Robotic and endoscopic transoral thyroidectomy: feasibility and description of the technique in the cadaveric model
Introduction
Traditionally, thyroidectomy has been performed through a midline neck incision. It is a safe procedure with a permanent recurrent laryngeal nerve palsy rate of 2.3% (1) and permanent hypoparathyroidism rate of 1.9% (2). Despite its safety, the conventional technique is associated with a visible scar. Several studies have shown the impact of the thyroidectomy scar on the quality of life of patients (3,4). As a result, there has been considerable interest in finding ways of concealing the scar by utilizing smaller incisions (5) or moving the incision outside of the neck area by remote-access techniques.
Over the years, various endoscopic and robotic remote-access techniques have been developed to improve the cosmetic outcomes of thyroid surgery. These include thyroidectomy through chest (6), breast (7), axillary (8,9), bilateral axillo-breast (10), and retroauricular (11) incisions. Also, robotic facelift thyroidectomy, a procedure that combines thyroidectomy with retroauricular facelift to achieve superior cosmesis, has been described (12). However, despite improved cosmesis, all of these techniques require incisions on the skin. Furthermore, some of them require extensive tissue dissection to expose the thyroid gland from the remote access site and therefore, potentially compromise the minimally invasive nature of thyroid surgery.
Transoral thyroidectomy is a new concept that conceals the thyroidectomy scar by placing the incisions in the oral cavity. First described by Witzel et al. (13) in 2008, various techniques for transoral thyroidectomy have been proposed over the years. Using the transoral approach, it is possible to remove the thyroid gland through three or four incisions placed in the oral cavity. These incisions can all be placed in the oral vestibule (14) or a combination of oral vestibular and mouth floor incisions can be used (15,16). The procedure can be performed endoscopically (17) or robotically (18) depending on surgeon preference and expertise. Two recent clinical studies have indicated that transoral thyroidectomy can be safe and feasible (19,20).
This study reports the initial experience with transoral thyroidectomy at two academic US institutions using endoscopic and robotic techniques.
Methods
Robotic transoral thyroidectomy
A male cadaver with full dentition was obtained from Cleveland Clinic Center for Multidisciplinary Simulation. The vestibular approach previously described by Park et al. (21) was utilized.
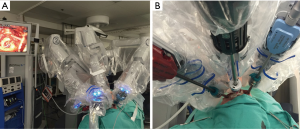
The cadaver was placed supine and the neck was extended. Pre-resection ultrasound revealed a normal-sized thyroid gland and no nodules. A 2-cm incision was made in the midline in the oral vestibule. Blunt dissection was carried towards the submental space along the mandibular periosteum. Once the submental space was reached and a pocket was created, working space was expanded by blunt dissection. Then, a 12-mm port was inserted, and the submental pocket was further expanded by CO2 insufflation at 6 mmHg. Then, two additional incisions were made in the mucosa on both sides at the level of the first molars. These two pouches were connected to the submental pouch by blunt dissection. Care was taken to identify and preserve the mental nerves. After connection to the submental pouch, two 8-mm ports were inserted into the lateral pockets (Figure 1).

After creation of the working space, the da Vinci surgical system (Intuitive Surgical Inc., Sunnyvale, CA, USA) was brought in from the head of the bed and docked. A 30-degree down-looking camera was introduced through the midline port, a robotic Maryland bipolar forceps through the left, and a harmonic scalpel through the right port (Figure 2). To maintain adequate working space, insufflation at 6 mmHg was used. In addition, traction sutures were placed on the neck skin as described by Dionigi et al. (22) to elevate the flap (Figure 3).

