
Correction of animation deformity with subpectoral to prepectoral implant exchange
Introduction
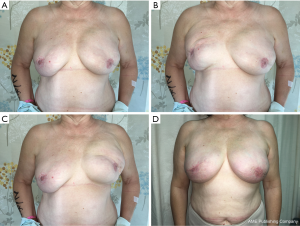
Implant-based breast reconstruction traditionally involves placement of the implant beneath the pectoralis major muscle, to provide adequate vascularized soft tissue coverage, and a lower risk of developing capsular contracture. While many patients achieve a satisfactory aesthetic result, an overwhelming proportion have been reported to develop some degree of animation deformity (Figure 1). Animation deformity refers to the tethering of the patient’s mastectomy flap skin to the underlying pectoralis major muscle, resulting in both visible contraction and lateral displacement of the entire breast mound with any activation of the pectoralis muscle (1,2). This can be painful for many patients and extremely visibly displeasing.
Several strategies have been previously described for treatment of animation deformity. However, much of the literature pertains to deformities seen following cosmetic breast augmentation, rather than breast reconstruction where the entirety of the glandular tissue has been surgically removed. This entity in the reconstructive population presents a unique challenge, with minimal to no soft tissue remaining between the pectoralis major muscle and the overlying skin.
Minimally invasive options for treatment have included the injection of botulinum toxin into the pectoralis major muscle in order to temporarily paralyze the muscle, which has been reported to have effective results, however not long lasting (3). As such, this approach carries a near 100% risk of animation recurrence.
Surgical options for addressing animation deformity have involved fat grafting and/or application of acellular dermal matrix (ADM) into the plane between the pectoralis muscle and the tethered skin. The theory with these procedures involves the placement of a spacer (fat or ADM), between the skin and muscle, with the intent of weakening their connections. While these methods have had variable success rates, neither has produced consistently reproducible correction of animation deformity.
Historically, implant pocket change from the submuscular to prepectoral position was reserved for breast augmentation patients, as concerns existed regarding the safety of placing the implant in the prepectoral plane of a reconstructed breast, directly under the thin skin envelope. However, recent studies have demonstrated successful reconstructive results when using the prepectoral plane for primary breast reconstruction (4-7). As such, implant pocket conversion from the submuscular to prepectoral plane has become our preferred method of addressing animation deformity. Additionally, when performed in conjunction with fat grafting and ADM coverage, implant pocket change to the prepectoral plane has been shown to produce optimal aesthetic results without animation deformity recurrence (8-10). In this study, we review our series of patients who have undergone implant pocket change for correction of animation deformity.
Methods
Over a 24-month period, 55 breast reconstruction revisions were performed in 31 patients for the treatment of breast animation deformity as a result of a prior submuscular prosthetic breast reconstruction. Fifty (91%) of initial reconstructions were two stage expander-implant based; five (9%) were direct to implant reconstructions. Forty-three (78%) patients had undergone their initial mastectomy and reconstruction at our institution, however the remaining 22% of patients had undergone their mastectomy and initial reconstruction at outside institutions.
All patients underwent implant pocket conversion from the submuscular to prepectoral plane, with resuspension of the pectoralis major muscle on the chest wall. All reconstructions were performed using smooth surface, round, cohesive or responsive silicone gel implants (Allergan). The senior author (HS) performed all reconstruction revision operations. Patients had at least 1 month follow-up for study inclusion, following their pocket conversion operation.
Patient medical records were reviewed for demographic information, perioperative details, and postoperative outcomes following approval from the University of California, San Francisco Institutional Review Board. All statistical analysis was performed using STATA/IC v.15.0 software.
Preoperative assessment and surgical technique
Preoperative assessment was performed by the senior author and surgical team during the patients’ initial preoperative consultation. Typically, patients presented with varying degrees of capsular contracture and animation deformity. Symptomatic complaints included pain with activation of the pectoralis major muscle, gross lateral displacement of implants with arm movements/chest flexion and dissatisfaction with the aesthetic appearance of their reconstructed breasts. Common aesthetic complaints included: blunted/flattened upper pole of the breast, widened breast appearance, and asymmetric shape. Patients were asked to flex their chest, and any movement of their implants was noted. Following initial assessment, patients were offered the option to undergo revision breast surgery with implant pocket conversion from the submuscular to the prepectoral plane. They were counseled on the risks and benefits of the operation prior to undergoing surgery.
