Robotic modified radical neck dissection with bilateral axillo-breast approach
Introduction
Robotic thyroidectomy with bilateral axillo-breast approach (BABA) was introduced in 2008, and has become popular worldwide (1). Many evidences support the safety and feasibility of BABA robotic thyroidectomy. Recently, there is a report that it was safe to perform the robotic surgery up to 2 cm of the tumor (2). As the skills have been upgraded, surgeons adapt the procedure to more advanced cases. Especially in case of lateral neck metastasis, 8 to 15 cm long incision is needed, and young women can be reluctant to have such a long incision in the neck (3). It is a great help to have an ‘oncoplastic thyroid surgery’ for those patients. BABA robotic thyroidectomy makes four tiny incisions (8 mm) at areolae and skin creases of the axillae and can perform modified radical neck dissection (MRND) effectively.
Surgical indications and contraindications
The eligible criteria for BABA robotic MRND is a patient of well-differentiated thyroid carcinoma (mostly papillary thyroid cancer) with suspicious or pathologically confirmed lateral neck metastasis. The contraindications of BABA robotic MRND are far advanced cases as follows: (I) advanced medullary thyroid carcinoma or poorly differentiated carcinoma; (II) the metastatic lymph nodes encase the common carotid artery or internal jugular vein; (III) the suspicious lymph nodes are located beneath the clavicle (3-5).
Surgical instruments
- Vascular tunneler (Gore-Tex, Flagstaff, AZ, USA).
- Harmonic (Ethicon Endo-Surgery, Cincinnati, OH, USA).
- Plastic endobag (EndoCatch, Auto Suture, United States Surgical, Norwalk, CT, USA).
- da Vinci robotic instruments: Maryland grasp and Prograsp (Intuitive Surgical Inc., Sunnyvale, CA, USA).
- Ten mL syringes with 22-gauge spinal needle: 200 mL normal saline with 1 mL epinephrine (1:200,000).
- Surgical pillow.
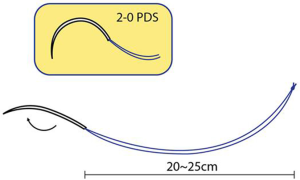
- The 20–25 cm of 2-0 polydioxanone (PDS; Ethicon, San Angelo, TX, USA): to retract the SCM muscle laterally from outside (Figure 1).
Surgical procedures
Position
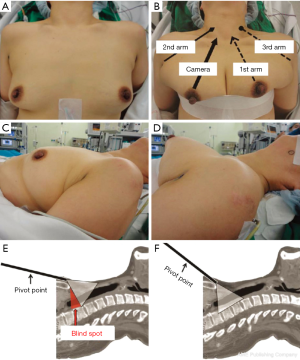
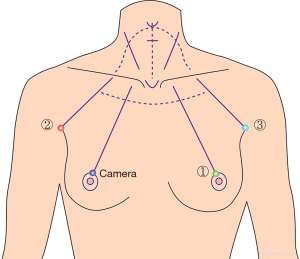
The patient is placed in the supine position on an operating table with a surgical pillow under the shoulders. The patient’s neck is gently extended to expose the neck. Arms should be fixed in the abducted position in order to expose the axillae. To facilitate dissection of lower neck and to get rid of blind spot, the elevation of the circumareolar site with an elastic band is helpful (Figure 2). For MRND, it is also helpful to reposition the direction of the camera port so that it corresponded with medial border of the SCM muscle. A slight clockwise rotation of the camera port is needed for left MRND. The location of the camera port for the right MRND is different from that for the left. After releasing the docking, the camera port is moved to the left areolar incision, and the third arm is moved to the right side of the second arm.
Flap design & dissection
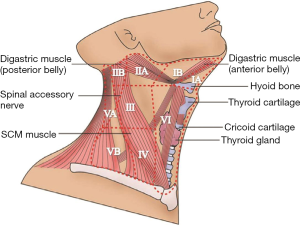
Draw guidelines along the landmarks of the chest and the neck, i.e., midline, thyroid cartilage (V), cricoid cartilage (+), anterior border of the sternocleidomastoid (SCM) muscle, the clavicles, suprasternal notch (U), circumareolar & axillary incisions and trajectory lines from the incision to cricoid cartilage as described in the previous chapter (Figure 3). Epinephrine-saline mixture is then injected into the working space (6). This “hydrodissection” technique makes a saline pocket in the subplatysmal layer, which decreases the bleeding in the flap area and makes the subsequent dissection easier. The working space for BABA robotic MRND should be made wider than the flap for usual robotic thyroidectomy. It should be extended over the lateral border of the ipsilateral SCM muscle laterally and to the lower border of the submandibular gland and posterior belly of digastric muscle superiorly. During flap dissection to the lateral side, the great auricular nerve is encountered. Identifying this nerve is very important, because it is helpful to predict the location of the spinal accessory nerve at Erb’s point and injury of the great auricular nerve would make loss of sensation around earlobe area, which can lower the quality of life seriously.
