Skin metastasis on the neck: an unusual presentation of recurrence of papillary thyroid carcinoma
Introduction
Differentiated thyroid carcinomas such as papillary and follicular carcinomas metastasize usually to the lymph nodes, lungs and bone. Skin metastasis of papillary thyroid carcinoma (PTC) is rare and hints a locally invasive tumor (1). It represents 0.7–2.0% of all cutaneous malignant neoplasms. Skin metastasis usually occurs as a first sign of an occult thyroid carcinoma (2).
Here, two cases of skin metastases of papillary thyroid cancer are presented. Both of the patients were female, one is 83 and the other is 65 years old.
Case presentation
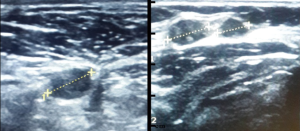
The patients were admitted to the hospital with a movable skin lesion on anterior neck region. Both patients had no family history of thyroid disease or exposure to radiation. In both patients, a palpable, mobile, firm mass without evidence of thyrotoxicosis in addition to TSH suppression was found in anterior neck region in physical examination (Figure 1).
Patient one is an 83-year-old female who underwent total thyroidectomy for papillary thyroid cancer followed by 131I ablation therapy and thyroid suppression therapy with levothyroxine in order. One year after thyroidectomy, in the thyroid scintigraphy, no activity was seen in thyroid region. Disease free survival (DFS) was three years until the occurrence of skin metastasis in the thyroidectomy scar. By palpation, a 10 mm firm mobile mass was palpated in right upper neck region. Thyroid ultrasonography revealed two hypoechoic lesions, one was 11.4 mm and the other one was 11 mm in diameter, on left paramedian region superficially on the upper right neck. Central vascularization was observed and both lesions were considered as lymphadenopathy. Fine needle aspiration biopsy (FNAB) was obtained from level 3 neck region and no metastasis was seen. Excisional biopsy for palpable masses was performed due to discordance with physical examination and imaging modalities (Figures 2,3).

Patient two is a 65-year-old female who had a total thyroidectomy 5 years ago for papillary carcinoma then functional neck dissection due to metastasis 3 years after that and then received 131I ablation therapy. In the report of positron emission tomography (PET) which was performed to scan distant metastasis, no metastasis nor recurrence was found. Lymph node dissection was performed to ascertain the diagnosis. In the thyroid ultrasonography of this patient, a 4 mm × 3.5 mm and another 3.5 mm × 3 mm sized two round, hypoechoic lymph nodes with central vascularization were seen on the left side of her neck. FNAB of these subcutaneous nodules was carcinoma cells consisting of partial follicular cells and then excisional biopsy was performed for definite diagnosis of recurrence.
For both patients, the histological examination of the excisional biopsy specimens on the neck region showed cystic lesions filled with papillary structures, which are evidence of PTC with solid trabecular pattern. Tissue immunohistochemistry was positive for thyroglobulin, PAX-8 antibody and TTF-1 in both patients. Both of the patients had heavily stained for thyroglobulin due to the recurrence of the disease indicating tumor burden.
Discussion
PTC tends to metastasize to regional lymph nodes but distant metastasis is rare (2). In these two patients, distant metastasis to the skin is occurred in the neck. In the literature, the most common site of skin metastasis is the scalp and usually skin metastasis is encountered in previous PTC cases (3). There is no gender predominance in skin metastasis of papillary thyroid cancer. So it is only coincidence that both of our patients were females (4).
When distant metastasis develops, prognosis of the disease is poor (5). Therefore, skin metastasis of papillary thyroid cancer is a poor prognostic factor. In both cases, there was no evidence of persisting tumor in the neck. This shows that a case of recurrent PTC may represent with a distant metastasis. If the patient does not have a previous thyroid malignancy history, diagnosis of PTC metastatic to the skin may be difficult since primary skin tumors such as apocrine tumors have similar histopathological features (6). Nevertheless, in the presented two cases since there was a history of PTC, the diagnosis was easier with the help of histopathological examination. However, FNAB was inconclusive for the diagnosis of carcinoma and excisional biopsy was performed.
Since skin lesions of these two patients were not the first manifestation of cancer, the diagnosis of recurrence of cancer through these lesions represent systemic spread of known papillary thyroid cancer. Although clinically recurrence is not suspected in patients with the history of thyroid cancer, in conditions of admission with atypical skin lesions, biopsy should be taken for the differential diagnosis.
In literature, skin metastasis is also seen after FNAB of thyroid with PTC (7). However, possible mechanisms cannot be explained in previous literature reviews regarding skin metastasis of thyroid cancer after surgery, we can propose that during surgery, thyroid nodules can erupt and contamination with skin may cause metastasis (3,8). In here, these patients were operated previously in different centers, contamination with skin may be the cause of skin metastasis.
Skin metastases of thyroid cancer is localized to the upper body as scalp and face due to these locations’ rich dermal capillary network and therefore providing an ideal metastatic focus. However, the exact mechanism of skin metastasis is not fully known yet (9).
Conclusions
Skin metastasis of PTC should be kept in mind when differential diagnosis of atypical skin lesions are made, especially in the patients with thyroid malignancy history. Excisional biopsy is advised for definite diagnosis rather than FNAB due to inconclusive results and possible discordance with physical examination.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Alwaheeb S, Ghazarian D, Boerner SL, et al. Cutaneous manifestations of thyroid cancer: a report of four cases and review of the literature. J Clin Pathol 2004;57:435-8. [Crossref] [PubMed]
- de Giorgi V, Alfaioli B, Massi D, et al. Solitary cutaneous metastasis as the first sign of relapse of thyroid carcinoma: a clinical, dermoscopic-pathologic case study. Dermatol Surg 2009;35:523-6. [Crossref] [PubMed]
- Dahl PR, Brodland DG, Goellner JR, et al. Thyroid carcinoma metastatic to the skin: a cutaneous manifestation of a widely disseminated malignancy. J Am Acad Dermatol 1997;36:531-7. [Crossref] [PubMed]
- Koller EA, Tourtelot JB, Pak HS, et al. Papillary and follicular thyroid carcinoma metastatic to the skin: a case report and review of the literature. Thyroid 1998;8:1045-50. [Crossref] [PubMed]
- Horiguchi Y, Takahashi C, Imamura S. Cutaneous metastasis from papillary carcinoma of the thyroid gland. Report of two cases. J Am Acad Dermatol 1984;10:988-92. [Crossref] [PubMed]
- Romanelli P, Mejias A, Isaac G, et al. Cutaneous metastasıs from papıllary thyroıd carcınoma. Am J Dermatopathol 1994;16:102. [Crossref]
- Karwowski JK, Nowels KW, McDougall R, et al. Needle Track Seeding of Papillary Thyroid Carcinoma from Fine Needle Aspiration Biopsy. Acta Cytol 2002;46:591-5. [Crossref] [PubMed]
- Farina E, Monari F, Tallini G, et al. Unusual Thyroid Carcinoma Metastases: a Case Series and Literature Review. Endocr Pathol 2016;27:55-64. [Crossref] [PubMed]
- Avram AM, Gielczyk R, Su L, et al. Choroidal and skin metastases from papillary thyroid cancer: case and a review of the literature. J Clin Endocrinol Metab 2004;89:5303-7. [Crossref] [PubMed]