Intraoperatively, the patient’s prior incision was typically used to perform the revisionary procedure. However, in instances when patients have had a history of breast radiation, the author’s preference is to utilize a new incision. At this point, dissection is carried down through the skin and subcutaneous tissue until the pectoralis major muscle is reached at its anterior surface.
Often, the skin and subcutaneous tissue is fairly well adhered and scarred onto the pectoralis major muscle. In our experience, we have found that it is easier to begin by first developing this plane and separating the skin flap from the underlying pectoralis muscle, while the implant is still in place. Once the superior flap is well elevated, the implant is removed and a complete open periprosthetic capsulectomy is performed.
The pectoralis major muscle is then transferred back to its original anatomic position on the chest wall and secured using PDS or Vicryl sutures, thus allowing for a new prepectoral implant pocket. A temporary sterile implant sizer is then selected based on the patients’ prior implant size and desired final breast size and placed beneath the mastectomy skin in the newly created prepectoral plane. The sizer is inflated to an appropriate volume, and adjusted for symmetry, and to ensure an appropriate volume for the selected implant.
The sizer is then removed and the breast pocket is irrigated with betadine (full strength or 50% dilution) and antibiotic irrigation.
The appropriately selected implant is then wrapped with ADM. Depending on the size of the implant, this will require at least one 16×20 cm sheet. In our series, 55% of reconstructions required a second sheet of ADM (either one additional 6×16, 8×10, or 16×20 cm. The ADM is rinsed saline, and the sheet is then fenestrated to allow for fluid drainage. The selected implant is then wrapped with the ADM. In this series, all sheets of ADM used were AlloDerm (Allergan, Inc.).
The implant is then placed sterilely into the breast pocket overlying the repositioned pectoralis muscle. One 19-French round Blake drain is then placed in the breast pocket. The incision is closed in a layered fashion and dressed with surgical glue. Patients are to wear surgical bras during the postoperative period.
Of note, we have recently modified our operative approach to some patients seeking animation correction. We are now performing these revision operations in a staged manner, in patients deemed to have subjectively thin skin. In order to provide a more robust, healthier skin flap with easier and safer dissection planes between the pectoralis muscle and subcutaneous skin flap, we now perform fat grafting as a preliminary operation, prior to proceeding with implant pocket conversion. Following fat grafting, patients should wait approximately 6–8 weeks before undergoing the second stage, implant pocket change operation.
Results
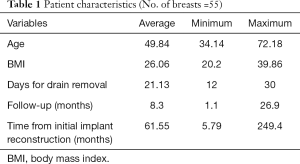
Thirty-one patients underwent 55 breast reconstruction revision operations for correction of animation deformity (Table 1). The average age was 49.84 and the average BMI was 26.06. Seven breasts had been previously irradiated. Patients underwent revision implant pocket change an average of 61.5 months after their initial submuscular breast reconstruction. In transitioning to a prepectoral plane, implants were upsized an average of 90.36 cc from their prior reconstruction volume.
Full table
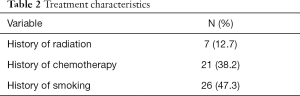
All patients achieved complete resolution of their animation deformity as a result of their implant pocket change operation (Tables 2,3). Patients were followed for an average of 8.3 months (range, 1.1–26.9 months) postoperatively.
Full table
Full table
Overall complication rates were assessed as part of this analysis (Table 4). Unplanned admission for intravenous antibiotics occurred in 14.5% of reconstructions. Eight (14.5%) reconstructions required reoperation. Four reoperations were for implant malposition, one for hematoma evacuation, and three for washout due to infection. One patient lost her implant as a result of infection. There were no reported incidences of seroma.
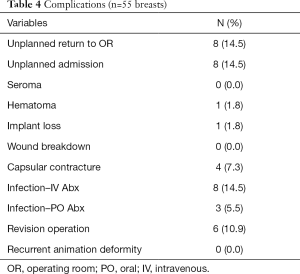
Full table
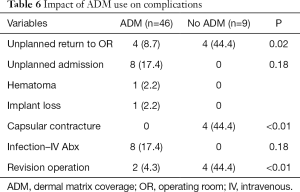
As our practice has grown, performing a complete ADM coverage of these implants has become our standard (Tables 5,6). Of note, nine reconstructions (16.4%) were performed with implant pocket change alone, without the use of ADM. This cohort had a 44.4% incidence of capsular contracture requiring reoperation as compared to zero instances of capsular contracture when ADM was employed (P<0.01).
