Transoral endoscopic thyroidectomy using vestibular approach: updates and evidences
Introduction
Since the nineteenth century, the standard open cervical thyroidectomy technique has been significantly improved in order to reduce morbidity and mortality rates. In the present day, the surgical technique now focuses on minimizing visible scarring by moving the incision to a hidden area (1,2). Various remote access thyroidectomy techniques for endoscopic and robotic thyroidectomy have been invented and developed for over two decades because of their enhanced cosmetic results compared to open surgery (3-6). However, with those techniques, the scars are still seen at the incision area. Recently, natural orifice transluminal endoscopic surgery (NOTES) of the thyroid has been developed (7,8). A benefit of this innovative thyroid technique is its excellent cosmetic outcome due to scarless surgery. Despite its benefits, however, this procedure has been considered experimental due to the limitations of the previous sublingual approach (9-12). The oral vestibular approach has since been introduced with better clinical outcomes (13-15). We have reviewed the history and development, clinical evidence, and potential future development of transoral thyroidectomy techniques.
Development of minimally invasive thyroidectomy
Minimally invasive surgery has been adopted for thyroid surgery since Ganger in 1996 (16). For over two decades, various approaches for endoscopic thyroidectomies have been proposed, with some becoming popular to date. The rationale for these procedures was to reduce, prevent, or eliminate scarring on the neck by moving to other areas with less pain, less bleeding and a faster recovery period (3-6). The concepts of good minimally-invasive thyroidectomy technique should include: (I) a short distance from incisions to the thyroid, so the risk of instrumental collision is reduced and the distance of flap dissection is shortened for less trauma from access; (II) excellent cosmetic outcome, with incisions ideally hidden on an unnoticeable area of the body; (III) a good operative and anatomic view for patient safety, so no important structures are proximal to the operative area, such as the carotid artery, internal jugular vein, or brachial plexus; (IV) oncological outcome such that the specimen is taken out with good shape; (V) acceptable price, using only conventional instruments with acceptable operative costs, and (VI) simplification, so the technique is simple, with a short learning curve, and can be performed by every surgeon.
However, some remote access thyroidectomy techniques, for example, the BABA technique or axilla technique, cannot be considered minimally invasive because they usually require large areas of flap dissection from the axilla or breast to the thyroid gland (4,5,17,18). Later, the patients may have paresthesia over the skin for a long time after surgery, which might impact their quality of life. Moreover, there are often surgical difficulties as a result of the very long distance from the incision to the thyroid, which can create instrumental collision.
To resolve the problem and achieve the goal of good, minimally invasive thyroidectomy mentioned earlier, transoral access seems to be an appropriate route for thyroidectomy because: (I) the distance between mouth and thyroid is the shortest among the various endoscopic/robotic approaches, resulting in reduction of instrumental collision and difficulties of surgery; (II) the best cosmetic outcomes are achieved as the wound will be hidden intraorally; (III) the operative visualization is a top-down view, cranial to caudal. Surgeons could easily get used to the view and the anatomy is very clear, similar to open surgery but upside down; (IV) no complicated instruments are necessary and the technique is feasible to be performed with a short learning curve, and (V) this is another midline approach meaning that a total thyroidectomy or central lymph node dissection can be performed without any additional incision or port.
Classification of transoral endoscopic thyroidectomy
Sublingual approach
The concept of thyroid NOTES has been developed by Witzel et al. (7). In their report, the transoral endoscopic thyroidectomy was performed in 2 fresh cadavers and 10 living pigs using a single 10 mm incision in the center of the sublingual area. Additionally, two 3.5 mm incisions for two 3.5 mm trocars were made externally at the neck to allow the triangulation of rigid instruments during surgery. An oscilloscope and ultrasonic shears were used for the entire operation. In their report, no complications or bleeding in the living pigs were found. Karakas et al. (19) introduced another refined technique for the parathyroid called transoral partial parathyroidectomy (TOPP). The technique involved introducing a cervicoscope more dorsally compared to Witzel’s technique, and directly in front of the trachea. Experimentation was performed on 10 living pigs, 10 human cadavers, and finally in 2 patients with primary hyperparathyroidism. Unfortunately, 1 patient experienced a transient palsy of the right hypoglossal nerve. Karakas et al. continued their evaluation of this technique and reported in another paper in 2014 (20), for which 85 parathyroid adenoma patients were offered TOPP as a surgical option, but only 5 patients accepted the procedure. Of these patients, 2 required conversion to open surgery. One patient experienced transient recurrent laryngeal nerve (RLN) palsy. One patient experienced transient right hypoglossal nerve injury. They concluded that, although feasible, TOPP was not readily accepted by patients and its complication rate was high. Since that time, TOPP has become impracticable with currently available devices (Table 1).
