
Use of choline PET and ultrasound for preoperative localization of hyperfunctioning parathyroid glands: a single-institution retrospective cohort study
Highlight box
Key findings
• Choline positron emission tomography (PET) in combination with ultrasound (US) located enlarged parathyroid glands in all operated patients.
• A high proportion of patients (28%) had multiglandular disease in this selected patient cohort.
What is known and what is new?
• Choline PET is the most accurate method to detect hyperactive parathyroid glands.
• We show that US has additional value in the workup when performed by an experienced radiologist.
• US detected multiglandular disease as often as choline PET but had more false positives.
What is the implication, and what should change now?
• Choline PET in combination with US should be the new gold standard for detection of parathyroid disease.
Introduction
Hyperparathyroidism (HPT) is cured by removing hypersecreting parathyroid glands. These were traditionally identified during surgery by bilateral neck exploration. However, preoperative localization of the small and sometimes ectopic glands is associated with higher cure rates, while minimizing complications and duration of the surgery (1-3). Several studies in the last decade have shown the superiority of positron emission tomography (PET)/computed tomography (CT) or PET/magnetic resonance imaging (MRI) with fluorine-18 or carbon-11 labeled choline (choline PET) as compared to more commonly used imaging modalities such as ultrasound (US), scintigraphy with [99mTc]Tc-sestamibi (sestamibi), CT or MR (4-8). However, availability and cost are obstacles for many clinics to implement choline PET as the standard preoperative imaging modality for all patients with HPT.
When implementing an advanced imaging procedure such as choline PET as a clinical routine, it is important to examine the role of existing modalities such as US. US is cheap, irradiation-free, and has, in experienced hands, a high detection rate, but a disadvantage is high operator dependability and inability to detect all mediastinal and retrotracheal parathyroid lesions. The variance in detection rate is reported between 48.3% and 96.2% (9) for parathyroid disease and even lower for normal parathyroids (10).
The aim of this study was to evaluate the relative contribution of choline PET, and US performed by an experienced radiologist specialized in neck US, in selected patients with HPT. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-2025-12/rc).
Methods
We have retrospectively reviewed all patients (n=62) with HPT, including both primary HPT and HPT secondary to renal insufficiency, who had choline PET with fluorine-18 labeled choline in the University Hospital of North Norway from the introduction of the method in August 2019 to December 2022. Inclusion in the study was stopped at that time to allow sufficient time for most patients to be operated on at the time of data analysis. The indications for choline PET were negative or discordant preoperative localization studies, repeat surgery, or suspicion of multiglandular disease (independent of previous surgery). Routine preoperative localization for new patients with HPT at the time of the study was sestamibi scintigraphy and US. At the time of data analysis, 50 of the 62 patients had been operated on and these were analyzed separately, which allowed to calculate diagnostic performance using intraoperative findings as ground truth. Diagnostic accuracy for the choline PET and US was defined as true positives (TPs) and true negatives (TNs) divided by all evaluated glands. All patients were asked to leave blood samples 6 weeks and 6 months postoperatively.
US
US examinations were performed by the same operator (OIH), who was specialized in neck US and had over 15 years of experience. Two Philips Epiq 5G ultrasound machines (Philips Ultrasound, Bothell, WA, USA) with a L12-5 or eL18-4 PureWave transducer were used. In 37 out of 55 patients, US was performed before the choline PET. For the remaining 18, US was performed after PET, and choline PET images and/or the written PET report were available to the US operator. When US was performed before PET, the findings were available for the nuclear medicine physician reading the PET examination. US was performed before PET in 12 out of 15 patients (80%) with verified multiglandular disease during surgery. Seven patients had a PET scan but no US. Alle positive findings were described as either upper/lower left/right parathyroid gland.
