
Long-term recurrence after parathyroidectomy in primary hyperparathyroidism—do predictors exist?
Highlight box
Key findings
• Postoperative parathyroid hormone (PTH) and calcium fluctuations after parathyroidectomy in primary hyperparathyroidism (pHPT) which highlight the importance of long-term follow-up.
What is known and what is new?
• Postoperative PTH elevations in parathyroidectomy in pHPT have been described in several studies. However, the long-term effects have so far been poorly studied.
• So far, it has been assumed that the recurrence rate is low. Recent findings from long-term studies provide indications of late recurrences.
What is the implication, and what should change now?
• The findings emphasize the importance of long-term follow-up in patients who have undergone parathyroidectomy and may help to guide the development of institutional postoperative checkups.
Introduction
Background
Primary hyperparathyroidism (pHPT) is the third most common endocrine disorder (1). Pathophysiologically, it is an excessive proliferation of the main cells of the parathyroid gland (2) which leads to a functional over-secretion of parathyroid hormone (PTH) and is manifested by an elevated PTH concentration (3). This leads to hypercalcemia, a key feature of pHPT. Effects may be nephrotic, osseous, gastrointestinal or neuro-psychiatric (4,5). Nowadays, the focus is on another notable entity of pHPT, normocalcemic pHPT (npHPT). It is characterised by a normal calcium level with elevated PTH. It is still classified as pHPT because of its symptomatic expression and clinical improvement after parathyroidectomy (6).
In 85% of cases, the disease is caused by a solitary parathyroid adenoma. In about 15% of cases, pHPT is due to multi-gland disease. Parathyroid carcinoma in pHPT occurs in less than 1% of cases.
Surgical removal, the so called parathyroidectomy, is the only curative treatment (5). Recent publications suggest that parathyroidectomy leads not only to a large increase in cure rates compared with medical therapy (7), but also results in a significant reduction in the overall risk of fracture (8).
By measuring intraoperative PTH (ioPTH), it is possible to determine whether all pathological glands have been removed (9). A parathyroidectomy is considered successful if hypercalcemia has been corrected and normocalcemia is present 6 months postoperatively. Cure rates of 95–99% should be achieved for initial procedures for solitary adenomas in sporadic pHPT. If the serum calcium concentration does not fall within the normal range after surgery or if hypercalcemia is detected within 6 months of postoperative normocalcemia, “persistent pHPT” is present (10). If hypercalcaemia occurs after half a year of normocalcemia, the condition is called “recurrent disease” (10).
Rationale and knowledge gap
Long-term follow-up for parathyroidectomy in pHPT has become increasingly important in recent years. In contrast to the previously thought recurrence rate of 0.7% in sporadic pHPT, new study results have observed late recurrence rates that pose new challenges for the surgical treatment of pHPT.
In 2017, Lou et al. published the results of 196 patients with a median follow-up duration of 9.2 years and showed a recurrence rate of 14.3% after 6.3 years (11). This result was significantly higher than previously thought. In 2020, Mallick et al. reported a recurrence rate of 10.7% in a similar study of 261 patients with a median follow-up period of 77 months. The development of recurrent diseases was reported up to 17 years later (12). However, the predictors or causes of late recurrence are still unclear.
Another phenomenon that has been in the focus of research for many years is a postoperative normocalcemic PTH elevation. It occurs in up to 46% of operated patients within the first weeks after surgery (13). There are many different hypotheses as to its pathogenesis and impact on the long-term outcome. In 2004, Nordenström et al. published a retrospective study in which they followed 99 operated patients for 5 years. Within 8 weeks, 28% of patients developed a normocalcemic PTH increase, for which they postulated to be associated with a higher risk of subsequent recurrence (14). Another long-term study was published in 2011, looking at the dynamics of postoperative PTH increases in 42 patients over a 10-year period (15). It concluded that this is a reversible, transient phenomenon that is not associated with subsequent disease recurrence (15). While several variables, including concentrations of the preoperative PTH and calcium concentrations as well as parathyroid glandular weight, have been discussed as possible causes, the preoperative creatinine may also be an important factor (16-18).