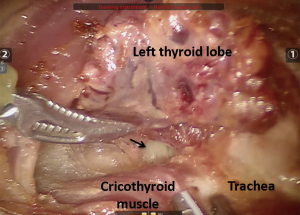
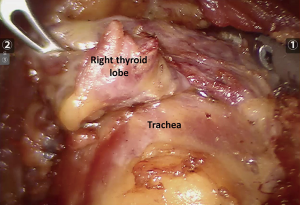
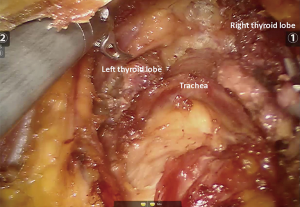
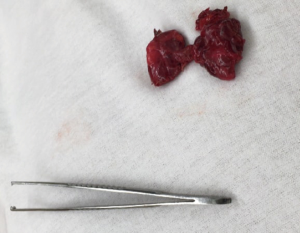
With the help of the robotic instruments, dissection was continued down to the level of the thyroid cartilage in a subplatysmal fashion. The strap muscles were identified and divided at the midline raphe to expose the thyroid gland. The thyroid was divided at the isthmus. First, the left lobe was excised with the help of the energy device. The recurrent laryngeal nerve and parathyroid glands were identified and preserved during dissection (Figure 4). The contralateral right thyroid lobe was excised in a similar fashion (Figure 5). The specimen was removed through the midline incision for the camera port (Figure 6). Total operative time was 2 hours.
Endoscopic transoral thyroidectomy
A male cadaver was provided for this procedure by Tulane University School of Medicine. The cadaver was placed supine on the operating table and draped below the neck with the neck in an extended position. A 10-mm horizontal incision was made in the alveolar mucosa of the lower lip opposite to the central incisors. Electrocautery was used to create operative space in a caudal direction into the neck region. Kelly clamp was used to aid with dissection and retraction of the digastric muscle. A 10-mm trocar was then passed over the mandible and into the anterior neck with care to avoid penetration of the mentum skin. Carbon dioxide insufflation of 6 mmHg was used. Two vertical incisions of 5 mm were then made in the vestibular mucosa medial to the level of the canines, to avoid injury to the mental nerve (Figure 7).

A 30-degree endoscope was placed through the main incision, and two 5 mm ports were used through the lateral incisions for instrument placement. Maryland dissector (Intuitive Surgical, Sunnyvale, CA, USA) and LigaSure Vessel Sealing System (Covidien, Mansfield, MA, USA) were used. Further dissection was carried out in the subplatysmal space to the sternal notch. Operative space was expanded laterally to the anterior borders of the sternocleidomastoid muscle. Strap muscles were then visualized and divided in the midline for thyroid gland exposure. Hanging sutures were placed for strap muscle retraction. We then divided the middle thyroid vein on the right side followed by division of the superior thyroid vessels, with care taken to avoid the external branch of the superior laryngeal nerve. The superior lobe was mobilized and the recurrent laryngeal nerve was identified. The inferior thyroid vessels were divided. Thyroid lobe was then mobilized. Care was taken to avoid injury to the recurrent laryngeal nerve. Parathyroid glands were carefully identified and preserved, and their blood supply kept intact. Similar technique was then used to mobilize the left thyroid lobe. The thyroid gland was then lifted anteriorly and berry’s ligament was transected. Specimen was extracted in an Endocatch bag through the central port (Figure 8).
Results
Total thyroidectomy was successfully performed transorally with both endoscopic and robotic techniques. In both procedures, bilateral recurrent laryngeal nerves and all four parathyroid glands were visualized and preserved. In the endoscopic removal, bilateral mental nerves were also identified and preserved (Figure 9). Postoperatively, the mentum and the anterior cervical skin were observed to retain the original appearance and elasticity (Figure 10). The operative times were 120 minutes for the robotic and 100 minutes for the endoscopic procedure.


Discussion
Overall, the procedure was found feasible given the direct access it provides into the neck without excessive trauma to the surrounding tissues. Obviously, the biggest advantage of this technique was the avoidance of a visible scar in the neck.