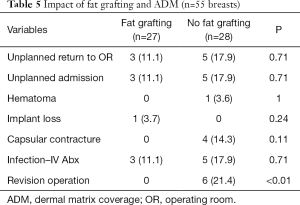
Full table
Full table
Additionally, 49% of our patients had undergone fat grafting prior to their implant pocket change procedure. The group that did no undergo fat grafting required additional revision operations for 21.4% of reconstructions as compared to 0% revisions performed on the group that had undergone fat grafting (P<0.01).
Discussion
Implant based breast reconstruction remains the most popular option for women undergoing post mastectomy breast reconstruction today (11). Traditionally, the implant is placed in the submuscular plane, deep to the pectoralis major muscle. A known consequence of this approach is the development of animation deformity. Without the breast parenchyma to separate the mastectomy skin from the pectoralis muscle, the skin becomes tethered to the underlying muscle. Any activation of the pectoralis can cause significant deformity of a patients’ chest, with lateral breast displacement (1,2).
Breast animation can be extremely bothersome to patients, and carry a negative implant on their daily quality of life. Nigro and Blanchet, in 2017, reported a large survey series of subpectoral reconstruction patients, in which patients reported their perception their own reconstructive outcomes. They found that 76% of patients surveyed were aware of their animation deformity, 26% rated their animation deformity as moderate or severe, and 52% would have preferred a technique eliminating it (2). These high rates of patient awareness towards animation deformity with subpectoral reconstruction indicate the highly beneficial aspects of the conversion operation from subpectoral to prepectoral. With this operation, all these patients reporting dissatisfaction with their animation, are given a surgical option for correction.
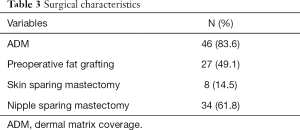
By repositioning the implant from the submuscular to a new prepectoral plane, anatomic separation of the contracting muscle from the overlying skin is restored, thus reversing the underlying etiology of the animation deformity (Figure 2). Reluctance towards prepectoral implant placement is largely credited to the high incidence of capsular contracture associated with subcutaneous breast reconstruction in the 1980s (12,13).

The acceptance of ADM has allowed plastic surgeons to revisit prepectoral implant placement with a significantly lower risk of developing capsular contracture. In a series of 1,584 reconstructions, Salzberg et al. showed a capsular contracture rate of 0.8% with ADM assisted direct to implant breast reconstruction (14).
Initial attempts to address animation deformity with prepectoral pocket conversion were described by Hammond et al. (9). In a series of 19 breasts, the authors performed implant pocket change to the prepectoral plane without the use of ADM. Similar to our series, all patients experienced complete resolution of their animation deformity postoperatively. However, their rate of capsular contracture requiring re-operative capsulectomy was 21.1%. Our rate of capsular contracture in our patients without the use of ADM was also high, at 44.4%.
Given the extremely high incidence of capsular contracture without the application of ADM, upon pocket conversion to the prepectoral plane, we now routinely perform complete ADM coverage of implants. Since employing this technique, our rate of capsular contracture has dropped to 0%. Our findings are supported by Gabriel et al. who similarly found complete resolution of animation deformity and no incidence of capsular contracture with ADM use in their large series (10).
Incidence of seroma is a complication often associated with the use of ADM. However, in our series, we did not experience any patients with seromas. We typically leave our breast drains in an average of 3 weeks in patients undergoing complete ADM coverage, which may contribute towards the absence of seromas in our cohort.
Notably our rate of admission for IV antibiotics, 14.5% is higher than other studies describing this operation. It has been our practice to treat prepectoral breast infections fairly aggressively and proactively. As a result, we have experienced only one case of a patient losing her reconstructed breasts due to infection. We found a trend towards a lower rate of infection in patients who underwent fat grafting prior to undergoing prepectoral conversion (11.1% vs. 17.9%, P=0.71).
