Visualized oncoplastic surgery of the breast I: inferior and medial quadrantectomy
Introduction
Inverted T reductions by the superior pedicle for inferior and medial tumors
With oncoplastic reduction techniques, tumors can be easily resected with large safety margins, avoiding important cosmetic postoperative defects. Reducing breast size decreases retraction risk significantly, without affecting adjuvant therapies, clinical and radiological follow-up (1-3).
The design of these therapeutic reductions is based on a keyhole Wise pattern (“inverted T”) or a “V” design. The areola can be repositioned as needed, including the lesion within the resection piece. The choice of the pedicle that will ensure nipple-areola complex (NAC) irrigation will depend on tumor location and glandular resection (3,4).
For tumors located at the inferomedial or lateral quadrants, the keyhole pattern may rotate slightly and allow better lateral or medial resections. The NAC is moved in the opposite direction to the surgical defect after piece resection, remaining; as a result, an inverted T scar (5,6).
The resection piece should be full thickness, and the remaining breast tissue should be advanced to minimize the defect. When treating the contralateral breast simultaneously with mirror procedures, the surgeon should remove any suspicious tissue revealed by preoperative mammogram (7,8).
We aim to offer a detailed step by step technique description of this oncoplastic procedure.
Operative technique
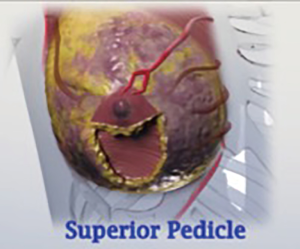
Superior pedicle
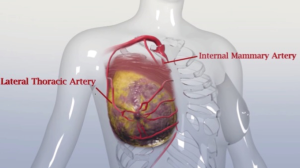
The superior pedicle technique is especially suitable for tumors located in the junction of the lower medial & lateral quadrants, especially in large breasts with ptosis, since the areola that must be repositioned in a more cephalic position at least 10 or 11 cm below the clavicle (9,10).
These tumor locations are the most difficult to locate since the lateroareolar segment of the breast is the area where the mammary gland is poorer, especially if ptosis is important.
The pre-established drawing resumes the Wise pattern in a keyhole. This technique allows to refill the resected area due to the superior dermoglandular pedicle, the area corresponding to the resection of the tumor located at the junction of the upper quadrants above the areola. To reduce the dead space and the consequent seroma, a beveled (inverted pyramidal form) glandular resections, must be performed if possible (11,12).
The preoperative scheme and resulting scar are identical to those of the inverted T with the inferior pedicle. The quadrantectomy zone corresponds to the future implantation area of the NAC. The skin incision follows the rounded tracing and goes in monoblock up to the pectoralis major fascia plane, with the skin detached laterally along the vertical and horizontal lower incisions.
The complete piece that contains the tumor with sufficient margins resembles a horseshoe. The inferior pedicle must be no less than 8 cm wide to ensure the vascularity and vitality of the NAC (13,14); likewise, the dissection must be careful, in a pyramidal manner, so as not to release the said pedicle from its adherence to the pectoralis major and the rib cage. By raising the NAC, the reconstructed glandular tissue allows the skin to be closed above, reconstructing a smaller breast with a narrower base and the NAC relocated in a more cephalic position (15,16). This technique allows en bloc resection, reaching the chest plate, and including the tumor in the resected piece.
The opposite breast symmetrization is carried out simultaneously using a similar technique, providing the same results in terms of volume and scars (17-19). Resection over the contralateral breast must be approximately 10% larger than the affected breast; this observation is important considering that postoperative radiotherapy will reduce the size of the treated breast (20,21).
Indications
Superior pedicle with Wise incision pattern
- Large or moderate, breast volume with lower inner and lower outer quadrant lesions;
- Indicated in the large ptotic breast, grade II or III.
Operative markings
Agreement between the surgical team, plastic, and oncologic surgeon, leads to the ideal selection of type and position of skin incision.
As an oncologic principle, large inferior quadrant lesions can be easily resected. Also, breast tissue including the pectoralis fascia can be resected to increase safety, regarding negative posterior margins.
Surgical marking is performed in a stand-up position. When the tumor is palpable, it is advisable to outline it during this marking process.