On the other hand, we had some concerns. First one was about the possible introduction of oral infectious agents into the neck. However, two recent clinical studies indicated otherwise. Anuwong reported no surgical site infection in a 60-patient series (19). Similarly, Park and Sun reported no infections in a study of 18 transoral thyroidectomies (20). Our second concern was about the possible deviation from surgical oncologic principles with the extraction of larger tumors. In our experience, we had to divide the thyroid gland for laparoscopic removal through the midline incision. Nakajo et al. reported three papillary thyroid cancers removed transorally as part of their 8-patient series. However, they did not specify tumor sizes or the details of removal (23). Park and Sun reported 11 papillary and 1 follicular thyroid cancers operated transorally. Specimens were removed endoscopically. Despite successful removal of benign tumors as large as 7.5 cm, no malignant tumor larger than 2.5 cm was approached transorally (20). Another concern was about the risk of damage to the skin of the mentum and the anterior neck, and the resulting loss of elasticity of the skin. Finally, we had concerns about the adequacy of exposure. Our groups have had long-term experience in another remote-access technique, transaxillary thyroidectomy (24-26). Despite the direct access into the neck, in our opinion, dissection of the lateral borders of the thyroid lobes was more difficult in the transoral compared to the axillary approach. For better exposure in transoral approach, Anuwong recommended use of external traction sutures placed on the strap muscles (19).
Several technical considerations should be taken during the conduct of the procedure. To avoid puncturing the cervical skin, blunt dissection should be carried with tactile feedback. Furthermore, during dissection, the instruments should be kept medial to the canine teeth to avoid damage to the mental nerves. In our cadaveric experience, CO2 insufflation and physical traction were used for flap creation and elevation of the anterior cervical skin. However, it may be possible to perform the procedure with a gasless technique with only physical traction.
Conduct of transoral thyroidectomy requires placement of three trocars in a relatively small surgical space. Unlike endoscopic technique, the robotic system provides articulating instruments and a stable camera platform. It minimizes port manipulations due to improved ergonomics and superior maneuverability. In clinical practice, this may translate into less trauma to the surrounding tissues and less postoperative pain compared to endoscopic technique. Despite lacking some advantages provided by the surgical platform, laparoscopic technique is also feasible and may constitute a cheap cosmetic alternative to the Kocher incision. Clinical studies analyzing both techniques are needed to determine which technique is better for transoral approach.
In conclusion, this study reports the initial experience with transoral thyroidectomy at two US academic institutions with robotic and endoscopic techniques. With superior cosmetic outcomes, this new approach may be more widely implemented in the future and prove to be a valid alternative to conventional thyroid surgery.
Review of the literature
Transoral thyroid resection was first described by Witzel et al. in 2008 (13). In this proof-of-concept study, a new hybrid sublingual-skin technique was developed in two human cadavers and ten living pigs. For the removal of the thyroid, a central 15 mm infralingual incision in the mouth and an additional 3.5 mm skin incision below the larynx were used. The pigs were observed for 2 hours after completion of the procedure without any complication. Recurrent laryngeal nerve function was shown to be intact after resection by neuromonitoring in all pigs.
In 2009, Benhidjeb et al. described totally transoral video-assisted thyroidectomy (TOVAT) in a study of five human cadavers (15). The technique was developed in three cadavers, and TOVAT itself was tested in two cadavers. TOVAT was a hybrid mouth floor-oral vestibule technique, and was performed using one 5-mm sublingual and two 3-mm vestibular trocars. One-sided subtotal thyroidectomy could be performed within 60 minutes without damage to vital structures. It had better cosmetic outcome than the previous method as all the incisions were concealed in the oral cavity.
Wilhelm et al. described another hybrid mouth floor-vestibular transoral thyroidectomy technique, endoscopic minimally invasive thyroidectomy (eMIT), in 2010 (27). Later same year, they reported the first clinical application of this technique in a 53-year-old man (28). The patient had no complications except for minimal neck swelling and hematoma. Given the initial positive experience with eMIT, a prospective clinical study was conducted in eight patients undergoing total and subtotal thyroidectomies (17). Three cases were converted to open due to large tumor size. Six mental nerve and two recurrent laryngeal nerve palsies were noted. One recurrent laryngeal nerve palsy was permanent, while the other seven palsies resolved on follow-up.