PET imaging
[18F]F-choline was shipped from Curium Finland OY, Helsinki, Finland. Standard activity of 150 MBq ±5% was injected by an automatic injector (Posijet®, Lemer Pax, Brasil) 15–120 min (preferably 45–90 min) before start of imaging. Imaging was performed on a Siemens Biograph Vision PET/CT, Siemens mCT PET/CT, or on a Siemens Biograph mMR PET/MRI (all scanners: Siemens Healthineers, Forchheim, Germany) according to our standard clinical protocol. PET acquisition was from orbit to below the carina. Whether imaged on Biograph Vision PET/CT, mCT PET/CT, or Biograph mMR PET/MRI was determined based on internal logistics.
On the Biograph Vision PET/CT the acquisition was 1 bed of 10 min, while on the mCT PET/CT we imaged two beds of 15 min each. PET data were reconstructed with TrueX-TOF (Siemens Healtineers), with 4 iterations and 5 subsets. Full diagnostic dose CT without contrast was obtained during shallow breathing for attenuation correction and anatomic correlation (gantry rotation time 0.5 s, scan time 15 s, 200 mAs with the use of automatic current modulation, slice thickness 3 mm, incremental 3 mm).
For PET/MRI we imaged one bed (40 cm) for 15 min, no contrast used. The MR-sequences T1 and T2 Dixon were used. PET-data were reconstructed without time-of-flight (TOF) with point-spread function (PSF) by 4 iterations and 21 subsets. Image interpretation was performed using the integrated imaging software Syngo.via (Siemens Healthineers). Image interpretation was performed by a specialist in radiology and/or nuclear medicine or approved by such a specialist when primarily read by a resident. All positive findings were described as either upper/lower, left/right parathyroid gland.
Surgery
Five different consultant endocrine surgeons performed the surgeries. Intraoperative parathyroid hormone (PTH) was measured for all patients at the time of gland removal, and then after 5, 10 and 15 min in ethylenediamine tetraacetic acid (EDTA) blood samples analyzed with a standard two-site immunoassay. The operative strategy was focused parathyroidectomy if preoperative imaging suggested a single parathyroid adenoma. Bilateral exploration was performed in patients with suspected multiglandular disease. Bilateral exploration was also performed if focused parathyroidectomy did not result in a significant intraoperative PTH decrease, as evaluated by the operating surgeon. The surgeon reported whether the lesion or lesions removed corresponded with preoperative imaging or not. Each lesion was denominated as upper or lower right or left parathyroid and sent separately for histological evaluation.
Successful treatment was defined as normocalcemia on postoperative control (blood samples after 1–80 weeks, median 26 weeks) and histological verification of pathological parathyroid gland(s) in the surgical specimen(s).
Statistical analysis
All data was analyzed using Microsoft Excel and IBM SPSS. Statistical tests were performed with a 5% significance level. Mann-Whitney U tests were used for group comparisons of continuous variables and chi square for categorical variables. Specificity, sensitivity, positive and negative predictive values (NPVs) were calculated based on manual classification of TP, TN, false positive (FP) and false negative (FN) findings. Diagnostic accuracy was calculated as (TP + TN)/(TP + TN + FP + FN). Agreement between intraoperative findings and imaging was calculated by Cohen’s Kappa based on the number of lesions removed/detected. No substitution was performed for missing data.
Ethical considerations
The study was performed in accordance with the Declaration of Helsinki and its subsequent amendments. All patients signed a written informed consent form. The study was approved by the Data Protection Official (No. 02654) and the Norwegian Regional Ethics Committee North (No. 784535).
Results
Clinical outcomes
Out of 62 patients, 36 (58%) were female, the median age was 61.5 years, 21 had previous parathyroid surgery, 57 had primary HPT (pHPT) and five had secondary HPT (sHPT) (Figure 1, Table 1). Median free calcium level was 1.41 mmol/L, and median PTH was 12.2 pmol/L preoperatively. These demographic data were not significantly different for operated and unoperated patients (Table 1, Mann-Whitney U tests, P>0.5). Fifty-one of the 62 patients (85%) had a previous sestamibi scintigraphy with single-photon emission computerized tomography (SPECT)/CT, in which parathyroid disease was identified in 15 (29%). As selection to the study was partially based on negative or inconclusive scintigraphy, the diagnostic accuracy of sestamibi SPECT/CT was not further evaluated.
