
Acute transient thyroid swelling following fine-needle aspiration: a case series and a systematic review
Highlight box
Key findings
• This study aimed to conduct a systematic review of 10 institutional cases and 18 literature cases to describe the clinical characteristics, imaging findings and treatment methods of acute transient thyroid swelling (ATTS).
What is known and what is new?
• ATTS is a rare but potentially important complication of fine-needle aspiration (FNA) in thyroid nodules. Despite its clinical relevance, there are few reports and case summary analyses in the literature.
• ATTS after FNA is self-limited and fatal in rare cases, with obvious ultrasonic manifestations.
What is the implication and what should change now?
• This study helps clinicians identify and pay attention to ATTS after FNA. Clinicians can select the appropriate treatment methods in time.
Introduction
Thyroid nodules are a common type of thyroid disease (1,2). According to different diagnostic techniques, the prevalence rate in the general population ranges from 2% to 65%. According to TIDE (Thyroid Disorders, Iodine Status, and Diabetes Epidemiological survey) research report, the prevalence rate of thyroid nodules with diameter >0.5 cm is 20.43% (3). Among them, the overall number of new cases and crude incidence rate (CIR) of thyroid cancer worldwide are on the rise (4). Fine-needle aspiration (FNA) is the gold standard for evaluating the benign and malignant thyroid nodules, and the incidence of complications is low (0.15%) (5). However, in recent years, cases of acute transient thyroid swelling (ATTS) after thyroid FNA have gradually emerged. ATTS is rare and self limiting. It is characterized by unilateral or bilateral rapid enlargement of the thyroid gland, accompanied by unique ultrasound findings. We systematically describe its clinical features, imaging findings and treatment by conducting a systematic review of 10 cases in our hospital and 18 cases in the literature. We present this article in accordance with the PRISMA and the AME Case Series reporting checklists (available at https://gs.amegroups.com/article/view/10.21037/gs-2025-66/rc).
Methods
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patients to publish this study and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Institutional cases
We analyzed and summarized the information from 10 cases of ATTS following FNA at our hospital between May 2018 and August 2024. This is a public tertiary hospital.
Characteristics of ATTS encompass (I) swift bilateral or unilateral enlargement of thyroid nodules during or after FNA; (II) a momentary and self-restricting nature; (III) distinctive ultrasound patterns depicting patchy and fissure-like appearances in the thyroid gland with either double or single lobes.
Follow-up
After FNA, the patients were evaluated and monitored every 0.5 hours until their ultrasound images returned to normal. The evaluation included the evaluation of thyroid ultrasound images and thyroid discomfort symptoms. The treatment strategy is observation and pressure treatment.
Literature
For the review, in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, we searched the PubMed, Embase, the Cochrane Library and Web of Science databases up to August 1, 2024 and performed a systematic review of ATTS following FNA using the following mesh terms in the title: “thyroid swelling”, “FNA”, “thyroid nodule”. These terms were combined with the term “acute transient thyroid swelling” and “fine-needle aspiration”. Items from the preliminary search were screened for duplicate items and then assessed for eligibility to be included. Two reviewers independently extracted articles with demographic and clinical characteristics. Finally, 18 relevant cases were extracted.
Collected clinical data were entered into a Microsoft Excel database, including year of publication, county, the first author, sex, age, history of allergy, nodule characteristics, symptom, onset of swelling, duration of swelling, needle gauge, degree of swelling, treatment, and cytological diagnosis.
The included studies in this paper are case reports, case series and non-controlled studies. The quality evaluation is carried out by using the JBI literature quality evaluation tool on descriptive studies (Table 1).
Table 1
| Entry | Evaluation results | |||
|---|---|---|---|---|
| Yes | No | Not clear | Not applicable | |
| 1. Are there a clear case inclusion criteria? | √ | |||
| 2. Is it ensured that standard and reliable methods are adopted to determine the disease or health problem of the case? | √ | |||
| 3. Is it ensured that effective methods are taken to diagnose diseases or health problems? | √ | |||
| 4. Is the inclusion of subjects in the case consistent? | √ | |||
| 5. Is the inclusion of research objects in the case comprehensive? | √ | |||
| 6. Whether the demographic information of the research object is clearly reported? | √ | |||
| 7. Is the clinical information of the subjects clearly reported? | √ | |||
| 8. Whether the outcome or follow-up results of the case are clearly reported? | √ | |||
| 9. Is the geographic and sociological information of the case clearly reported? | √ | |||
| 10. Is the statistical analysis method appropriate? | √ | |||
Inclusion criteria: (I) prospective or retrospective studies of acute goiter after FNA of thyroid nodules published before August 1, 2024; (II) complete case information.