Karakas et al. described transoral endoscopic thyroid and parathyroid surgery in 2010 (16). The thyroid gland was accessed by placing a modified rigid rectoscope through a 20-mm paralingual incision. Dissection was performed using 5-mm laparoscopic instruments. With this technique, hemithyroidectomy was performed first in ten pig cadavers, then in ten living pigs. Next, in five human cadavers, both thyroid and parathyroid resections were performed. No complications were observed and all cases could be completed transorally. The same group further developed their surgical technique in 2011 (29). Using a special cervicoscope, transoral hemithyroidectomy was performed in ten living pigs and transoral parathyroidectomy in two patients. Pigs were followed for 14 days postoperatively and then underwent autopsy. All ten pigs had normal postoperative recovery and no evidence of infection on autopsy. Next, transoral parathyroidectomy was performed in two patients with preoperatively localized parathyroid adenoma. One patient experienced transient right hypoglossal nerve palsy. In 2014, as a follow-up on this study, Karakas et al. planned a 10-patient prospective pilot study to better assess the utility of transoral parathyroidectomy (30). Only five patients could be recruited and 2 of the 5 operations had to be converted to open. Complications included 1 permanent lingual nerve palsy, 1 transient recurrent laryngeal nerve palsy, 1 transient hypoglossal nerve palsy, and 3 hematomas of the mouth floor. Transoral parathyroidectomy was found not feasible by the authors.
In 2011, Richmon et al. performed robotic transoral thyroidectomy in two cadavers (31). Using a hybrid sublingual-buccal technique and the da Vinci surgical system (Intuitive Surgical Inc.), they successfully removed the thyroid gland without damage to the surrounding structures. Later same year, the same group described the technique for robotic-assisted transoral central lymph node dissection (18). For this study, instead of a hybrid sublingual-buccal technique, all three incisions were placed in the gingival-buccal sulcus. This approach, according to the authors, provided better view of the central neck compared with the previous technique.
In 2013, Nakajo et al. developed transoral video-assisted neck surgery (TOVANS), a new gasless technique for endoscopic transoral thyroidectomy (23). TOVANS was a vestibular technique that used a premandibular and subplatysmal tunnel to access the thyroid gland. Instead of CO2 insufflation, working space was maintained by lifting the cervical skin using Kirschner wires. A total of 8 patients underwent TOVANS including 3 papillary microcarcinomas requiring central lymph node dissection. Sensory disorder around the chin persisted at 6 months in all patients. One patient had recurrent laryngeal nerve palsy. With 3-day antibiotic use, no patient had surgical site infections.
Wang et al. compared endoscopic thyroidectomy with oral vestibular approach (ETOVA) to endoscopic thyroidectomy with areolar approach in a randomized clinical comparative study in 2014 (14). Twelve patients were randomized to each group. Operative time, blood loss, postoperative hospital-stay, and cost of surgery were similar between groups. Patient satisfaction score was higher with ETOVA (2.33 vs. 1.58) on follow-up at 6 months given superior cosmetic outcomes. No recurrent laryngeal nerve injury or hypoparathyroidism was observed in any group.
Lee et al. described endoscopic transoral periosteal thyroidectomy (TOPOT) in seven living pigs in 2014 (32). Four of the seven pigs were operated with a four-port technique and three with a three-port technique. All incisions were made in the mandibular periosteum, preventing mentalis muscle transection and Wharton’s duct injury. Three-port technique was performed with a central 2 cm incision on the buccal surface of the central incisors and two 0.8 cm gingival-buccal sulcus incisions at the level of the first molars. For the four-port technique, an additional 1.5 cm midline incision was made on the lingual side. Total thyroidectomy was completed successfully in all seven pigs without any intraoperative complications and with normal 7-day postoperative recovery. Same group later described how to perform TOPOT on da Vinci surgical system (Intuitive Inc.) (33), and using this robotic technique, operated on four patients (34). Three patients had transient paresthesia of the mental nerve. There were otherwise no complications.