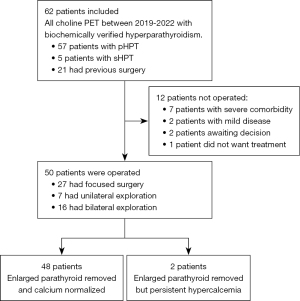
Table 1
| Characteristics | All patients (n=62) | Operated (n=50) | Unoperated (n=12) |
|---|---|---|---|
| Female gender | 36 [58] | 29 [58] | 7 [58] |
| Age (years) | 61.5 [28–84] | 61 [28–84] | 62.5 [36–83] |
| Calcium (mmol/L) | 2.67 [2.32–3.10] | 2.68 [2.35–3.10] | 2.65 [2.32–2.73] |
| Free calcium (mmol/L) | 1.41 [1.21–1.71] | 1.42 [1.21–1.71] | 1.38 [1.22–1.47] |
| PTH (pmol/L) | 12.2 [5.7–54.8] | 12.35 [5.7–43.8] | 10.8 [6.1–54.8] |
| Previous parathyroid surgery | 21 [34] | 17 [34] | 4 [33] |
| Secondary HPT | 5 [8] | 2 [4] | 3 [25] |
| Ultrasound results | |||
| Negative | 6 [10] | 5 [10] | 1 [8] |
| 1 lesion identified | 36 [58] | 28 [56] | 8 [67] |
| 2 lesions identified | 9 [15] | 9 [18] | 0 |
| 3 lesions identified | 1 [2] | 1 [2] | 0 |
| 4 lesions identified | 3 [5] | 3 [6] | 0 |
| Not performed | 7 [11] | 4 [8] | 3 [25] |
| Choline PET results | |||
| Negative | 4 [6] | 2 [4] | 2 [17] |
| 1 lesion identified | 41 [66] | 34 [68] | 7 [58] |
| 2 lesions identified | 12 [19] | 10 [20] | 2 [17] |
| 3 lesions identified | 2 [3] | 2 [4] | 1 [8] |
| 4 lesions identified | 3 [5] | 2 [4] | 1 [8] |
| Not performed | 0 | 0 | 0 |
Values are shown as number of patients [%] or median [range]. HPT, hyperparathyroidism; PET, positron emission tomography; PTH, parathyroid hormone.
Twelve of the 62 patients were not operated (Figure 1). Seven patients were recommended for observation because of severe comorbidity, and two patients with mild disease were also observed without surgery. Two patients are still awaiting clinical decision, while one patient declined surgical treatment. Among the 50 operated patients, abnormal parathyroid tissue was excised and verified histologically in all, and 48 (96%) became cured after surgery. In one patient with persisting disease, only one of two lesions visible on PET was removed. The patient had previously removed two parathyroid glands, and the surgeon did not want to risk iatrogenic hypoparathyroidism. The other patient with persisting disease had hyperplasia due to renal HPT. There were no intrathoracic or ectopic glands in our material.
Histological examination verified that parathyroid glands were removed from all the operated patients. A single gland was removed in 35 patients (70%), while multiple glands were removed in 15 patients (30%, Table 2). The intraoperative PTH dropped from a median pre-excision value of 13.3 (range, 4.7–51) to 3.4 (range, 1.4–28) pmol/L after 15 minutes. The median weight of the glands was 337 (range, 110–1,908) µg.