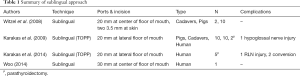
Full table
Combined sublingual and oral vestibular approach
The combination technique was first introduced by Benhidjeb et al. (8) and was called transoral video-assisted thyroidectomy (TOVAT). The researchers conducted experiments on 5 human cadavers. One 5 mm and two 3 mm trocars were introduced through the floor of the mouth and the oral vestibule. CO2 was insufflated at a pressure of 4–6 mmHg. After surgery, the cadavers were totally dissected to study the safety and anatomy of the procedure.
Another technique was performed in 8 real patients by Wilhelm et al. Actually, this procedure was similar to TOVAT but the name was changed to endoscopic minimally invasive thyroidectomy (eMIT) (9,10). The center port was refined to 10 mm and another 5 mm port was used at the oral vestibule. In 3 cases, conversion to open surgery was necessary due to specimen size. RLN palsy was found in 2 patients, one transient and one permanent. Mental nerve injury was found in 3 cases. Wilhem et al. later reported a bi-center series of eMIT, collaborating between German and Chinese institutes, reporting their 96 cases of eMIT. However, 1 case was found to have transient RLN injury, 1 case had permanent RLN injury. Mental nerve injury was found in 15 cases. There was infection at the sublingual incision and neck area in 6 cases. Conversion to open surgery was needed in 3 cases (12).
The sublingual route, including combination, has been critiqued and has experienced decreasing popularity due to the difficulty of the technique and its high complication rate (21-25). Although there are some papers still investigating this technique, it is no longer active in real clinical practice (26,27) (Table 2).
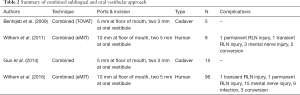
Full table
Oral vestibular approach
The oral vestibular approach was first described by Richmon et al. They first performed transoral robotic-assisted thyroidectomy (TRAT) with a sublingual approach and found later that moving the camera to the oral vestibule was better (28). Nakajo et al. performed transoral video-assisted neck surgery (TOVANS) in 8 cases (13). A single 2.5 cm incision was created at the center of the oral vestibule. The operation was carried out using a gasless technique and K-wire for hanging up the skin. Only 1 case experienced RLN injury. All 8 cases were found to have paresthesia around the chin, persistent for more than 6 months. These refer to the mental nerve injury as well. Wang et al. reported another vestibular technique in 12 patients using 3 vestibular ports and CO2 insufflation (14). The complication was 2 cases of skin ecchymosis. From those earlier reports, mental nerve injury was the most concerning problem.
The transoral endoscopic thyroidectomy vestibular approach (TOETVA) was performed in 60 patients by Anuwong (15). All three ports were placed at the oral vestibule. No mental nerve injury was found and only 2 patients experienced transient RLN palsy, which completely resolved afterwards. To date, 500 cases of TOETVA have been performed at the Police General Hospital, Thailand. The technique will be described in brief in the technique section. Udelsman et al. at reported a series of 7 cases of TOETVA (2 parathyroidectomy and 5 thyroidectomy) with no complications, which was the first series in the United States (29). Jitpratoom et al. reported a comparison study between 46 TOETVA and 49 open thyroidectomies for Grave’s disease in terms of safety (30). The operative time was longer in the TOETVA group. In contrast, pain was lower in the TOETVA group than in open surgery. The remaining parameters showed no significant differences in terms of safety (Table 3).