Park et al. described the trivestibular route for transoral endoscopic thyroidectomy in 2014 (21). This is the same approach we used in this study. In 2016, they performed the first clinical application of this technique (35). A 30-year-old female underwent transoral thyroidectomy without any complication. Recently, Park and Sun reported a study of 18 thyroidectomies using this technique (20). In this study, tumors as large as 7.5 cm were successfully removed transorally. Postoperative complications included 2 seromas and 1 transient hypocalcemia. No permanent recurrent laryngeal nerve palsy or surgical site infection was observed.
The largest clinical experience with transoral thyroidectomy to date was reported by Anuwong in 2016 (19). In this study of 60 patients, mean tumor size was 5.4 cm and tumors as large as 10 cm were removed successfully via the vestibular approach. The median operative time was 90 and 135.5 minutes for hemithyroidectomy and bilateral thyroidectomy, respectively. Postoperative complications included 3 temporary hypoparathyroidisms, 2 temporary recurrent laryngeal nerve palsies, and 1 hematoma.
Recently, Udelsman et al. reported the clinical application of transoral approach in the US in a study of seven patients (36). Five patients underwent thyroid surgery, while the remaining two underwent parathyroidectomy. Mean operative time was 222 minutes with a mean length of hospital stay of 1 day. No complications were encountered.
Conclusions
In conclusion, we hereby report our initial experience with transoral thyroidectomy at two academic US institutions, along with a review of the current literature. Despite certain limitations, this technique may help achieve superior cosmetic outcome. With growing interest, more clinical studies are indicated to fully elucidate its potentials and limitations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jeannon JP, Orabi AA, Bruch GA, et al. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract 2009;63:624-9. [Crossref] [PubMed]
- Almquist M, Hallgrimsson P, Nordenstrom E, et al. Prediction of permanent hypoparathyroidism after total thyroidectomy. World J Surg 2014;38:2613-20. [Crossref] [PubMed]
- Arora A, Swords C, Garas G, et al. The perception of scar cosmesis following thyroid and parathyroid surgery: a prospective cohort study. Int J Surg 2016;25:38-43. [Crossref] [PubMed]
- Lee S, Kim HY, Lee CR, et al. A prospective comparison of patient body image after robotic thyroidectomy and conventional open thyroidectomy in patients with papillary thyroid carcinoma. Surgery 2014;156:117-25. [Crossref] [PubMed]
- Miccoli P, Berti P, Conte M, et al. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 1999;22:849-51. [Crossref] [PubMed]
- Shimizu K, Akira S, Jasmi AY, et al. Video-assisted neck surgery: endoscopic resection of thyroid tumors with a very minimal neck wound. J Am Coll Surg 1999;188:697-703. [Crossref] [PubMed]
- Ohgami M, Ishii S, Arisawa Y, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 2000;10:1-4. [Crossref] [PubMed]
- Ikeda Y, Takami H, Niimi M, et al. Endoscopic thyroidectomy by the axillary approach. Surg Endosc 2001;15:1362-4. [Crossref] [PubMed]
- Kang SW, Jeong JJ, Nam KH, et al. Robot-assisted endoscopic thyroidectomy for thyroid malignancies using a gasless transaxillary approach. J Am Coll Surg 2009;209:e1-7. [Crossref] [PubMed]
- Lee KE, Rao J, Youn YK. Endoscopic thyroidectomy with the da Vinci robot system using the bilateral axillary breast approach (BABA) technique: our initial experience. Surg Laparosc Endosc Percutan Tech 2009;19:e71-5. [Crossref] [PubMed]
- Byeon HK, Holsinger FC, Tufano RP, et al. Robotic total thyroidectomy with modified radical neck dissection via unilateral retroauricular approach. Ann Surg Oncol 2014;21:3872-5. [Crossref] [PubMed]
- Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: II. Clinical feasibility and safety. Laryngoscope 2011;121:1636-41. [Crossref] [PubMed]
