Development of a surgical algorithm by using pre-operative imaging to predict mammoplasty cosmetic outcomes for large non-malignant tumours
Introduction
Large non-malignant tumours, such as giant fibroadenomas, phyllodes tumours and giant lipomas, are rare (1-3) and often cause breast distortion and asymmetry. Although these tumours are non-malignant, surgical excision is the mainstay of treatment for these masses.
Mammoplasty, which involves the use of volume displacement techniques, has been reported to successfully remove large non-malignant tumours with good cosmetic outcomes (4,5). However, data from the literature is sparse. There is, to date, no known study on what is the optimal tumour to breast size ratio cut-off in this group of patients undergoing mammoplasty, beyond which could result in a compromise of the postoperative cosmetic outcome.
We aim to determine the optimal tumour to breast size ratio cut-off in patients, with large non-malignant tumours undergoing mammoplasty, which could achieve satisfactory cosmetic outcomes.
Methods
Patients who underwent mammoplasty by a single surgeon from May 2014 to June 2017 for biopsy-proven large non-malignant tumours were included in the study. These patients were also offered mastectomy with reconstruction as an alternative option but declined. The demographics, tumour to breast size ratios based on imaging, histological features and cosmetic outcomes of these patients were assessed.
These patients were selected because they all had visible breast asymmetry arising from the large non-malignant mass that would concomitantly need some form of redundant skin excision post-tumour removal.
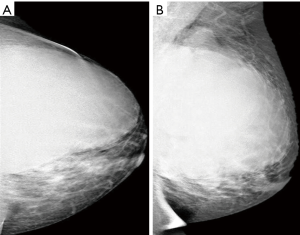
The tumour to breast size ratio assessment was made on 2 dimensional (2D) ultrasound and mammogram images where available. Ultrasound volume estimation was based on the four quadrant scans of the breasts in the transverse and longitudinal planes. Mammogram size estimation was performed using standard craniocaudal and mediolateral mammographic projections. The tumour to breast size ratio was then visually estimated in ten percentile intervals. This assessment was performed by a dedicated breast-imaging radiologist with 10 years of imaging experience who was blinded to the post-operative cosmetic outcome of the patients.
The choice of mammoplasty technique was individualised and depended on various factors such as the patient’s breast size, grade of ptosis, tumour size, tumour location and the degree of asymmetry at presentation. The incision was planned so as to remove the tumour en-bloc with a margin of normal breast tissue wherever possible, excise the post-excision residual skin, re-shape the remaining breast tissue, re-size and reposition the nipple areolar complex. The aim of the surgery was primarily to avoid deformity of the operated breast post safe removal of the tumour with the secondary aim of achieving symmetry with the contralateral normal breast as much as possible.
A margin of normal tissue was obtained in all patients as it has been shown that it can be challenging to distinguish giant fibroadenoma from phyllodes based on core needle biopsy (6) and treatment guidelines have advocated resection of phyllodes with a wide margin to reduce the recurrence rate (2,6).
The cosmetic outcome was assessed by the patient and surgeon respectively using a 4 point scale of excellent, good, fair and poor. Excellent score was rated when there was no or slight asymmetry of the breasts postoperatively, good when there was some asymmetry but no deformity on the operated breast, fair when there was marked asymmetry and/or some deformity of the operated breast and poor when there was marked deformity of the operated breast. The combined mean cosmetic score was then calculated.
This study was approved by Singhealth Centralised Institutional Review Board.
Results
Ten patients were included in the study. The median age was 40 years old (range, 14–55 years). All were non-smokers. Five patients had coexisting comorbidities, of which hypertension and hyperlipidemia were the commonest. Five patients had grade I ptosis while the remaining patients had grades II and III ptosis.
All the patients had preoperative ultrasound breast assessment and five patients also had mammograms. Based on imaging, the median tumour to breast size ratio was 55% (range, 20–90%).
Histology revealed phyllodes tumour and giant fibroadenoma in six and four patients respectively. For the patients with phyllodes, two had benign phyllodes while the rest had borderline phyllodes. Margins were clear in all cases. Two patients with borderline phyllodes underwent adjuvant radiotherapy. One of these patients had incidental 1 mm low grade ductal carcinoma in situ (DCIS) in the breast tissue surrounding the tumour which was completely excised.
Mean weight and average maximum size of surgical specimen were 357.9 g (range, 28–1,186 g) and 99.3 mm (range, 35–165 mm) respectively.
Five patients underwent round block mammoplasty, one had vertical mammoplasty and four had wise pattern mammoplasty. The nipple areolar complex was preserved in all cases. One patient developed partial nipple necrosis which resolved with conservative management.
Mean cosmetic score was excellent and good in all patients except for one patient with a fair outcome. This particular patient received adjuvant radiotherapy and also had the highest estimated tumour to breast size ratio of 90% while the rest of the patients had an estimated tumour to breast size ratio of 20–70%.