A midline, beginning at the suprasternal notch and running inferiorly to umbilicus is drawn. Two meridian lines were running from midclavicular point to the inframammary fold (IMF), is selected as the central position of the new NAC. Two cm higher from the projected point over the meridian line at the IMF will result in the higher borderline point of the new NAC. The distance between the midline and new nipple should result between 9–11 cm over the meridian line, and the distance from the suprasternal notch and the new both sides nipples usually remains between 18–22 cm. After marking the tumor location on the skin, a Wise keyhole pattern is designed including in it the lesions to be resected. The keyhole marking can be rotated laterally or enlarged to include better the tumor in the resection piece, and a superiorly based pedicle is designed (Figures 1-3).

Intraoperative steps
- Markings with the patient in stand-up position (Figure 4);
- Sentinel or complete axillary lymph node dissection can be performed through the same or by a separate axillary incision;
- NAC is placed under slight stretch. Mark with the corresponding desired size cookie cutter and drawn with a pen the new NAC size and position centered over the meridian line;
- Perform the breast-conserving surgery (BCS) with full-thickness resections and including the pectoralis fascia in the corresponding region of the lesion (Figure 5);
- Mark the BCS resection piece to allow pathology margin assessment. Weigh the specimen that has been removed. Try to leave approximately 10% more volume on this side, as it will undergo radiation with posterior volume reduction;
- Complete closure of the lateral and medial pillars in a standard Wise pattern;
- Special care needs to be given to allow symmetrical appearance, especially to obtain a natural midpoint closure on the IMF, without lateral dog ears. That’s the importance of preoperative markings;
- Finish closure (Figure 6).
Comments
Various factors may influence decisions regarding breast reconstruction technique, such as smoking, obesity, diabetes, autoimmune diseases, and previous scars or radiotherapy. These previous conditions may cause an increase in the complications rates with the commonly used reconstruction techniques (23,24). Obesity can rise complication rates up to 12 times, and smoking may directly lead to vasoconstrictor in the skin and indirectly alter capillary flow, which can increase necrosis in skin flaps and NAC (18,25,26) (Figure 7).
In our experience superior pedicle technique to resect inferior or lateral lesions allows a safe oncologic treatment in large and ptotic breasts with great cosmetic outcome Denewer et al. (16) reported on the complications of therapeutic reductions. In 35 patients who underwent inferior pedicle reduction mastoplasty as therapy for tumors in the upper quadrants, they observed that the most common early complication (first postoperative week) was wound dehiscence (17.6%). This was mainly in the lower part of the vertical scar in its consequence with the horizontal scar in the submammary fold. However, in most cases, it resolved with conservative treatment. The authors noted that other early complications, in order of frequency, were the presence of partial skin necrosis (11%), infection, fat necrosis, hematoma, and partial areola necrosis (3%). Seroma is reported as the most frequent late complication (14.7%), but all cases resolved with aspiration puncture. Long-term bad scaring is reported as 5% (Figure 8). These data are similar to those reported by Hernanz et al. (27), in their study of 57 patients who underwent therapeutic reduction mammoplasty, and by Gulcelik et al. (28).
Aesthetic results
All the reported works agree that the cosmetic result and patients’ satisfaction who underwent therapeutic reduction mastoplasty is higher than 80% when evaluated 6 months after the surgical intervention. The parameters evaluated were volume symmetry, breast shape, the symmetry of the areolar complexes, and scars (16,27,29).
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Rancati A, Gonzalez E, Angrigiani C, et al. Oncoplastic options in breast conservative surgery. Gland Surg 2013;2:163-9. [PubMed]
- Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002;347:1227-32. [Crossref] [PubMed]
- Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002;347:1233-41. [Crossref] [PubMed]
- Audretsch W, Rezai M, Kolotas C, et al. Tumor-Specific Immediate Reconstruction in Breast Cancer Patients. Semin Plast Surg 1998;11:71-100. [Crossref]
- Navarro Martínez M, Navarro Campos BC, Navarro Campos LJ. Cirugía conservadora en cáncer de mama con técnica de reducción en mamas voluminosas. Revista Venezolana de Oncología 2016;28:78-86.