Full table
Trans-tracheal approach
This technique was reported by Liu et al. in 2015 (31). Total transtracheal endoscopic thyroidectomy was performed in 3 pigs and 14 beagle dogs using a 4.2 mm flexible fiber optic bronchoscope. Endoscopic biopsy forceps and laparoscopic curved instruments were used during the procedure. The scope and instruments were inserted beside the orotracheal tube and then a small incision was made at the anterior tracheal wall to reach the thyroid gland. A total of 26 thyroidectomies and 8 partial thyroidectomies were performed. The anterior tracheal wall was closed using endostitch. The result showed no morbidity or mortality in 5 days. After that, all the animals were sacrificed. However, this is an experimental procedure carried out only on animals. No human clinical application was performed.
From the classifications above, the sublingual approach was no longer active and the trans-tracheal approach was only an animal experiment. The only thyroid NOTES technique that is currently working is the oral vestibular operation. The number of TOETVA publications has increased recently (32-37).
Surgical technique of TOETVA
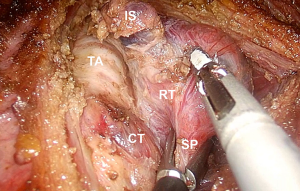
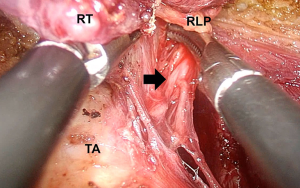
The technique is based on Anuwong’s technique (15,38). In brief, the patient is placed in a supine position under nasotracheal intubation. Oral tracheal intubation can be used but will somewhat limit the movement of instruments during operation. The neck is placed in a slightly extended position with a sandbag under the shoulders. Pre-operative amoxicillin-clavulanic acid is administered 30 min before incision. Three incisions are made at the oral vestibular area, which is the area between the lower lip and lower teeth, for the laparoscopic trocar insertions. A 10–15 mm trocar is inserted at the center, while another two 5 mm trocars are inserted laterally. The position of the lateral ports has since been refined to a more anterior area, just under the inferior lip to the greatest extent possible. This is done to avoid injury to the branches of mental nerves located just below this area. The working space is then dissected using the dilator first, followed by dissection under direct vision. The plane was in between the strap muscle and platysma muscle. The strap muscle midline raphe is opened up to expose the thyroid and trachea. Lateral dissection of the thyroid is performed and then external suturing by 2/0 silk is introduced from the neck skin outside to retract the strap muscle laterally. Subsequently, thyroid lobectomy was initiated by cutting the isthmus. Next, the superior pole of the thyroid was accessed at the avascular plane between the cricoid and the superior pole of the thyroid, which is called Joll’s space, and which is exposed. Mobilization of the superior pole is performed by inserting the grasper into this space and pulling the superior pole upward (Figure 1). Superior thyroid vessels are then ligated using an ultrasonic scalpel. After that, the thyroid is mobilized to the opposite side as much as possible, which is called the ‘median rotation maneuver’. The upper parathyroid will be revealed after medial rotation. The RLN is then identified at the insertion, traced down to the inferior parallel to the trachea in the trachea-esophageal groove (Figure 2). The lower parathyroid is also preserved. After identification of all important anatomy, a lobectomy is completed using a harmonic scalpel. An endobag is introduced and inserted via a 10 mm port. The specimen is dunked inside this endobag and extracted from the 10–15 mm incision. If the specimen is too large, cutting of the specimen must be done while inside the endobag and under the scope. If a total thyroidectomy is necessary, a contra lateral thyroidectomy can be done with the same technique. Oral vestibule wounds were sutured using 4/0 absorbable sutures. A pressure dressing was placed around the chin for 24 hours. Liquid diet was offered right after surgery and soft diet from the next morning. The patient can be kept in the hospital overnight and discharged the next day. However, in Asian cultures, it is normal for the patient to stay in the hospital as long as possible. In our experience, 3-4 days of post-operation hospital stay is common in Asian countries.