The patients were followed up for a median period of 12.5 months (range, 0.5–35 months) and there was no known recurrence.
Discussion
While it is known that the post-operative breast cosmetic outcome is highly dependent on the volume of breast resected (7), there is no data on the maximal tumour to breast size ratio cut-off beyond which cosmetic outcome in patients with large non-malignant tumours undergoing mammoplasty would have a poor cosmetic outcome. To our knowledge, this is the first study which evaluated the impact of the tumour to breast size ratio on the cosmetic outcome in this group of patients. Our study showed that mammoplasty can be performed successfully in patients with a tumour to breast size ratio of up to 70% with a good cosmetic outcome.
Various surgical techniques for the excision of large non-malignant breast tumours have been described which include excision via the inframammary approach (8), mammoplasty (4,5), ‘swiss roll’ operation (9), periareolar with extension (10), etc. Each technique has its own merits and disadvantages. Mammoplasty, in particular, has been shown to be very useful in patients with significant asymmetry arising from the large benign mass compared to the inframammary approach (11). This is because mammoplasty has the advantage of removing the resultant redundant skin concomitantly following tumour excision which helps to restore breast symmetry.
As these large benign tumours often occur in young women, excision with breast conservation is desired. However, not all patients can undergo excision of the large benign mass while conserving the rest of the breast to achieve a safe resection margin and good cosmetic outcome. This is especially true in patients with a very high tumour to breast size ratio. As a result, mastectomy with or without reconstruction (6,12) or excision with concomitant partial volume replacement flaps (3) had been described in the literature. In some cases, a contralateral breast operation may be needed for symmetricalisation.
From the results, a surgical algorithm involving mastectomy with or without reconstruction or excision with concomitant partial volume replacement flaps for patients with tumour to breast size ratio of more than 70% may be proposed. This algorithm will be useful in the preoperative planning for such patients which in turn will lead to a better cosmetic outcome. The findings also provide some guidance for the surgical options when clinicians discuss the management of large non-malignant breast tumour with their patients.
In contrast to breast cancer where mastectomy is advocated in cases found to have a tumour to breast size ratio that is greater than 50% (13), our study’s cut-off ratio of more than 70% may appear excessive. However, our study differed in that all our patients presented initially with a much bigger, asymmetrical breast. After removal of the large non-malignant mass which accounted most of the asymmetry, we found that in these originally larger breasts, a residual volume of 30% or more could be reshaped with mammoplasty to avoid deformity of the breast, giving a good cosmetic outcome.
However, our study was not without limitations. It was a small retrospective study. This was attributed to the fact that the prevalence of patients presenting with large benign breast mass was low. To date, there were less than 200 cases of giant benign breast masses reported in literature with most studies being case reports or series of limited patients.
We measured the tumour to breast size ratio in ten percentile intervals and there were no patients, in our study, with the tumour to breast size ratio between 70–90%, hence we are unable to comment on the effect of this particular ratio on the cosmetic outcome.
Data from mammographic assessment was limited because many of the patients in the series were young. Mammography is rarely performed in this age group due to its lack of diagnostic sensitivity and the increased radio-sensitivity of breast tissue in young women. For the ultrasound modality, tumour and breast size estimation obtained from the static 2D ultrasound images would be expected to be fairly imprecise. This is because the static 2D images were only obtained in a few segments of the mass and much of the tumour and breast would not be captured on ultrasound imaging for measurement. Ultrasound assessment was also heavily operator dependent with the tumour dimensions reliant on how the operator obtained the images. Despite these limitations, mammogram and ultrasound remain the main imaging modalities in clinical practice for assessment of large non-malignant masses. Hence our study, using ultrasound with or without mammography assessment, can provide the surgeon with a good preoperative estimate of the tumour to breast size ratio and aid in the subsequent surgical management.
Ideally, the volumetric assessment of the tumour and breast size is best measured with cross-sectional imaging. Magnetic resonance imaging (MRI) has been shown to be the most accurate method to measure breast volume (14). The MRI 3 dimensional (3D) volume imaging provides a more complete visual assessment of the tumour size relative to that of the breast. Computer-aided detection (CAD) software can also be employed to objectively measure the volumes of the breast and the tumour to derive the tumour to breast size ratio. The MRI derived ratio has been shown to be able to predict cosmetic outcome accurately after breast conserving surgery (15). However, MRI is relatively costly and there is currently no recognised role for MRI imaging for the assessment of benign breast lesions. Automated ultrasound 3D scan is an emerging modality in breast imaging which has the potential to accurately measure breast and tumour volumes (16). Multiple 2D slices of almost the entire breast are acquired from an automated scanning probe. The images then undergo 3D reconstruction by an imaging software and volumetric assessments can be made on an ultrasound viewer workstation. Software capability to automatically calculate volume measurements of the breast and the tumour mass are being developed. However, as this is a relatively recent development, there is little data on the accuracy of the volumetric calculations derived from ultrasound 3D imaging.