- Asgeirsson KS, Rasheed T, McCulley SJ, et al. Oncological and cosmetic outcomes of oncoplastic breast conserving surgery. Eur J Surg Oncol 2005;31:817-23. [Crossref] [PubMed]
- Bong J, Parker J, Clapper R, et al. Clinical series of oncoplastic mastopexy to optimize cosmesis of large-volume resections for breast conservation. Ann Surg Oncol 2010;17:3247-51. [Crossref] [PubMed]
- Clough KB, Kaufman GJ, Nos C, et al. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol 2010;17:1375-91. [Crossref] [PubMed]
- Anderson BO, Masetti R, Silverstein MJ. Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques. Lancet Oncol 2005;6:145-57. [Crossref] [PubMed]
- Masetti R, Pirulli PG, Magno S, et al. Oncoplastic techniques in the conservative surgical treatment of breast cancer. Breast Cancer 2000;7:276-80. [Crossref] [PubMed]
- Chang E, Johnson N, Webber B, et al. Bilateral reduction mammoplasty in combination with lumpectomy for treatment of breast cancer in patients with macromastia. Am J Surg 2004;187:647-50; discussion 650-1. [Crossref] [PubMed]
- Hernanz De La Fuente F, Gómez Fleitas M, Martínez García F. Reduction mammaplasty in breast cancer surgery. Cir Esp 2009;85:140-6. [Crossref] [PubMed]
- Acea-Nebril B, Cereijo-Garea C, García-Novoa A, et al. The role of oncoplastic breast reduction in the conservative management of breast cancer: Complications, survival, and quality of life. J Surg Oncol 2017;115:679-86. [Crossref] [PubMed]
- Kaviani A, Safavi A, Mohammadzadeh N, et al. Oncoplastic surgery in breast conservation: a prospective evaluation of the patients, techniques, and oncologic outcomes. Am J Surg 2014;208:727-34. [Crossref] [PubMed]
- Clough KB, Lewis JS, Couturaud B, et al. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg 2003;237:26-34. [Crossref] [PubMed]
- Denewer A, Elnahas W, Hussein O, et al. Evaluation of Inferior Pedicle Therapeutic Mammoplasty as a Primary Procedure for Upper Quadrants Early Breast Cancer. Adv Breast Cancer Res 2013;2:86-90. [Crossref]
- Goffman TE, Schneider H, Hay K, et al. Cosmesis with bilateral mammoreduction for conservative breast cancer treatment. Breast J 2005;11:195-8. [Crossref] [PubMed]
- Chen CL, Shore AD, Johns R, et al. The impact of obesity on breast surgery complications. Plast Reconstr Surg 2011;128:395e-402e. [Crossref] [PubMed]
- Rancati A, Gonzalez E, Dorr J, et al. Oncoplastic surgery in the treatment of breast cancer. Ecancermedicalscience 2013;7:293. [PubMed]
- Lin KY, Johns FR, Gibson J, et al. An outcome study of breast reconstruction: presurgical identification of risk factors for complications. Ann Surg Oncol 2001;8:586-91. [Crossref] [PubMed]
- Stefanek M, Hartmann L, Nelson W. Risk-reduction mastectomy: clinical issues and research needs. J Natl Cancer Inst 2001;93:1297-306. [Crossref] [PubMed]
- Rancati A, Angrigiani C, Dorr J, et al. Surgical technique video, inferior quadrantectomy by superior pedicle. Asvide 2019;6:298. Available online: http://www.asvide.com/watch/32983
- Le Bouëdec G, Vergote T, Kauffmann P, et al. Immediate breast reconstruction following mastectomy for recurrence after conservative treatment. J Chir (Paris) 1994;131:138-43. [PubMed]
- Audretsch W, Rezai M, Kolotas C. Oncoplastic surgery: “target” volume reduction, (BCT mastopexy), lumpectomy reconstruction (BCT reconstruction) and ap supported operability in breast cancer. Proceedings of the Second European Congress on Senology; 1994; Vienna, Austria. Bologna, Italy: Monduzzi; 1994:139-57.
- Silverstein M. Cosmetic quadrantectomy. Annual Miami Breast Cancer Conference; Miami, FL; 1993.
- Rancati A, Irigo M, Angrigiani C. Management of the Ischemic Nipple-Areola Complex After Breast Reduction. Clin Plast Surg 2016;43:403-14. [Crossref] [PubMed]
- Hernanz F, González-Noriega M, Pérez RV, et al. Versatility of therapeutic reduction mammoplasty in oncoplastic breast conserving surgery. World J Surg Proced 2015;5:217-22. [Crossref]
- Gulcelik MA, Dogan L, Camlibel M, et al. Early complications of a reduction mammoplasty technique in the treatment of macromastia with or without breast cancer. Clin Breast Cancer 2011;11:395-9. [Crossref] [PubMed]
- Grisotti A. Immediate reconstruction after partial mastectomy. Operative Techniques in Plastic and Reconstructive Surgery 1994;1:1-12. [Crossref]