Exclusion criteria: (I) acute goiter caused by other causes; (II) incomplete case information.
Results
Institutional cases
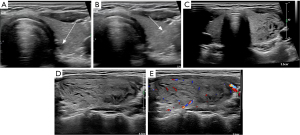
All ten cases in our study were female, with a median age of 40 years (ranging from 27 to 54 years). Among them, one case had elevated thyroid peroxidase antibodies, one case had elevated serum T3, and eight exhibited normal thyroid function. The average size of the punctured nodules was 8.7 mm (ranging from 2 to 19 mm). Bilateral involvement was observed in four cases, while unilateral involvement was noted in six cases. The average degree of thyroid swelling was 1.6 times (ranging from 1.1 to 3 times). Nine cases were asymptomatic, while one case reported swelling pain at the puncture site. Two cases underwent pressure treatment, while eight received no specific intervention, and the average recovery time for acute goiter was 5.2 hours (ranging from 1 to 23 hours). All ten cases exhibited the “crack sign” changes in the thyroid as observed through ultrasound. Pathological analysis revealed that four cases had benign outcomes and six cases had malignant findings (Table 2 and Figure 1).
Table 2
| Case | Sex | Age (years) | History of allergy | Nodule characteristics | Symptom | Onset of swelling | Duration of swelling | Needle gauge | Degree of swelling | Treatment | Cytological diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 40 | None | 4 mm, R lobe | Asymptomatic | During FNA | 4 h | 25 | R lobe 2.8 | Observation method | Benign |
| 2 | F | 35 | None | 5 mm, L lobe | Asymptomatic | During FNA | 2 h | 25 | Bilateral 3 | pressure treatment | Benign |
| 3 | F | 54 | None | 7 mm, L lobe | Asymptomatic | During FNA | 16 h | 25 | L lobe 1.6 | pressure treatment | PC |
| 4 | F | 35 | None | 16 mm, R lobe | Swelling | During FNA | 1.5 h | 25 | L lobe 1.2 | Observation method | Atypical cells |
| 5 | F | 41 | None | 17 mm, R lobe | Asymptomatic | During FNA | 23 h | 25 | R lobe 1.2 | Observation method | Benign |
| 6 | F | 37 | None | 2 mm, L lobe | Asymptomatic | During FNA | 1 h | 25 | R lobe 1.1 | Observation method | PC |
| 7 | F | 42 | None | 3 mm, R lobe | Asymptomatic | During FNA | 1 h | 25 | Bilateral 1.1 | Observation method | PC |
| 8 | F | 50 | None | 7 mm, R lobe | Asymptomatic | During FNA | 1 h | 25 | Bilateral 1.1 | Observation method | Benign |
| 9 | F | 27 | None | 19 mm, L lobe | Asymptomatic | During FNA | 1.5 h | 25 | L lobe 1.3 | Observation method | PC |
| 10 | F | 40 | None | 7 mm, R lobe | Asymptomatic | During FNA | 1 h | 25 | Bilateral 1.1 | Observation method | PC |
F, female; FNA, fine-needle aspiration; L, left; PC, papillary carcinoma; R, right.