Discussion
It is very important for innovative operations to prove themselves in terms of the benefit to the patient. To ensure patients’ safety, clinical evidence is the most important matter of concern before widespread use of that technique. For transoral endoscopic thyroidectomy, there were many studies in animals and cadavers before application to clinical practice (8-15). The transoral approach is to operate from the mouth which is contaminated with many bacteria, to the neck, which is the sterile area. If infection occurs, it can result in the development of abscesses and systemic infection, as well as airway compression. This problem is the main concern in performing transoral thyroidectomy (39). The clinical evidence was sufficient to demonstrate that a sublingual approach may not be appropriate due to many complications which occurred. In particular, some infections were observed in certain series (10,12). In the literature review, there was no infection in the oral vestibular approach. Thus, a pure oral vestibular approach, especially TOETVA, seems to be safer regarding infection.
RLN injury seems to be another problem even in endoscopic or open thyroidectomy. Despite the rate being very low in the present day due to a better operative technique (40,41), it is better to avoid this problem. Inabnet et al. (34), Dionigi et al. (36), and Wang et al. (33) demonstrated intraoperative neuromonitoring in TOETVA operations with good results. However, the numbers of patients in those papers were too small; larger studies should be conducted to confirm that neuromonitoring can reduce the rate of RLN injury.
In the case of total thyroidectomy, hypoparathyroidism is the next important problem. The use of indocyaninegreen (ICG) is being investigated in terms of its use for locating the parathyroid glands or proofing of the viable glands (42-44). This could be applied to TOETVA for reducing the rate of hypoparathyroidism. In our institute, we are currently investigating the ICG in TOETVA and will report our experience very soon.
One drawback of TOETVA is the removal of the specimen. There are concerns about how to remove such a big goiter through a 1 cm incision at the oral vestibule (39). For our specimen extraction technique, inserting the specimen into an endobag is mandatory whether the nodule is benign or malignant. The normal thyroid size not exceeding 3–4 cm can be extracted by using sponges, forceps, and a ‘push and pull technique’ without rupture of the thyroid capsule. Larger glands cannot be extracted without manipulation. In that situation, we have made two to three 1 cm incisions in the thyroid capsule inside the endobag under endoscopic view. Care must be taken to make incisions at the normal thyroid portion, away from the tumor. By this technique, the specimen can be squeezed through 1–1.5 cm incisions. This technique works well for benign tumors. However, there will be occult malignancy on any cancer nodule. In Grave’s disease, the possibility to be cancer is unlikely, so in this case TOETVA can be used safely. In the case of pre-operative diagnosis of thyroid carcinoma, TOETVA could be performed only for 1–2 cm cancer nodules because the central incision size is limited to 1–1.5 cm. We aware of the oncological result of the cancer nodule. Moreover, another benefit of TOETVA is the clear anatomical view. Central lymph node dissection can be done easily and completely. However, long term oncological outcome studies would be necessary to evaluate the benefits in thyroid cancer patients.
For these reasons, we strongly recommend using this TOETVA surgery for: (I) benign thyroid disease with small to moderate thyroid nodules; (II) thyroid cancer which has 1–2 cm cancer nodules, and (III) Grave’s disease limited to 10 cm in size.