Objective
Sixty-five of 111 patients who underwent surgery for pHPT between 2007 and 2017 were evaluated over a postoperative period of up to 12.1 years. The aim of the study is to evaluate the treatment strategy of pHPT in endocrine surgery at the University Medical Center Rostock with regard to the long-term outcome. Special attention was paid to the postoperative development of PTH and calcium as compared to the preoperative state and to the question of whether there are predictors for late recurrence. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-24-116/rc).
Methods
Patient cohort
This study is based on a retrospective data analysis of a collective of 111 patients who underwent surgery for pHPT at the Department of General, Visceral, Thoracic, Vascular and Transplant Surgery at the University Medical Center Rostock (Germany) between 2007 and 2017, regardless of whether they had “classic” or “normocalcemic” pHPT.
Of these patients, 65 patients were followed up for a maximum of 12.1 years. The remaining 46 patients could not be included because of death or insufficient data, such as missing postoperative check-ups by the patients or missing answers to the questionnaire by doctors. In addition, only spontaneous, adenomatous disease was included. Syndromic cases of pHPT, such as multiple endocrine neoplasia or parathyroid carcinoma, as well as histological hyperplasia confirmed intraoperatively were excluded from the long-term follow-up.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Approval has been granted by the Ethics Committee of the University of Rostock, Germany (No. A 2020-0062). Informed consent was taken from all the patients.
Follow-up
A follow-up questionnaire was developed and sent to general practitioners or endocrinology specialists with the aim of obtaining postoperative follow-up examinations 6 months after parathyroidectomy or later.
It asked about calcium and PTH concentrations at the first postoperative outpatient visit, as well as postoperative complaints and medication in the form of calcium and/or vitamin D substitution were asked. The second part aimed to asses any persistent or recurrent disease and its treatment. The questions were formulated as “yes/no answers” and could be expanded individually by adding free text.
For the evaluation of the results, two dates were defined as follows: a first postoperative outpatient control as the first follow-up and a last available postoperative outpatient control as the second follow-up. This results in a “short-term follow-up” and “long-term follow-up”. In addition to these two endpoints, there was a “variable group” of 7 patients who were followed more closely over many years. The last measured value was used to evaluate the “long-term follow-up”.
Laboratory work-up
The standard laboratory values listed here refer to the Institute of Clinical Chemistry and Laboratory Medicine of the University Medical Center Rostock. The standard range for PTH is 15 to 65 pg/mL and refers to “intact” PTH. The measurement of calcium refers to total calcium in serum and is defined from 2.20 to 2.60 mmol/L. Concentrations outside these reference ranges are classified as “elevated”/“decreased” or “hypocalcemic”/“hypercalcemic”. The definition of ioPTH in this study is the lowest PTH value measured intraoperatively, 10 or 20 minutes after extirpation. Figure 1 provides an overview of the temporal definition of the laboratory parameters considered in this study.

In order to identify laboratory chemical abnormalities in the postoperative course, the patients were divided into a “remarkable” and an “unremarkable” group. Patients in the “remarkable” group had a PTH >60 pg/mL and/or a total calcium concentration >2.60 mmol/L at long-term follow-up. Conversely, the “unremarkable” group consisted of patients with unremarkable parameters at long-term follow-up.
Statistical analysis
The statistical analysis and the graphics were set by Microsoft Excel 2016 and SPSS Version 25.0.
Mean, standard deviation, median, minimum, and maximum were calculated to summarize the data. Primarily descriptive information and non-normally distributed data were presented as median and interquartile range (IQR).
Various tests were used to analyze the statistical significance of differences. The Mann-Whitney U test was used to compare two independent samples, and the Friedman test was used to compare paired samples.
Linear correlations were tested using Pearson’s correlation coefficient. Relationships between variables of interest were tested by regression analysis. Box plots show the median, the 25th and 75th percentiles as a box and the 10th and 90th percentiles as whiskers. Sample size is given as n.
The significance level of all tests was set to α=0.05 (P<0.05).
Results
Perioperative situation
The median age on the day of surgery was 60 (IQR, 52–71) years. The collective consisted of 76.9% (n=50/65) women and 23.1% (n=15/65) men. The preoperative serum calcium had a median of 2.8 (IQR, 2.68–2.87) mmol/L. The median preoperative PTH was 140.5 (IQR, 107–200) pg/mL. The median ioPTH was 26.4 (IQR, 20.2–39.5) pg/mL. There were no differences in laboratory parameters between age groups (P=0.10).