Combined analysis
Among the 28 patients, 25 were female (89%), while three were male (11%). Bilateral goiter was present in 20 individuals (71%), and eight individuals (29%) exhibited unilateral goiter. ATTS manifested in 14 cases (50%) during the puncture process and in 14 cases (50%) at the conclusion of the puncture. Treatment approaches included medication in seven cases (25%) (involving pain relief, nonsteroidal anti-inflammatory drugs, or hormones), physical therapy in four cases (14%) (such as compression or ice compress) and endotracheal intubation therapy in one case (4%), while 16 patients (57%) did not receive any specific treatment. Within 24 hours, 22 patients (79%) returned to normal, and six patients (21%) experienced normalization after ≥24 hours. Symptoms of pain and swelling were reported in 15 cases (54%); symptoms of severe dyspnea and cardiac arrest were reported in one case (3%), while 12 cases (43%) were asymptomatic (Tables 2,3). The ultrasonic manifestations were: unilateral or bilateral goiter with linear, fissure-like low echo areas or patchy low echo areas, with no significant change in thyroid blood flow.
Table 3
| Study | Country | Sex | Age (years) | History of allergy | Nodule characteristics | Symptom | Onset of swelling | Duration of swelling | Needle gauge | Degree of swelling | Treatment | Cytological diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Haas SN, 1982 (6) | UK | F | 47 | None | 30 mm, R lobe | Moderate pain | 2–3 min after FNA | 1 h | 22 | Bilateral 2.5 | Ice compress | N/A |
| Dal Fabbro S, 1987 (7) | Italy | F | 63 | N/A | 38 mm, R lobe | Slight pain | Just after FNA | A few hours | 22 | Bilateral 3 | Ice compress | FC |
| Van den Bruel A, 2008 (8) | Belgium | M | 56 | None | 20 mm, L lobe | Neck pain | During FNA | 4 h | 24 | Bilateral 3 | Observation method | Medullary carcinoma |
| Norrenberg S, 2011 (9) | Belgium | F | 27 | None | 10 mm, L lobe | Pain | During FNA | 3 h | 21 | Bilateral 2 | NSAIDs | FC |
| Belgium | F | 46 | None | 15 mm, R lobe | Severe pain | Within 5 min after FNA | 4 days | 21 | Bilateral 2.9 | Pireparacetamol | Medullary carcinoma | |
| Nakatake N, 2012 (10) | Japan | F | 58 | None | 9 mm, L lobe | Slight pain | 1 h after FNA | A few hours | 22 | Bilateral 3 | Observation method | Benign |
| Japan | M | 31 | None | 15 mm, R lobe | Neck pain | 1.5 h after FNA | A few hours | 22 | Bilateral 2 | Observation method | Benign | |
| Japan | F | 45 | None | 24 mm, L lobe | Asymptomatic | 2 h after FNA | A few hours | 22 | Bilateral 2.5 | Observation method | Benign | |
| Yamada K, 2015 (5) | Japan | F | 50s | None | 14 mm, R lobe | Pain and tenderness | Just after FNA | 1.5 h | 22 | R lobe 3 | Observation method | N/A |
| Japan | F | 60s | None | 24 mm L/15 mm, R | Pain, slight dyspnea | 2 h after FNA | A few hours | 22 | Bilateral 12 | NSAIDs | R PC, L benign | |
| Japan | F | 70s | Penicillin and pyrazolone drugs | 1.1 cm, L/1.9 cm, R | Swelling | 1.5 h after FNA | 2 weeks | 22 | Bilateral 5 | Steroids | Benign | |
| Japan | F | 40s | None | 6 mm, R lobe | Asymptomatic | During FNA | 5.5 months | 22 | Bilateral 2 | Observation method | PC | |
| Tang WK, 2017 (11) | China | F | 68 | None | 26 mm, R lobe | Swelling and tenderness | 2–3 min after FNA | 22 h | 21 | Bilateral 5 | Observation method | FN |
| Zhu T, 2021 (12) | China | F | 30 | None | 13 mm, L/5 mm, R | Asymptomatic | During FNA | 0.5 h | 23 | L lobe 1.5 | Observation method | L benign, R atypical cells |
| Imaoka K, 2021 (13) | Japan | F | 26 | None | 14 mm, L lobe | Swelling and tenderness | 3 h after FNA | 18 h | 23 | Bilateral N/A | Steroids and H1 antihistamines | PC |
| Kim YK, 2022 (14) | Korea | F | 65 | N/A | 19.1 mm, L lobe | Neck pain, swelling, and shortness of breath | 1 h after FNA | 24 h | N/A | Bilateral 3 | Dexamethasone | N/A |
| Zeng W, 2022 (15) | China | M | 56 | None | 39 mm, R lobe | Pain | 0.5 h after FNA | 7 days | N/A | Bilateral 4.9 | Dexamethasone and furosemide | Benign |
| Yoshizawa S, 2023 (16) | Japan | F | 81 | None | L lobe | Severe dyspnea, cardiac arrest | 1.5 h after FNA | 4 days | 21 | Bilateral N/A | Endotracheal intubation | Benign |
F, female; FC, follicular carcinoma; FN, follicular neoplasm; FNA, fine-needle aspiration; L, left; M, male; N/A, not available; NSAID, non-steroidal anti-inflammatory drug; PC, papillary carcinoma; R, right.