Conclusions
TOETVA can be performed safely with excellent cosmetic results, providing good oncological outcomes. In our experience as well as in the literature review, TOETVA is one of the transoral endoscopic thyroidectomies which can be considered no longer an experimental operation. It can be performed in real clinical practice in selected patients with few complications, similar to standard open thyroidectomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Dordea M, Aspinall SR. Short and long-term cosmesis of cervical thyroidectomy scars. Ann R Coll Surg Engl 2016;98:11-7. [Crossref] [PubMed]
- Arora A, Swords C, Garas G, et al. The perception of scar cosmesis following thyroid and parathyroid surgery: A prospective cohort study. Int J Surg 2016;25:38-43. [Crossref] [PubMed]
- Miccoli P, Berti P, Conte M, et al. Minimally invasive surgery for thyroid small nodules: preliminary report. J Endocrinol Invest 1999;22:849-51. [Crossref] [PubMed]
- Ikeda Y, Takami H, Niimi M, et al. Endoscopic thyroidectomy by the axillary approach. Surg Endosc 2001;15:1362-4. [Crossref] [PubMed]
- Choe JH, Kim SW, Chung KW, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg 2007;31:601-6. [Crossref] [PubMed]
- Wang C, Feng Z, Li J, et al. Endoscopic thyroidectomy via areola approach: summary of 1,250 cases in a single institution. Surg Endosc 2015;29:192-201. [Crossref] [PubMed]
- Witzel K, von Rahden BH, Kaminski C, et al. Transoral access for endoscopic thyroid resection. Surg Endosc 2008;22:1871-5. [Crossref] [PubMed]
- Benhidjeb T, Wilhelm T, Harlaar J, et al. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc 2009;23:1119-20. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Video. Endoscopic minimally invasive thyroidectomy: first clinical experience. Surg Endosc 2010;24:1757-8. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg 2011;35:543-51. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral thyroid and parathyroid surgery--development of a new transoral technique. Surgery 2011;150:108-15. [Crossref] [PubMed]
- Wilhelm T, Wu G, Teymoortash A, et al. Transoral endoscopic thyroidectomy: current state of the art—a systematic literature review and results of a bi-center study. Transl Cancer Res 2016;5:S1521-S30. [Crossref]
- Nakajo A, Arima H, Hirata M, et al. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc 2013;27:1105-10. [Crossref] [PubMed]
- Wang C, Zhai H, Liu W, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery 2014;155:33-8. [Crossref] [PubMed]
- Anuwong A. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Series of the First 60 Human Cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 1996;83:875. [Crossref] [PubMed]
- Lee KE, Kim E. Robotic thyroidectomy by bilateral axillo-breast approach: review of 1,026 cases and surgical completeness. Surg Endosc 2013;27:2955-62. [Crossref] [PubMed]
- Kang SW, Lee SC, Lee SH, et al. Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery 2009;146:1048-55. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral thyroid and parathyroid surgery. Surg Endosc 2010;24:1261-7. [Crossref] [PubMed]
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral parathyroid surgery--a new alternative or nonsense? Langenbecks Arch Surg 2014;399:741-5. [Crossref] [PubMed]
- Dionigi G, Rovera F, Boni L. Commentary on transoral access for endoscopic thyroid resection: Witzel K, von Rahden BH, Kaminski C, et al. Transoral access for endoscopic thyroid resection. Surg Endosc 2008;22:1871-5. Surg Endosc 2009;23:454-5. [Crossref] [PubMed]
- Miccoli P, Materazzi G, Berti P. Natural orifice surgery on the thyroid gland using totally transoral video-assisted thyroidectomy: report of the first experimental results for a new surgical method: are we going in the right direction? Surg Endosc 2010;24:957-8; author reply 959-60. [Crossref] [PubMed]
- Benhidjeb T, Witzel K, Stark M, et al. Transoral thyroid and parathyroid surgery: still experimental! Surg Endosc 2011;25:2411-3. [Crossref] [PubMed]
