Silk suture reaction in thyroid surgery
Introduction
Thyroidectomy is one of the most commonly performed surgical procedure worldwide. Many complications as hypocalcemia, recurrent laryngeal nerve paralysis, hemorrhage and infection are encountered after thyroidectomy. A silk suture reaction, a benign granulomatous inflammatory foreign body reaction is a rare complication of thyroid surgery. However, since it can be mistaken for a thyroid malignancy, it is important to diagnose and treat this rare post-thyroidectomy complication. In this case report we aimed to show how to diagnose a silk suture reaction clinically and how to treat this lesion.
Case presentation
One of our patients is a 48 years old female, admitted with a neck swelling (Figure 1). Her thyroid function tests are normal. She had a right partial and left near total thyroidectomy six years ago. In the neck ultrasonography, there was a 25 mm × 26 mm, heterogeneous nodule with a hypoechoic rim on the superior of the right thyroid lobe. In the scintigraphy, that nodule was normoactive while another nodule in the lower pole was hyperactive. Fine needle aspiration biopsy showed that both nodules consists of benign follicular epithelial cells.
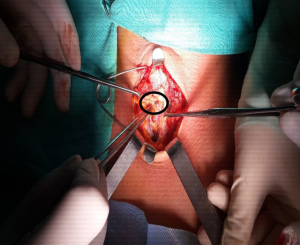
The other patient, a 34 years old female, applied to the hospital with a leakage from the incision of previous thyroidectomy. Six years ago she had a bilateral total thyroidectomy. She had a normal free T4, free T3, and TSH values. In her thyroid ultrasonography, two nodules with hypoechoic collection containing hyperechoic structure were seen. In thyroid scintigraphy, no radiopharmaceutical involvement in thyroid region was seen (Figure 2). Fine needle aspiration biopsy (FNAB) showed neutrophils, histiocytes and granulation tissue. There was no evidence of microorganisms or malignancy. The residue suture material and fibrotic tissue were excised (Figure 3).
Discussion
A silk suture reaction is a benign, granulomatous inflammatory reaction occurring due to the use of non-absorbable suture in thyroidectomies. An inflammatory lesion can be differentiated from a malignancy or an infection with a fine needle aspiration biopsy. Since recurrence of thyroid malignancy is highly suspected, surgical excision of the lesion should be performed. Surgical pathology of these two patients showed benign epithelial cells and chronic granulomatous inflammation.
In the silk reaction, the suture is compact and it is surrounded by a fibrous tissue capsule. Inside the capsule also histiocytes, lymphocytes and giant cells are seen. In another type of silk reaction, suture is again covered by a capsule but this time, the suture is invaded by fibroblasts and histiocytes. It is much like a granuloma (1). However, in the first patient, FNAB showed benign follicular lesions which could be due to remaining thyroid tissue from the previous surgery of that patient.
Silk reaction is not symptomatic and usually does not interfere with wound healing. If an amplified response occurs, it is seen either as an inflammation along the incision or as a leakage in the suture line as seen in the second patient. Leakage or a fistulous fluid in the suture line leads to the diagnosis of a foreign body reaction. In last decade, rather than silk, absorbable synthetic sutures are used. With these absorbable polymers, less foreign body reaction is encountered. Furthermore, use of ligation is discontinued with facilitation of energy based devices and sutureless thyroidectomy is preferred choice for thyroidectomy (2-4). When a patient is presented with a wound infection or leakage, suture reaction should be kept in mind. These two patients, who developed silk suture reaction had delayed reaction to silk since there was 6 years between the implantation of silk suture and the reaction (5).
In the ultrasound of both patients, heterogeneous nodule with a hypoechoic rim was seen. In a study done by Kim et al. (6), it was seen that internal echogenic foci were higher in suture reaction than recurrent carcinomas. To differentiate suture granulomas from locally recurrent tumors, the shape, heterogeneity and presence of central echogenic foci are important (6).
Conclusions
A suture reaction after thyroid surgery can be diagnosed cytologically with fine needle aspiration biopsy. Successful treatment of this chronic inflammation is achieved with surgically removal of silk suture.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Nordman CH, Hernberg S. Blood lead levels and erythrocyte delta-amino-levulinic acid dehydratase activity of selected population groups in Helsinki. Scand J Work Environ Health 1975;1:219-32. [Crossref] [PubMed]
- Teksoz S, Bukey Y, Ozcan M, et al. Sutureless thyroidectomy with energy-based devices: Cerrahpasa experience. Updates Surg 2013;65:301-7. [Crossref] [PubMed]
- Arikan AE, Teksoz S, Bukey Y, et al. Short-stay Sutureless Thyroidectomy is Safe and Effective: Cerrahpasa Experience. Surg Technol Int 2014;25:907-101. [PubMed]
- Dionigi G, Wu CW, Kim HY, et al. Safety of energy based devices for hemostasis in thyroid surgery. Gland Surg 2016;5:490-4. [Crossref] [PubMed]
- Rossitch E Jr, Bullard DE, Oakes WJ. Delayed foreign-body reaction to silk sutures in pediatric neurosurgical patients. Childs Nerv Syst 1987;3:375-8. [Crossref] [PubMed]
- Kim JH, Lee JH, Shong YK, et al. Ultrasound features of suture granulomas in the thyroid bed after thyroidectomy for papillary thyroid carcinoma with an emphasis on their differentiation from locally recurrent thyroid carcinomas. Ultrasound Med Biol 2009;35:1452-7. [Crossref] [PubMed]