Discussion
FNA is a straightforward, efficient, and safe technique for identifying the characteristics of thyroid nodules. Common complications encompass local pain (92%) and mild bleeding (3–26%) (15,17). The incidence of ATTS subsequent to thyroid FNA is infrequent, and was first reported by Haas in 1982 (6). Currently, only a limited number of cases have been reported. This summary and analysis of cases from our hospital and literature aim to enhance awareness among clinical and ultrasound practitioners regarding this uncommon complication and offer valuable clinical insights.
Etiology and pathogenesis
The mechanism behind ATTS after FNA remains unclear, and three current hypotheses have been proposed. The first hypothesis involves vasodilation and capillary leakage (5,15). Some scholars posit that puncturing thyroid nodules triggers local release of calcitonin-related peptide (CGRP), a potent endogenous vasodilator produced by the nervous system, which is known for causing vasodilation and is highly expressed in medullary thyroid cancer. Therefore, the levels of serum calcitonin measured increase (8). However, Norrenberg et al. argue that the CGRP hypothesis may not account for all cases (9). In this study, only two cases involved medullary carcinoma, providing insufficient evidence to support this notion. The alternative theory suggests that repeated punctures could lead to vascular injury, inducing local release of vasodilators and consequent vascular leakage. The second hypothesis is a hypersensitivity reaction mediated by thyroglobulin. Puncture disrupts thyroid follicles, leading to the release of thyroglobulin into the circulation. Thyroglobulin or other molecules may then trigger a self-reactive response within the thyroid (12,15). Mast cells become activated upon contact of the suction needle with the patient’s skin, leading to the release of histamine and other inflammatory mediators. Histamine can bind to four types of receptors. Among them, the binding of histamine to H1 receptors causes vasodilation and increased blood flow, leading to high permeability of postcapillary venules (18,19). This activation contributes to changes in vascular permeability, ultimately resulting in thyroid swelling. After the stimulus is removed, the patient undergoes self-recovery, and the substances in the body are gradually eliminated. Hence, vascular leakage alone cannot account for the short-term spontaneous recovery observed in ATTS after puncture (9). The third hypothesis involves intrathyroidal hemorrhage, which could result from focal thin-walled vascular rupture or vascular fistula within the thyroid parenchyma (20). However, the study by Dal Fabbro et al. on surgical exploration of patients with thyroid cancer-induced goiter after a puncture revealed no apparent hematoma signs outside or within the thyroid gland (7). The second hypothesis is favored, as the other two fail to explain the short-term recovery of diffuse bilobar goiter and goiter post-puncture. In our ten cases, an interesting observation is that some patients were punctured twice in different parts and on different days, but not all of them had ATTS, which requires further analysis and research.
Sonographic findings
ATTS subsequent to FNA typically presents the following ultrasonic features (10,15,17):
- Unilateral or bilateral acute enlargement of the thyroid gland.
- Linear, fissure-like hypoechoic areas or patchy hypoechoic areas within the thyroid gland. During or at the end of the thyroid puncture, it was found that the thyroid was diffusely distributed in one or both sides with strip-shaped low echo passing through the normal thyroid tissue, which was similar to the appearance of “plaque” or “crack”, indicating that there was thyroid parenchyma edema, which was characterized by transient rapid appearance and regression, accompanied by goiter, and this phenomenon was related to thyroid fine-needle puncture.
- Generally, no significant alterations in thyroid blood flow are observed.
- Most of them had no severe complications such as tracheal obstruction.