- Benhidjeb T. Transoral Video-Assisted Thyroidectomy and Its Clinical Implementation. J Laparoendosc Adv Surg Tech A 2015;25:514-5. [Crossref] [PubMed]
- Benhidjeb T. Transoral Endoscopic Thyroidectomy with Central Neck Dissection. Chin Med J (Engl) 2015;128:1838. [Crossref] [PubMed]
- Guo P, Tang Z, Ding Z, et al. Transoral endoscopic thyroidectomy with central neck dissection: experimental studies on human cadavers. Chin Med J (Engl) 2014;127:1067-70. [PubMed]
- Woo SH. Endoscope-assisted transoral thyroidectomy using a frenotomy incision. J Laparoendosc Adv Surg Tech A 2014;24:345-9. [Crossref] [PubMed]
- Richmon JD, Pattani KM, Benhidjeb T, et al. Transoral robotic-assisted thyroidectomy: a preclinical feasibility study in 2 cadavers. Head Neck 2011;33:330-3. [PubMed]
- Udelsman R, Anuwong A, Oprea AD, et al. Trans-oral Vestibular Endocrine Surgery: A New Technique in the United States. Ann Surg 2016;264:e13-e16. [Crossref] [PubMed]
- Jitpratoom P, Ketwong K, Sasanakietkul T, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves' disease: a comparison of surgical results with open thyroidectomy. Gland Surg 2016;5:546-52. [Crossref] [PubMed]
- Liu E, Qadir Khan A, Niu J, et al. Natural Orifice Total Transtracheal Endoscopic Thyroidectomy Surgery: First Reported Experiment. J Laparoendosc Adv Surg Tech A 2015;25:586-91. [Crossref] [PubMed]
- Pai VM, Muthukumar P, Prathap A, et al. Transoral endoscopic thyroidectomy: A case report. Int J Surg Case Rep 2015;12:99-101. [Crossref] [PubMed]
- Wang Y, Yu X, Wang P, et al. Implementation of Intraoperative Neuromonitoring for Transoral Endoscopic Thyroid Surgery: A Preliminary Report. J Laparoendosc Adv Surg Tech A 2016;26:965-71. [Crossref] [PubMed]
- Inabnet WB 3rd, Suh H, Fernandez-Ranvier G. Transoral endoscopic thyroidectomy vestibular approach with intraoperative nerve monitoring. Surg Endosc 2017;31:3030. [Crossref] [PubMed]
- Park JO, Kim MR, Kim DH, et al. Transoral endoscopic thyroidectomy via the trivestibular route. Ann Surg Treat Res 2016;91:269-72. [Crossref] [PubMed]
- Dionigi G, Bacuzzi A, Lavazza M, et al. Transoral endoscopic thyroidectomy via vestibular approach: operative steps and video. Gland Surg 2016;5:625-7. [Crossref] [PubMed]
- Zeng YK, Li ZY, Xuan WL, et al. Trans-oral glasses-free three-dimensional endoscopic thyroidectomy-preliminary single center experiences. Gland Surg 2016;5:628-32. [Crossref] [PubMed]
- Anuwong A, Sasanakietkul T, Jitpratoom P. Transoral Endoscopic Thyroidectomy Vestibular Approach. November 2016, 3. doi: 10.1089/ve.2016.0076. [Crossref]
- Masha JL, Michael WY. Transoral Endoscopic Thyroidectomy Is a Novel Experimental Technique. Clinical Thyroidology 2017;29:19-21. [Crossref]
- Calò PG, Pisano G, Medas F, et al. Identification alone versus intraoperative neuromonitoring of the recurrent laryngeal nerve during thyroid surgery: experience of 2034 consecutive patients. J Otolaryngol Head Neck Surg 2014;43:16. [Crossref] [PubMed]
- Vasileiadis I, Karatzas T, Charitoudis G, et al. Association of Intraoperative Neuromonitoring With Reduced Recurrent Laryngeal Nerve Injury in Patients Undergoing Total Thyroidectomy. JAMA Otolaryngol Head Neck Surg 2016;142:994-1001. [Crossref] [PubMed]
- Lavazza M, Liu X, Wu C, et al. Indocyanine green-enhanced fluorescence for assessing parathyroid perfusion during thyroidectomy. Gland Surg 2016;5:512-21. [Crossref] [PubMed]
- Vidal Fortuny J, Belfontali V, Sadowski SM, et al. Parathyroid gland angiography with indocyanine green fluorescence to predict parathyroid function after thyroid surgery. Br J Surg 2016;103:537-43. [Crossref] [PubMed]
- Zaidi N, Bucak E, Yazici P, et al. The feasibility of indocyanine green fluorescence imaging for identifying and assessing the perfusion of parathyroid glands during total thyroidectomy. J Surg Oncol 2016;113:775-8. [Crossref] [PubMed]