- Witzel K, von Rahden BH, Kaminski C, et al. Transoral access for endoscopic thyroid resection. Surg Endosc 2008;22:1871-5. [Crossref] [PubMed]
- Wang C, Zhai H, Liu W, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery 2014;155:33-8. [Crossref] [PubMed]
- Benhidjeb T, Wilhelm T, Harlaar J, et al. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc 2009;23:1119-20. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral thyroid and parathyroid surgery. Surg Endosc 2010;24:1261-7. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg 2011;35:543-51. [Crossref] [PubMed]
- Richmon JD, Holsinger FC, Kandil E, et al. Transoral robotic-assisted thyroidectomy with central neck dissection: preclinical cadaver feasibility study and proposed surgical technique. J Robot Surg 2011;5:279-82. [Crossref] [PubMed]
- Anuwong A. Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Park JO, Sun DI. Transoral endoscopic thyroidectomy: our initial experience using a new endoscopic technique. Surg Endosc 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Park JO, Kim CS, Song JN, et al. Transoral endoscopic thyroidectomy via the tri-vestibular routes: results of a preclinical cadaver feasibility study. Eur Arch Otorhinolaryngol 2014;271:3269-75. [Crossref] [PubMed]
- Dionigi G, Bacuzzi A, Lavazza M, et al. Transoral endoscopic thyroidectomy via vestibular approach: operative steps and video. Gland Surg 2016;5:625-7. [Crossref] [PubMed]
- Nakajo A, Arima H, Hirata M, et al. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc 2013;27:1105-10. [Crossref] [PubMed]
- Foley CS, Agcaoglu O, Siperstein AE, et al. Robotic transaxillary endocrine surgery: a comparison with conventional open technique. Surg Endosc 2012;26:2259-66. [Crossref] [PubMed]
- Aliyev S, Taskin HE, Agcaoglu O, et al. Robotic transaxillary total thyroidectomy through a single axillary incision. Surgery 2013;153:705-10. [Crossref] [PubMed]
- Kandil EH, Noureldine SI, Yao L, et al. Robotic transaxillary thyroidectomy: an examination of the first one hundred cases. J Am Coll Surg 2012;214:558-64; discussion 564-6. [Crossref] [PubMed]
- Wilhelm T, Harlaar JJ, Kerver A, et al. Surgical anatomy of the floor of the oral cavity and the cervical spaces as a rationale for trans-oral, minimal-invasive endoscopic surgical procedures: results of anatomical studies. Eur Arch Otorhinolaryngol 2010;267:1285-90. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Video. Endoscopic minimally invasive thyroidectomy: first clinical experience. Surg Endosc 2010;24:1757-8. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral thyroid and parathyroid surgery--development of a new transoral technique. Surgery 2011;150:108-15. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral parathyroid surgery--a new alternative or nonsense? Langenbecks Arch Surg 2014;399:741-5. [Crossref] [PubMed]
- Richmon JD, Pattani KM, Benhidjeb T, et al. Transoral robotic-assisted thyroidectomy: a preclinical feasibility study in 2 cadavers. Head Neck 2011;33:330-3. [PubMed]
- Lee HY, Hwang SB, Ahn KM, et al. The safety of transoral periosteal thyroidectomy: results of Swine models. J Laparoendosc Adv Surg Tech A 2014;24:312-7. [Crossref] [PubMed]
- Lee HY, Richmon JD, Walvekar RR, et al. Robotic transoral periosteal thyroidectomy (TOPOT): experience in two cadavers. J Laparoendosc Adv Surg Tech A 2015;25:139-42. [Crossref] [PubMed]
- Lee HY, You JY, Woo SU, et al. Transoral periosteal thyroidectomy: cadaver to human. Surg Endosc 2015;29:898-904. [Crossref] [PubMed]
- Park JO, Kim MR, Kim DH, et al. Transoral endoscopic thyroidectomy via the trivestibular route. Ann Surg Treat Res 2016;91:269-72. [Crossref] [PubMed]
- Udelsman R, Anuwong A, Oprea AD, et al. Trans-oral vestibular endocrine surgery: a new technique in the United States. Ann Surg 2016;264:e13-6. [Crossref] [PubMed]


