellent with 97% satisfied or very satisfied. Since its development, the above-mentioned tool for surgical risk assessment is widely used for decision support or quality control in different settings (11). A recent retrospective cohort study reported discrepancy between ACS-NSQIP SRC predicted and observed rates of reoperation, emergency room visits, and readmissions (12). To the best of our knowledge, that was the only study where ACS-NSQIP SRC was utilized in thyroid surgery. Another recent study reporting the outcomes of US Navy’s Pacific Partnership mission used ACS-NSQIP SRC in the setting of a surgical mission and found that the calculator overpredicted postoperative morbidity risk (2.0% vs. 0.7%) (13). However, the authors concluded that the calculator offers a good starting point for humanitarian surgery risk calculation.
Extent of thyroidectomy has been debated over the last two decades. Authors advocating subtotal or total thyroidectomy expressed concern about increased recurrence rates of multinodular goiter after partial thyroidectomy (14,15). On the other hand, subtotal and total thyroidectomy entail lifelong L-thyroxin replacement and increased postoperative morbidity (16). In our mission, limited access to lifelong thyroxin replacement therapy, need for frequent follow-up visits, as well as increased risk of postoperative complications were factors encouraging partial thyroidectomy, provided goiter is unilateral.
Patient satisfaction after thyroid surgery is a metrics which is not easy to evaluate. The lack of validated comprehensive scoring systems leads to the use of different self-administered scales in the evaluation of patient satisfaction. In fact, a recent cross-sectional study comparing radiofrequency ablation to surgery for benign thyroid nodules used a self-administered questionnaire to evaluate patient satisfaction (17). Another recent study used a 5-point Likert scale as we did to evaluate patient satisfaction (18). However, the fact that 97% of patients were satisfied with thyroid surgery performed during the mission is a good adjunct to the safety of thyroid surgery encouraging to help people in low-income countries with high incidence of benign and malignant thyroid diseases.
We would like to acknowledge limitations of our study. First, as any other observational study, this prospective cohort study might be imposed to selection bias. Another limitation is the fact that patients were evaluated immediately after surgery. This is the time when they realize that they do not carry the massive goiters (in mist cases) any longer. Lack of a validated patient satisfaction assessment tool and language barrier are other limitations.
Conclusions
This prospective cohort study found thyroid surgery performed within a surgical mission to be safe. Patient satisfaction assessment showed 97% satisfaction rate. Further research is needed to develop and validate standardized patient satisfaction assessment tools.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by University of Arizona and Borja Hospital (Tagbilaran, Philippines) and written informed consent was obtained from all patients.
References
- Gaitan E, Nelson NC, Poole GV. Endemic goiter and endemic thyroid disorders. World J Surg 1991;15:205-15. [Crossref] [PubMed]
- WHO/ICCIDD. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers. 3 edition. Geneva, Switzerland: 2007.
- Kim BK, Jeong JY, Seok KH, et al. Current iodine nutrition status and awareness of iodine deficiency in Tuguegarao, Philippines. Int J Endocrinol 2014;2014:210528. [Crossref] [PubMed]
- Latifi R, Harper J, Rivera R. Total thyroidectomy for giant goiter under local anesthesia and Ketamine in a surgical mission. Int J Surg Case Rep 2015;8C:52-4. [Crossref] [PubMed]
- Reyes CV, Reyes EA. The role of fine needle aspiration cytology in medical-surgical missions. Acta Cytol 2009;53:524-6. [Crossref] [PubMed]
- American College of Surgeons. Operation Giving Back. Available online: https://www.facs.org/ogb. [Accessed October 10, 2018].
- Latifi R, Rivera R, Gachabayov M, et al. Outcomes of 1,327 patients operated on through twelve multispecialty volunteerism missions: A retrospective cohort study. Int J Surg 2018;60:15-21. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Agha RA, Borrelli MR, Vella-Baldacchino M, et al. STROCSS Group. The STROCSS statement: Strengthening the Reporting of Cohort Studies in Surgery. Int J Surg 2017;46:198-202. [Crossref] [PubMed]
- American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) Surgical Risk Calculator. Available online: https://riskcalculator.facs.org/RiskCalculator/index.jsp [Accessed October 10, 2018].
- Bilimoria KY, Liu Y, Paruch JL, et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 2013;217:833-42.e1-3.
- Margolick J, Wiseman SM. Risk of major complications following thyroidectomy and parathyroidectomy: Utility of the NSQIP surgical risk calculator. Am J Surg 2018;215:936-41. [Crossref] [PubMed]
- Berger JH, Jiang Z, O'Reilly EB, et al. First Do No Harm: Predicting Surgical Morbidity During Humanitarian Medical Missions. World J Surg 2018;42:3856-60. [Crossref] [PubMed]
- Wadström C, Zedenius J, Guinea A, et al. Multinodular goitre presenting as a clinical single nodule: how effective is hemithyroidectomy? Aust N Z J Surg 1999;69:34-6. [Crossref] [PubMed]
- Boutzios G, Tsourouflis G, Garoufalia Z, et al. Long-term sequelae of the less than total thyroidectomy procedures for benign thyroid nodular disease. Endocrine 2019;63:247-51. [Crossref] [PubMed]
- Makay Ö. Less than total thyroidectomy for goiter: when and how? Gland Surg 2017;6:S49-58. [Crossref] [PubMed]
- Bernardi S, Dobrinja C, Carere A, et al. Patient satisfaction after thyroid RFA versus surgery for benign thyroid nodules: a telephone survey. Int J Hyperthermia 2018;35:150-8. [Crossref] [PubMed]
- Doo AR, Hwang H, Ki MJ, et al. Effects of preoperative oral carbohydrate administration on patient well-being and satisfaction in thyroid surgery. Korean J Anesthesiol 2018;71:394-400. [Crossref] [PubMed]