Table 2
| Characteristics | Values |
|---|---|
| Gland removed | |
| 1 | 35 [70] |
| 2 | 11 [22] |
| 3 | 2 [4] |
| 3.5 | 2 [4] |
| ioPTH (pmol/L) | |
| 0 min | 13.3 [4.7–51] |
| 15 min | 3.4 [1.4–28] |
| Parathyroid weight (µg) | 337 [110–1,908] |
| Free calcium at follow-up (mmol/L) | 1.26 [1.12–1.41] |
| Total calcium at follow-up (mmol/L) | 2.37 [2.18–2.64] |
| PTH at follow-up (pmol/L) | 5.3 [0.7–19] |
Values are shown as number of patients [%] or median [range]. ioPTH was recorded at the time of last gland excision (0 min) and 15 minutes later. ioPTH, intraoperative parathyroid hormone.
Diagnostic performance for all patients
Suspected abnormal parathyroid glands were identified on choline PET in 58 out of 62 patients (94%). Forty-one of these had one lesion, while the remaining 17 (27%) had multiple lesions (suspected multiglandular disease). US identified abnormal parathyroid glands in 49 out of 55 patients (89%). Multiple lesions were identified in 13 out of 55 patients (24%). Seven patients did not have a US performed.
Diagnostic performance for operated patients
The most correct estimation of diagnostic performance was calculated using data only from operated patients, in which ground truth was established from surgery and histological verification.
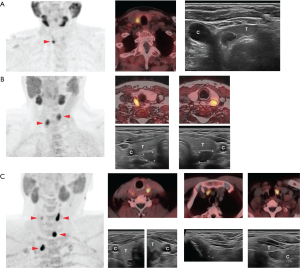
In a per-patient analysis, the combined use of US and PET detected hyperfunctioning parathyroid glands in all patients (100% sensitivity, Table 3). To assess the relative contribution of US and PET, we classified all findings as TP/FP and TN/FN, as compared to intraoperative findings. Choline PET had TP findings in 48 out of 50 operated patients (96%), and 2 had FN PET. These two patients had TP findings on US. US had TP findings in 36 of 46 patients (78%), 4 FPs and 6 FNs. Four patients had no pre-operative US. Thirty-four patients had one lesion on choline PET, while the remaining 14 (28%) had multiglandular disease. Multiglandular disease was identified by US in 13 of 46 patients (28%). Figure 2 shows example images of patients with multiglandular disease and solitary adenoma.
Table 3
| Characteristic | Ultrasound (n=46) | Choline PET (n=50) | Combined (n=50) |
|---|---|---|---|
| Sensitivity | 85.7% (71.5–94.5%) | 96.0% (86.3–99.5%) | 100% (92.9–100%) |
| PPV | 90.0% (88.8–91.1%) | 100% (92.6–100%) | 100% (92.9–100%) |
Confidence intervals in parenthesis. The combined use of ultrasound and choline PET detected all pathological parathyroid glands verified during surgery in 50 patients. PET, positron emission tomography; PPV, positive predictive value.
To evaluate the diagnostic accuracy of US and choline PET in more detail, we analyzed our data on a gland level (Table 4). The total number of glands was 176 (assuming 4 glands in every patient, minus any previously removed glands). Seventy-one glands were removed and histologically verified. We then compared the location of image findings to decide whether they matched the location of surgically removed parathyroid glands. Sixty-six glands were TP on PET, 106 were assumed TN, 4 were FN, and none were FP. This gave a sensitivity for choline PET of 94.3%, specificity of 100%, positive predictive value (PPV) of 100% and NPV of 96.4%. For US, 51 glands were TP, 93 were assumed TN, 13 were FN and 4 were FP. US had a sensitivity of 79.7%, specificity of 95.9%, PPV of 92.7% and NPV of 87.7% in our analysis. Diagnostic accuracy for the two methods, defined as TPs and TNs divided by all evaluated glands, was 98% for choline PET and 89% for US.