Surgical landmarks of robotic MRND
The anatomic landmarks used to dissect the lateral lymph node compartments are depicted in Figure 4.
Level IV and Vb dissection
Important structures of level IV and Vb:
- Internal jugular vein.
- Vagus nerve.
- Phrenic nerve.
- Cervical plexus (Erb’s point).
- Brachial plexus.
- Thoracic duct (left side).
- Transverse cervical artery.
The dissection begins with division between SCM muscles and strap muscles. Usually the Maryland forceps are docked in the ipsilateral axillary port, and the Prograsp forceps are docked in the contralateral axillary port. The entire medial border of the SCM muscle is dissected with lateral traction of the Maryland forceps. The omohyoid muscle is identified, and its inferior belly is cut with a Harmonic, thereby exposing the internal jugular vein. The omohyoid muscle is a good landmark for the internal jugular vein and can be cut without any functional loss or deformity. After the medial border of SCM is fully exposed, the muscle is pulled laterally using anchoring suture by 2-0 PDS. For the anchoring suture, a PDS with an unfolded needle is inserted into the operation field through an axillary trocar. The PDS suture is made around the SCM muscle, then extracted through the skin, thereby pulling the SCM laterally. For better visualization the lowermost subclavicular area, the pivot point of camera port is set as possible as high (Figure 2).
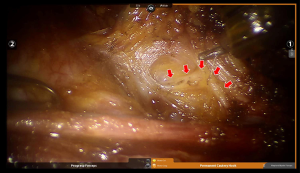
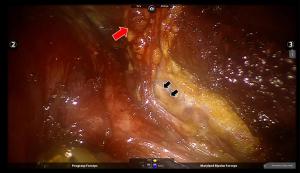
The internal jugular vein is drawn medially using the Prograsp forceps. The soft tissue with lymph nodes is detached from the anterior surface of the internal jugular vein to the posterior aspect of the internal jugular vein until the common carotid artery and vagus nerve are identified. Inferior dissection of level IV is performed preserving the transverse cervical artery and the phrenic nerve (Figure 5). Especially in the left level IV dissection, branches of the thoracic duct are identified and clipped. Thanks to the 15 times magnified view of the da Vinci system, main trunk of the thoracic duct can be identified easily. The best way to prevent postoperative chyle leakage would be to identify and preserve it (Figure 6). Small branches of lymphatic ducts can be managed using a robotic Hem-o-Lock clips (Weck Surgical Instrument; Teleflex Medical, Durham, NC, USA) or a Harmonic. Careful dissection of level IV is required to preserve the phrenic nerve. Not to injure the phrenic nerve which is always deep to the transverse cervical artery, surgeons should not enter the deep space beneath the transverse cervical artery unnecessarily.
Level Vb LNs can be dissected with medial traction of LNs using Prograsp forceps, while preserving the brachial plexus and the spinal accessory nerve.
Level III dissection
Important structures in level III compartment:
- Internal jugular vein.
- Vagus nerve.
- Phrenic nerve.
- Cervical plexus.
The dissection is extended to the level III after dissecting level IV and Vb. The vagus nerve and the phrenic nerve that are identified at the level IV dissection are traced carefully not to give any injury. Care should be taken to preserve cervical plexus as far as possible. Magnified vision of da Vinci system can facilitate the preservation these nerves. Dissection of the level III compartment is performed carefully not to perforate the internal jugular vein. If the internal jugular vein is perforated, it can be controlled by metal endoclips. In case of uncontrollable tear of internal jugular vein, it should be ligated with a robotic Hem-o-Lock clips.
Level IIa dissection
Important structures of level IIa:
- Internal jugular vein.
- Spinal accessory nerve.
- Hypoglossal nerve.
- Submandibular gland.
- Marginal mandibular branch of facial nerve.
After finishing the dissection of level IV, Vb and level III compartments, the camera trocar and contralateral circumareolar trocar are placed slightly forward to provide a better view for level IIa dissection. The dissection is preceded until the posterior belly of the digastric muscle is exposed superiorly. The spinal accessory nerve should be preserved at this point. The spinal accessary nerve runs under the internal jugular vein mostly, but it can be found over the internal jugular vein. The spinal accessary nerve can be confirmed with the current of 1.0–2.0 mA of neuromonitor (Medtronics, Jacksonville, FL, USA).
The hypoglossal nerve and the marginal mandibular branch of facial nerve also should be preserved during the level IIa dissection but they are not necessarily exposed unless rigorous dissection is needed for nearby clinically metastatic lymph nodes.