- The thyroid gland typically recovers within a short timeframe.
Among the 28 patients, 20 exhibited bilateral thyroid swelling, while eight had unilateral thyroid swelling, with bilateral occurrences being more prevalent.
A study has reported a 1.5 to 5 times increase in the degree of ATTS (average 2.5 times) (15). In our study, the thyroid volume in the 28 patients increased by 1.1 to 12 times (average 2.7 times). ATTS manifested in 14 cases after the conclusion of the puncture, occurring within 0 to 3 hours (average 1.01 hours). Inadequate time allowance following thyroid puncture may lead to the oversight of certain cases. Therefore, it is advisable to observe patients for a minimum of one hour post-puncture to promptly identify potential adverse reactions.
Prognosis and outcome
This study reports a case of severe complication, including dyspnea and cardiac arrest (16). The patient was an 81-year-old female who developed severe dyspnea 1.5 hours after FNA followed by cardiac arrest. Cardiopulmonary resuscitation and intubation were performed, and the thyroid function returned to normal after recovery. The patient was successfully discharged. Therefore, for patients with severe complications, early identification and active management of airway patency are key to treatment. It is also important to inform patients that complications may be delayed. For mild complications and asymptomatic patients, common treatment methods include drug therapy, physical therapy, and observation methods. Drug therapy comprises pain relief, nonsteroidal anti-inflammatory drugs, or hormone drugs, while physical therapy involves compression or ice compression. The observation method entails monitoring the self-recovery of the thyroid gland without specific treatment measures. It remains unclear from the literature whether steroid use affects the course or duration of ATTS, though case reports suggest that intravenous hydrocortisone administration may expedite recovery within 20 hours (13). In our study, seven cases (25%) received drug treatment, and 20 cases (71%) were managed without drugs. The recovery time with drug treatment ranged from several hours to one week (11,14). Conversely, all ten of our cases were treated without drugs, with an average recovery time of 5.2 hours. Therefore, for patients with mild symptoms, we recommend non-pharmacological treatment with continuous observation until the swelling significantly alleviates or disappears. For rare severe complications, active management is required to ensure airway patency. In our institutional case series, ATTS was identified during FNA in all patients, whereas only 4 of 18 patients reported in the literature developed ATTS during FNA procedures. Notably, we observed that ultrasonographic manifestations of ATTS preceded clinical symptoms in all cases. Among our 10 patients, unilateral or bilateral thyroid involvement was first detected through the emergence of linear or patchy hypoechoic areas on real-time ultrasound monitoring during FNA, with subsequent gradual thyroid enlargement. Only one patient developed palpable swelling, while the majority remained asymptomatic throughout the observation period. This discrepancy may be attributed to the procedural differences between institutions: our FNA operators are ultrasound specialists who maintain continuous imaging surveillance during procedures, potentially enhancing sensitivity to early sonographic changes. In contrast, clinicians performing FNA at other institutions may prioritize clinical symptom monitoring over imaging findings during the intervention. Therefore, real-time dynamic ultrasound detection during and after FNA may help to identify ATTS. Among the cases, 22 (79%) returned to normal within <24 hours, while six cases (21%) normalized in ≥24 hours. Prolonged observation intervals in some cases may contribute to extended recorded recovery times for thyroid swelling.
Limitations
This study searched the main databases, but some cases may have still been omitted. The incidence of acute goiter after FNA is low, and the observation time after puncture is not sufficient, resulting in some cases not being found, so these cases may not fully reflect the clinical manifestations, treatment and prognosis of the disease. There may be some heterogeneity among the cases selected in this study, such as the differences in the experience of thyroid fine needle puncture operators and the differences in ultrasound equipment, which need further study in the future.