Table 4
| Characteristics | Ultrasound (n=157) | Choline PET (n=176) |
|---|---|---|
| Sensitivity | 79.7% (67.8–88.7%) | 94.3% (86.0–98.4%) |
| Specificity | 95.9% (89.8–98.9%) | 100% (96.6–100%) |
| PPV | 92.7% (82.9–97.1%) | 100% (94.6–100%) |
| NPV | 87.7% (81.5–92.1%) | 96.4% (91.1–98.6%) |
Confidence intervals in parenthesis. The per gland analysis illustrates the specificity of the imaging in more detail, as compared to Table 3. NPV, negative predictive value; PET, positron emission tomography; PPV, positive predictive value.
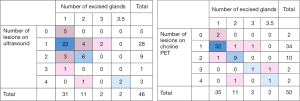
To further evaluate the clinical value of choline PET and US, we analyzed the correspondence between the number of glands removed during surgery and the number visualized on US or choline PET (Figure 3). The match between surgery and US was weak (Cohen’s Kappa 0.36, P<0.001) and the match between surgery and choline PET was moderate (Cohen’s Kappa 0.71, P<0.001), indicating that the surgeon was more informed by choline PET than by US.
Discussion
We have reported that, in selected patients with HPT, the diagnostic accuracy for choline PET and US was 98% and 89%, respectively. In the two patients with negative PET, US localized the adenomas, meaning that 100% of the patients had a TP localization when the two modalities were used in combination. This is consistent with previous reports of excellent choline PET localization of pathological parathyroid glands (6-8,11). This is the first study to find excellent performance of US in the same patient group.
A noteworthy finding in our study is that US identified multiglandular disease as frequently as PET. This is not reported in other studies and is probably explained by the narrow focus inherent to the US method. We speculate whether many physicians will conclude the examination once a pathological parathyroid gland has been identified and not continue searching for multiglandular disease. Our results show that it is indeed possible to localize multiglandular disease with US. It is also interesting that we found multiglandular disease in as many as 28% of the patients. A similar Swedish cohort found multiglandular disease in only 17% (6). The high incidence could be explained by a selection bias, but higher sensitivity of imaging methods is also likely to increase the proportion of patients found to have multiglandular disease. A weakness in our data is that we have mixed sHPT with pHPT. However, only two of the 15 operated patients with multiglandular disease had sHPT, so the bias introduced in the analysis is limited.
So far, there is only one published randomized controlled trial comparing choline PET to other imaging modalities (12). The retrospective nature of this study has its limits, especially in terms of patient selection. Inevitably, the indication for performing choline PET has not been very explicit. This introduces a selection bias in our results, like in most other studies. However, as the selection is predominantly towards “challenging cases”, we believe that performance of choline PET would be even better when tested on unselected HPT patients.
In many parts of the world, training in US skills is more achievable than establishing choline PET, while the opposite may be true in other parts of the world. Importantly, it is not sustainable healthcare to always recommend the most advanced and superior examination protocol in medicine. Most research focuses on defining the best available treatment or examination from a medical perspective, disregarding cost-benefit analysis or even side-effects and complications.
Good medical practice for preoperative localization of parathyroid disease the latest decades has been defined as using two different imaging modalities, typically US and sestamibi scintigraphy with SPECT/CT. This recommendation has emerged to compensate for the lack of accuracy in each available imaging method. We suggest a more pragmatic approach for the future, starting with US alone for new patients. We estimate that a large proportion of the patients will have a certain US finding that do not justify a second imaging procedure.
There are several limitations in this study. The sample size is small, and the retrospective design without planned inclusion criteria may have introduced selection biases in the data. The patient population is heterogenous, including two operated patients with sHPT. A single person performed all US examinations, limiting generalizability. The results of US or PET were not blinded for the interpreter of the other modality, thus, we cannot completely separate the performance of the two modalities. Availability of PET images to the radiologist could influence the detection, and vise versa. Our treatment results are to be considered as a combined effect of using the two modalities in conjunction, as they would be in a clinical setting. Comparison of PET/CT and PET/MRI was beyond the scope of this study. Choline PET/MRI has been effective for detection of parathyroid adenomas in at least one previous study, consistent with our findings (13). Another confounder in our results is that we changed from low-dose CT to full-dose CT without contrast halfway into the study period. We do not believe that this affected our results and conclusions.