Through performing several of these operations, the benefits of preemptive fat grafting have become more apparent. We have found that patients with a prior history of fat grafting have more robust skin flaps and more distinct planes between the pectoralis muscle and overlying subcutaneous tissue making for an easier and safer dissection. As such, we now incorporate fat grafting as a necessary step prior to performing prepectoral pocket change, in any patient deemed to have thin upper pole mastectomy skin flaps, identified by a pinch test less than 1 cm. Patients will typically wait a minimum of 6–8 weeks following fat grafting before proceeding with prepectoral pocket change.
Conclusions
Implant pocket conversion from the submuscular plane to the prepectoral plane is a safe and effective means of permanently correcting breast animation deformity. The application of preoperative fat grafting and perioperative ADM implant coverage contributes towards lower rates of complications and decreases the need for revision surgeries. The ability to offer surgical correction of animation deformity to our patient population has been extremely powerful, and allowed us to significantly enhance the satisfaction of our breast reconstruction patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. Sbitany is a consultant for Allergan, Inc. Other authors have no conflicts of interest to declare.
Ethical Statement: Patient medical records were reviewed for demographic information, perioperative details, and postoperative outcomes following approval from the University of California, San Francisco Institutional Review Board.
References
- Becker H, Fregosi N. The Impact of Animation Deformity on Quality of Life in Post-Mastectomy Reconstruction Patients. Aesthet Surg J 2017;37:531-6. [Crossref] [PubMed]
- Nigro LC, Blanchet NP. Animation Deformity in Postmastectomy Implant-Based Reconstruction. Plast Reconstr Surg Glob Open 2017;5:e1407. [Crossref] [PubMed]
- Figus A, Mazzocchi M, Dessy LA, et al. Treatment of muscular contraction deformities with botulinum toxin type A after latissimus dorsi flap and sub-pectoral implant breast reconstruction. J Plast Reconstr Aesthet Surg 2009;62:869-75. [Crossref] [PubMed]
- Jones G, Yoo A, King V, et al. Prepectoral Immediate Direct-to-Implant Breast Reconstruction with Anterior AlloDerm Coverage. Plast Reconstr Surg 2017;140:31S-8S. [Crossref] [PubMed]
- Sigalove S, Maxwell GP, Sigalove NM, et al. Prepectoral Implant-Based Breast Reconstruction and Postmastectomy Radiotherapy: Short-Term Outcomes. Plast Reconstr Surg Glob Open 2017;5:e1631. [Crossref] [PubMed]
- Highton L, Johnson R, Kirwan C, et al. Prepectoral Implant-Based Breast Reconstruction. Plast Reconstr Surg Glob Open 2017;5:e1488. [Crossref] [PubMed]
- Sbitany H, Piper M, Lentz R. Prepectoral Breast Reconstruction: A Safe Alternative to Submuscular Prosthetic Reconstruction following Nipple-Sparing Mastectomy. Plast Reconstr Surg 2017;140:432-43. [Crossref] [PubMed]
- Cheng A, Lakhiani C, Saint-Cyr M. Treatment of capsular contracture using complete implant coverage by acellular dermal matrix: a novel technique. Plast Reconstr Surg 2013;132:519-29. [Crossref] [PubMed]
- Hammond DC, Schmitt WP, O'Connor EA. Treatment of breast animation deformity in implant-based reconstruction with pocket change to the subcutaneous position. Plast Reconstr Surg 2015;135:1540-4. [Crossref] [PubMed]
- Gabriel A, Sigalove S, Sigalove NM, et al. Prepectoral Revision Breast Reconstruction for Treatment of Implant-Associated Animation Deformity: A Review of 102 Reconstructions. Aesthet Surg J 2018;38:519-26. [Crossref] [PubMed]
- Panchal H, Matros E. Current Trends in Postmastectomy Breast Reconstruction. Plast Reconstr Surg 2017;140:7S-13S. [Crossref] [PubMed]
- Slade CL. Subcutaneous mastectomy: acute complications and long-term follow-up. Plast Reconstr Surg 1984;73:84-90. [Crossref] [PubMed]
- Holzgreve W, Beller FK. Surgical complications and follow-up evaluation of 163 patients with subcutaneous mastectomy. Aesthetic Plast Surg 1987;11:45-8. [Crossref] [PubMed]
- Salzberg CA, Ashikari AY, Berry C, et al. Acellular Dermal Matrix-Assisted Direct-to-Implant Breast Reconstruction and Capsular Contracture: A 13-Year Experience. Plast Reconstr Surg 2016;138:329-37. [Crossref] [PubMed]