Conclusions
ATTS following FNA is rare, self-limiting, and sonographically distinct. Clinicians should recognize its benign course in most cases while prioritizing airway management in severe presentations.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the PRISMA and the AME Case Series reporting checklists. Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-66/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-66/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-66/prf
Funding: This work was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-2025-66/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patients to publish this study and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Grani G, Sponziello M, Filetti S, et al. Thyroid nodules: diagnosis and management. Nat Rev Endocrinol 2024;20:715-28. [Crossref] [PubMed]
- Fiorentino V. The Role of Cytology in the Diagnosis of Subcentimeter Thyroid Lesions. Diagnostics (Basel) 2021;11:1043. [Crossref] [PubMed]
- Li Y, Teng D, Ba J, et al. Efficacy and Safety of Long-Term Universal Salt Iodization on Thyroid Disorders: Epidemiological Evidence from 31 Provinces of Mainland China. Thyroid 2020;30:568-79. [Crossref] [PubMed]
- Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2024;74:229-63. [Crossref] [PubMed]
- Yamada K, Toda K, Ebina A, et al. Ultrasonographic and non-enhanced CT features of acute transient thyroid swelling following fine-needle aspiration biopsy: report of four cases. J Med Ultrason (2001) 2015;42:417-25. [Crossref] [PubMed]
- Haas SN. Acute thyroid swelling after needle biopsy of the thyroid. N Engl J Med 1982;307:1349. [Crossref] [PubMed]
- Dal Fabbro S, Barbazza R, Fabris C, et al. Acute thyroid swelling after fine needle aspiration biopsy. J Endocrinol Invest 1987;10:105. [Crossref] [PubMed]
- Van den Bruel A, Roelandt P, Drijkoningen M, et al. A thyroid thriller: acute transient and symmetric goiter after fine-needle aspiration of a solitary thyroid nodule. Thyroid 2008;18:81-4. [Crossref] [PubMed]
- Norrenberg S, Rorive S, Laskar P, et al. Acute transient thyroid swelling after fine-needle aspiration biopsy: rare complication of unknown origin. Clin Endocrinol (Oxf) 2011;75:568-70. [Crossref] [PubMed]
- Nakatake N, Fukata S, Tajiri J. Acute transient thyroid swelling after fine-needle aspiration biopsy: three cases during only 6 weeks - a rare complication? Clin Endocrinol (Oxf) 2012;77:152-4. [Crossref] [PubMed]
- Tang WK, Bhatia KSS, Pang ASW, et al. Acute diffuse thyroid swelling: A rare complication of fine-needle aspiration. J Clin Ultrasound 2017;45:426-9. [Crossref] [PubMed]
- Zhu T, Yang Y, Ju H, et al. Acute thyroid swelling after fine needle aspiration-a case report of a rare complication and a systematic review. BMC Surg 2021;21:175. [Crossref] [PubMed]
- Imaoka K, Nishihara M, Nambu J, et al. Acute diffuse thyroid swelling after fine-needle aspiration: A case report and review of the literature. J Clin Ultrasound 2021;49:720-3. [Crossref] [PubMed]
- Kim YK, Goak IS, Kim YJ, et al. A rare case of acute transient thyroid swelling without hematoma after fine needle aspiration. Korean J Intern Med 2022;37:693-4. [Crossref] [PubMed]
- Zeng W, Lu J, Yan Z, et al. Acute transient thyroid swelling after fine-needle aspiration biopsy: A case report of a rare complication and a literature review. Diagn Cytopathol 2022;50:E193-7. [Crossref] [PubMed]
- Yoshizawa S, Nemoto C, Inoue S. Cardiopulmonary arrest caused by airway obstruction due to acute transient thyroid swelling after fine-needle aspiration biopsy. JA Clin Rep 2023;9:43. [Crossref] [PubMed]
- Polyzos SA, Anastasilakis AD. Clinical complications following thyroid fine-needle biopsy: a systematic review. Clin Endocrinol (Oxf) 2009;71:157-65. [Crossref] [PubMed]
- Nguyen SMT, Rupprecht CP, Haque A, et al. Mechanisms Governing Anaphylaxis: Inflammatory Cells, Mediators, Endothelial Gap Junctions and Beyond. Int J Mol Sci 2021;22:7785. [Crossref] [PubMed]
- Nakamura T, Murata T. Regulation of vascular permeability in anaphylaxis. Br J Pharmacol 2018;175:2538-42. [Crossref] [PubMed]
- Roh JL. Intrathyroid hemorrhage and acute upper airway obstruction after fine needle aspiration of the thyroid gland. Laryngoscope 2006;116:154-6. [Crossref] [PubMed]