In our study, two patients with borderline phyllodes received radiotherapy, including the patient who had the highest tumour to breast size ratio of 90% who had a fair cosmetic outcome. The indication of radiotherapy in patients with borderline phyllodes remained controversial (17) and radiotherapy may have arguably affected the cosmetic outcome (18). However, the cosmetic outcome was reported to be good in the other patient with a tumour to breast size of 70% who also received radiotherapy (Figures 1-4). Hence, radiotherapy may not be a significant factor, in our study, affecting cosmetic outcome.


In conclusion, mammoplasty can be used successfully in patients with large non-malignant tumours. However, in patients with tumours occupying more than 70% of the breast, mammoplasty alone may not yield a good cosmetic outcome. The findings should be validated with larger prospective studies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by Singhealth Centralised Institutional Review Board (No. 2017/2093).
References
- Chepla KJ, Armijo BS, Ponsky TA, et al. Benefits of immediate dermoglandular preserving reconstruction following giant fibroadenoma excision in two patients. J Plast Reconstr Aesthet Surg 2011;64:e244-7. [Crossref] [PubMed]
- Guillot E, Couturaud B, Reyal F, et al. Management of phyllodes breast tumors. Breast J 2011;17:129-37. [Crossref] [PubMed]
- Bonomi S, Salval A, Settembrini F, et al. Breast reshaping with dermaglandular flaps after giant lipoma removal: versatility of oncoplastic techniques. Aesthetic Plast Surg 2012;36:355-8. [Crossref] [PubMed]
- Achebe JU, Njeze GE, Okwesili OR. Treatment of unilateral giant fibroadenoma by breast reduction skin incision: the inverted "T" technique. Niger J Clin Pract 2014;17:43-6. [Crossref] [PubMed]
- Beier JP, Jaeger K, Horch RE. Reduction mammaplasty for benign phyllodes tumour in an adolescent female--a 13-year follow up. Breast 2006;15:550-3. [Crossref] [PubMed]
- Chirappapha P, Lertsithichai P, Sukarayothin T, et al. Oncoplastic techniques in breast surgery for special therapeutic problems. Gland Surg 2016;5:75-82. [PubMed]
- Franceschini G, Martin Sanchez A, Di Leone A, et al. New trends in breast cancer surgery: a therapeutic approach increasingly efficacy and respectful of the patient. G Chir 2015;36:145-52. [PubMed]
- Hille-Betz U, Klapdor R, Henseler H, et al. Treatment of Giant Fibroadenoma in Young Women: Results after Tumor Excision without Reconstructive Surgery. Geburtshilfe Frauenheilkd 2015;75:929-34. [Crossref] [PubMed]
- Naraynsingh V, Maharaj D, Rampaul R. "Swiss-roll" operation for giant fibroadenomas. Breast J 2002;8:45-6. [Crossref] [PubMed]
- Sosin M, Feldman E. Giant juvenile fibroadenoma: a case and review of novel modalities in treatment. Breast Dis 2012;34:35-8. [Crossref] [PubMed]
- Ugburo AO, Olajide TO, Fadeyibi IO, et al. Differential diagnosis and management of giant fibroadenoma: comparing excision with reduction mammoplasty incision and excision with inframammary incision. J Plast Surg Hand Surg 2012;46:354-8. [Crossref] [PubMed]
- Dolmans GH, Hoogbergen MM, van Rappard JH. Giant fibroadenoma of one breast: Immediate bilateral reconstruction. J Plast Reconstr Aesthet Surg 2007;60:1156-7. [Crossref] [PubMed]
- Clough KB, Kaufman GJ, Nos C, et al. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol 2010;17:1375-91. [Crossref] [PubMed]
- Choppin SB, Wheat JS, Gee M, et al. The accuracy of breast volume measurement methods: A systematic review. Breast 2016;28:121-9. [Crossref] [PubMed]
- Faermann R, Sperber F, Schneebaum S, et al. Tumor-to-breast volume ratio as measured on MRI: a possible predictor of breast-conserving surgery versus mastectomy. Isr Med Assoc J 2014;16:101-5. [PubMed]
- Narayanasamy G, LeCarpentier GL, Roubidoux M, et al. Spatial registration of temporally separated whole breast 3D ultrasound images. Med Phys 2009;36:4288-300. [Crossref] [PubMed]
- Zeng S, Zhang X, Yang D, et al. Effects of adjuvant radiotherapy on borderline and malignant phyllodes tumors: A systematic review and meta-analysis. Mol Clin Oncol 2015;3:663-71. [Crossref] [PubMed]
- Taylor ME, Perez CA, Halverson KJ, et al. Factors influencing cosmetic results after conservation therapy for breast cancer. Int J Radiat Oncol Biol Phys 1995;31:753-64. [Crossref] [PubMed]