Closure
The resected specimen is removed using an endobag (EndoCatch, Auto Suture, United States Surgical, Norwalk, CT, USA). Meticulous hemostasis is needed and a Jackson-Pratt drain is inserted through the contralateral axillary incision. Suture between the SCM and strap muscles is not needed in most cases. Omohyoid muscle can be reconstructed with an absorbable suture. The skin incision is closed with 5-0 absorbable suture by a knot-burying technique. The wounds are covered by sterile dressings after the suture.
Postoperative management
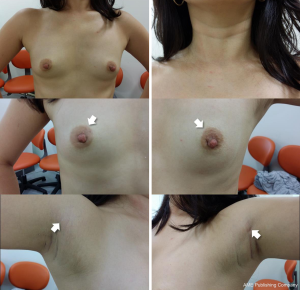
Patient who underwent robotic BABA MRND starts food intake in 2 hours after the surgery. The amount of drainage fluid is regularly checked during the patient’s hospital stay, and the drain is removed when the patient is discharged, usually on postoperative day 3 (7). In patient with left neck dissection with suspected thoracic duct injury, low fat diet is recommended not to cause the chyle leakage. Wounds are checked in 2 weeks after discharge (Figure 7). All patients are recommended to undergo radioactive iodine (RAI) ablation to lower the rate of the recurrence. RAI dose is determined according to the tumor progression at the final pathologic report. Tumor recurrence is regularly monitored by ultrasonography and measuring Tg concentration at the outpatient clinic.
Surgical outcomes of robotic MRND with BABA
After total thyroidectomy with MRND, the notification of surgical complications, such as transient hypocalcemia, permanent hypocalcemia, transient vocal cord palsy, permanent vocal cord palsy, chyle leakage, postoperative bleeding, and wound infection, is important.
Tables 1 and 2 show surgical outcomes after robotic BABA MRND in two institutions. There were no open conversion from the robotic procedure in two institutions. The rates of transient and permanent hypocalcemia were 46.7% (7/15) and 0% (0/15) in Seoul National University Hospital (SNUH), respectively, and 0% (0/13) and 0% (0/13) in Chung-Ang University Hospital (CAUH), respectively. The rates of transient and permanent vocal cord palsy were 6.7% (1/15) and 0% (0/15) in SNUH, respectively, and 0% (0/13) and 0% (0/13) in CAUH, respectively. There was no report of postoperative bleeding and wound infection in both institutions. Chyle leakage was observed in one case (7.7%, 1/13) in CAUH, on the other hand, no case in SNUH. A patient who was undergone robotic left MRND and shown small amount of chyle leakage recovered in 2 days after fat-free diet. One patient experienced Horner’s syndrome, with symptoms spontaneously regressing after 6 months in SNUH (6.7%, 1/15), on the other hand, no case presented in CAUH.

Full table

Full table
The median sTg concentrations after the first RAI treatment were 0.8 ng/mL (range, 0.1–36.5 ng/mL) in SNUH and 2.57 ng/mL (range, 0.15–16.19 ng/mL) in CAUH, respectively. Eight (53.3%) and 14 (93.3%) patients in SNUH had sTg concentrations below 1 ng/mL and below 2 ng/mL, respectively. Nine (69.2%, 9/13) of CAUH patients showed sTg concentration below 1 ng/mL. After a mean follow-up of 18.7 months in SNUH and 15.9 months in CAUH, no recurrence had been occurred after the robotic MRND. The postoperative satisfaction of the patients was high in both institutions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Lee KE. Outcomes of 109 patients with papillary thyroid carcinoma who underwent robotic total thyroidectomy with central node dissection via the bilateral axillo-breast approach. Surgery 2010;148:1207-13. [Crossref] [PubMed]
- Chai YJ, Suh H, Woo JW, et al. Surgical safety and oncological completeness of robotic thyroidectomy for thyroid carcinoma larger than 2 cm. Surg Endosc 2017;31:1235-40. [Crossref] [PubMed]
- Seup Kim B, Kang KH, Park SJ. Robotic modified radical neck dissection by bilateral axillary breast approach for papillary thyroid carcinoma with lateral neck metastasis. Head Neck 2015;37:37-45. [Crossref] [PubMed]
- Lee KE, Kim E. Robotic thyroidectomy by bilateral axillo-breast approach: review of 1,026 cases and surgical completeness. Surg Endosc 2013;27:2955-62. [Crossref] [PubMed]
- Lee KE, Choi JY, Youn YK. Bilateral axillo-breast approach robotic thyroidectomy. Surg Laparosc Endosc Percutan Tech 2011;21:230-6. [Crossref] [PubMed]
- Choi JY, Lee KE, Chung KW, et al. Endoscopic thyroidectomy via bilateral axillo-breast approach (BABA): review of 512 cases in a single institute. Surg Endosc 2012;26:948-55. [Crossref] [PubMed]
- Lee KE. Surgical completeness of bilateral axillo-breast approach robotic thyroidectomy: comparison with conventional open thyroidectomy after propensity score matching. Surgery 2011;150:1266-74. [Crossref] [PubMed]