Conclusions
Choline PET in combination with US performed by an experienced radiologist specialized in neck US provides reliable information in HPT patients with negative/discordant localization studies, reoperations, or suspected multiglandular disease. Both modalities detected the same proportion of multiglandular disease. Surgery in these patients had a very high success rate of 96%. The correspondence between lesions detected on choline PET and during surgery was excellent in our cohort, and enlarged parathyroid glands were found in all operated patients. Preoperative localization with US still has a value in difficult cases when performed by an experienced radiologist specialized in neck US.
Acknowledgments
We thank Martin Almquist for valuable comments on the manuscript.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-12/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-12/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-2025-12/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-2025-12/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was performed in accordance with the Declaration of Helsinki and its subsequent amendments. All patients signed a written informed consent form. The study was approved by the Data Protection Official (No. 02654) and the Norwegian Regional Ethics Committee North (No. 784535).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Udelsman R, Lin Z, Donovan P. The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg 2011;253:585-91. [Crossref] [PubMed]
- Kunstman JW, Udelsman R. Superiority of minimally invasive parathyroidectomy. Adv Surg 2012;46:171-89. [Crossref] [PubMed]
- Bergenfelz A, Lindblom P, Tibblin S, et al. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: a prospective randomized controlled trial. Ann Surg 2002;236:543-51. [Crossref] [PubMed]
- Mapelli P, Busnardo E, Magnani P, et al. Incidental finding of parathyroid adenoma with 11C-choline PET/CT. Clin Nucl Med 2012;37:593-5. [Crossref] [PubMed]
- Lee SW, Shim SR, Jeong SY, et al. Direct Comparison of Preoperative Imaging Modalities for Localization of Primary Hyperparathyroidism: A Systematic Review and Network Meta-analysis. JAMA Otolaryngol Head Neck Surg 2021;147:692-706. [Crossref] [PubMed]
- Murad H, Ciacoi-Dutu C, Lindblom G, et al. The role of (18)F-fluoromethylcholine-positron emission tomography-computed tomography for preoperative localization of hyperfunctioning parathyroid glands with special emphasis on multiglandular disease: a retrospective cohort study. Gland Surg 2023;12:1567-78. [Crossref] [PubMed]
- Quak E, Blanchard D, Houdu B, et al. F18-choline PET/CT guided surgery in primary hyperparathyroidism when ultrasound and MIBI SPECT/CT are negative or inconclusive: the APACH1 study. Eur J Nucl Med Mol Imaging 2018;45:658-66. [Crossref] [PubMed]
- Huber GF, Hüllner M, Schmid C, et al. Benefit of (18)F-fluorocholine PET imaging in parathyroid surgery. Eur Radiol 2018;28:2700-7. [Crossref] [PubMed]
- Cheung K, Wang TS, Farrokhyar F, et al. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol 2012;19:577-83. [Crossref] [PubMed]
- Ha TK, Kim DW, Jung SJ. Ultrasound detection of normal parathyroid glands: a preliminary study. Radiol Med 2017;122:866-70. [Crossref] [PubMed]
- Broos WAM, van der Zant FM, Knol RJJ, et al. Choline PET/CT in parathyroid imaging: a systematic review. Nucl Med Commun 2019;40:96-105. [Crossref] [PubMed]
- Quak E, Lasne-Cardon A, Cavarec M, et al. F18-Choline PET/CT or MIBI SPECT/CT in the Surgical Management of Primary Hyperparathyroidism: A Diagnostic Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg 2024;150:658-65. [Crossref] [PubMed]
- Araz M, Nak D, Soydal Ç, et al. Detectability of 18F-choline PET/MR in primary hyperparathyroidism. Eur Arch Otorhinolaryngol 2022;279:2583-9. [Crossref] [PubMed]


