Aesthetic Goldilocks mastectomy and breast reconstruction: promoting its use in the ideal candidate
The purpose of this article is to provide an experienced commentary on the aesthetic components of the Goldilocks mastectomy and single-stage reconstruction procedure based on our experience with 172 operations to date. Elements discussed include the history of the Goldilocks technique, ideal patient selection, operative technique, advantages and disadvantages of this approach to breast reconstruction compared to traditional techniques, and future directions for analyzing long-term outcomes of the Goldilocks approach to breast reconstruction. The authors advocate for its use in patients with higher-than-average risk factors for more extensive reconstructive techniques, as our institutional data have demonstrated safety, efficacy, and satisfactory aesthetic outcomes when using the Goldilocks technique. None of the authors have any conflicts of interest or financial support to disclose.
First described by Richardson and Ma in 2012 (1), the goal of the “Goldilocks mastectomy” was to provide completely autologous post-mastectomy reconstruction to patients by locally contouring native breast tissue. This was accomplished by preserving and de-epithelializing the residual mastectomy flap, creating a breast mound. The name Goldilocks embodies the simplicity of a single procedure with little down-time while still preserving a sufficient breast mound without an amputated appearance. This option is meant to be just right for select patients, rather than being too flat (traditional mastectomy) or too complex (microsurgical).
The ideal patient
Ideal candidates for aesthetic Goldilocks mastectomy procedures tend to be patients presenting with macromastia or severe breast ptosis, as these patients typically have redundant skin and adipose tissue remaining after mastectomy that are used to recreate a breast mound, improve contour, shape and improve the overall aesthetic appearance. Patients presenting with particular medical or surgical comorbidities [body mass index (BMI) >40, diabetes, immunosuppression, vascular insufficiency, etc.], or those who simply decline traditional approaches to breast reconstruction for personal reasons, can greatly benefit from Goldilocks mastectomy as a reconstructive option. The local contouring of native breast tissue with a de-epithelized flap of vascularized tissue and an internal dermal sling can improve breast support and enhance aesthetic outcomes in these patients (2,3). This technique has been described in a few small case series’ (2,3) and case reports (4-7) in patients who were poor candidates for traditional methods of reconstruction, such as implant-based or more complex autologous free flap reconstruction. The currently-growing body of literature has demonstrated positive results with the Goldilocks approach in a variety of patients, broadening the scope of potential candidates for post-mastectomy breast reconstruction.
Goals of aesthetic Goldilocks breast reconstruction
The Goldilocks approach to aesthetic breast reconstruction will provide a sufficient breast mound with variable degrees of projection depending upon the amount of tissue present in the native breast. This is not always meant to be a complete substitute for a formal breast reconstruction. In our practice, we often combine or build from an initial Goldilocks approach with adjuvant fat grafting or staged mastopexy to optimize the native breast mound after local contouring of the mastectomy flap. However, we commonly approach these cases as a modified mastopexy and local rearrangement of breast tissue in a single-stage. In addition, the resultant breast mound of locally-contoured native tissue lends well to staged nipple reconstruction. The Goldilocks approach is also an appealing alternative to near-total total mastectomy in the correct patient population who may be poor candidates for traditional reconstruction, or those patients who prefer a one-stage reconstruction without the time commitment and potential comorbidities of traditional multi-stage reconstruction. Furthermore, the Goldilocks approach can be a useful adjunct used in conjunction with implant-based reconstruction, providing a dermal sling to build an internal bra and scaffold for the implant.
Our experience to date: advantages and disadvantages
There is a significantly higher number of patients in our practice who undergo Goldilocks mastectomy and reconstruction who qualify as ‘morbidly obese’ (BMI >40) (Figure 1). Given the origins of the Goldilocks mastectomy technique in oncoplastic breast reconstruction cited above (predominantly being utilized in patients of higher BMI, as these patients tend to have more local residual breast tissue to create the autologous breast mound), this makes sense. From January 2012–January 2018, we have performed Goldilocks breast reconstruction for a total of 95 patients (172 breasts), qualifying as the largest account of cases to date. Mean age at the time of surgery was 55.8 [33–77] years, and mean BMI was 33.7 (19.2–54.6).
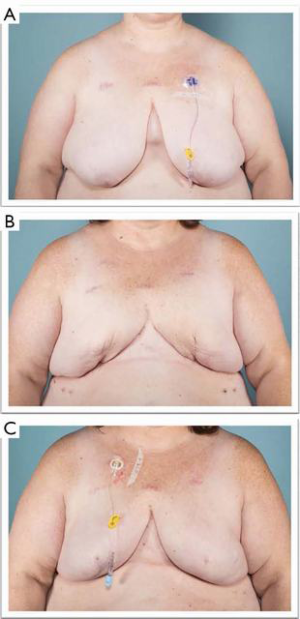
We find that the Goldilocks approach in the carefully selected patient provides a simple option (particularly for the obese patient with large, ptotic breasts not wanting implant or microsurgical reconstruction) to achieve the highest-possible aesthetic results with a short recovery time. The technique has limited application in small breasted or thin patients as the available tissue volume for local contouring is limited. If a large amount of skin needs to be removed from the upper pole, this can often result in aesthetically inferior results, in our experience. Our future studies analyzing our outcomes data with Goldilocks breast reconstruction will assess patient satisfaction using a validated scoring system such as BREAST-Q.
Conclusions
The observed results of this technique employed in our practice to date corroborate the consensus of the previously reported case reports and series’ that the Goldilocks approach is an excellent option for post-mastectomy reconstruction, particularly in conjunction with adjuvant, single-stage procedures such as fat grafting, mastopexy, implant, or tissue expander placement in the correct patient. We hope to encourage increased utility of this reconstructive method for the plastic surgeon to help the ideal candidate achieve aesthetically-superior results to traditional post-mastectomy outcomes in this patient population.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: The patient’s written informed consent was obtained for publication of these images.
References
- Richardson H, Ma G. The Goldilocks mastectomy. Int J Surg 2012;10:522-6. [Crossref] [PubMed]
- Schwartz JC. Goldilocks Mastectomy: A Safe Bridge to Implant-Based Breast Reconstruction in the Morbidly Obese. Plast Reconstr Surg Glob Open 2017;5. [Crossref] [PubMed]
- Ogawa T. Goldilocks mastectomy for obese Japanese females with breast ptosis. Asian J Surg 2015;38:232-5. [Crossref] [PubMed]
- Ter Louw RP, Bruce SB, Nahabedian MY. Partial Breast Reconstruction with Goldilocks Technique After Excision of Giant Fibroadenoma: A Case Report. Plast Reconstr Surg Glob Open 2017;5. [Crossref] [PubMed]
- Schwartz JD, Skowronksi PP. Extending the Indications for Autologous Breast Reconstruction Using a Two-Stage Modified Goldilocks Procedure: A Case Report. Breast J 2017;23:344-7. [Crossref] [PubMed]
- Schwartz JC, Skowronski PP. Case report of a definitive autologous reconstruction in a patient requiring immediate postoperative anticoagulation and reduced operative time. Int J Surg Case Rep 2016;25:86-8. [Crossref] [PubMed]
- Krishnan NM, Bamba R, Willey SC, et al. Explantation following nipple-sparing mastectomy: the Goldilocks approach to traditional breast reconstruction. Plast Reconstr Surg 2015;135:795e-6e. [Crossref] [PubMed]