The median serum calcium concentration on the first postoperative day was 2.23 (IQR, 2.11–2.35) mmol/L, significantly lower than preoperatively (P<0.001). In 60% (n=39/65) of the cases the calcium concentration was in the normal range, 38.5% (n=25/65) showed a decreased concentration and 1.5% (n=1/65) an increased concentration.
The median PTH on postoperative day 1 was 16.8 (IQR, 9.5–31.9) pg/mL, which was significantly lower than preoperatively (P<0.001). Standard PTH was seen in 50% (n=32/64) of cases; 46.9% (n=30/64) of patients had a PTH below standard and 3.1% (n=2/64) had a PTH above standard. There were, as well, no differences between age groups (P=0.10) (Table 1).
Table 1
| Parameters | Preoperative | Intraoperative | Postoperative day 1 |
|---|---|---|---|
| PTH (pg/mL) | 140.5 [107–200] | 153.5 [129–350.25] | 16.8 [9.5–31.9] |
| Ca (mmol/L) | 2.8 [2.68–2.87] | 2.68 [2.61–3.09] | 2.23 [2.11–2.35] |
| ioPTH (pg/mL) | – | 26.4 [20.2–39.5] | – |
Data are presented as median [interquartile range]. PTH, parathyroid hormone; Ca, calcium; ioPTH, intraoperative parathyroid hormone.
Follow-up
Short-term follow-up
The first outpatient postoperative check was performed at a median of 17 (IQR, 7.5–46.5) days. The median serum calcium was 2.34 (IQR, 2.26–2.45) mmol/L and was significantly higher than on the postoperative day 1 (P=0.04). Normocalcemia was found in 84.7% (n=50/59) and hypocalcaemia in 13.6% (n=8/59) of the patients. Median PTH was 54.6 (IQR, 30.5–70.7) pg/mL. Fifty-two-point-three percent (n=23/44) of the patients had a normal PTH, 13.6% (n=6/44) had a decreased PTH and 34.1% (n=15/44) had an increased PTH.
The PTH values at the first follow-up were thus significantly higher than at the first postoperative day (P=0.009). This was due to postoperative PTH elevations, which were seen in 34.1% (n=15/44). These PTH increases developed after discharge from hospital in 93.3% of cases (n=14/15). The median PTH of the group with PTH elevation was 79.2 (IQR, 70.7–140.5) pg/mL, 21.8% above the upper limit of normal. Compared with patients without PTH elevation, the collective with PTH elevation did not differ in other parameters (Table 2).
Table 2
| Parameter | PTH elevated (n=15) | PTH not elevated (n=29) | P value |
|---|---|---|---|
| Age at the time of surgery (years) | 61 [53–70] | 62 [54–70] | 0.70 |
| Preop. PTH (pg/mL) | 169 [109–450] | 140 [90.65–159.5] | 0.09 |
| Preop. Ca (mmol/L) | 2.83 [2.7–3] | 2.75 [2.7–2.87] | 0.36 |
| ioPTH (pg/mL) | 28.4 [25–45] | 22.65 [19.1–33.42] | 0.06 |
| Preop. creatinine (µmol/L) | 70.5 [54.8–93.3] | 56.2 [64.5–72.3] | 0.24 |
| Postop. PTH (pg/mL) | 21 [9.5–32.3] | 16.8 [12–36.15] | 0.90 |
| Postop. Ca (mmol/L) | 2.22 [2.15–2.31] | 2.25 [2.16–2.37] | 0.23 |
| 1st FU: Ca (mmol/L) | 2.27 [2.33–2.44] | 2.46 [2.26–2.37] | 0.30 |
| 2st FU: PTH (pg/mL) | 47.3 [29–92] | 38.8 [23.8–51.8] | 0.20 |
| 2nd FU: Ca (mmol/L) | 2.4 [2.36–2.48] | 2.37 [2.28–2.47] | 0.50 |
Data are presented as median [interquartile range]. PTH, parathyroid hormone; FU, follow-up; Preop., preoperative; postop., postoperative; Ca, calcium; ioPTH, intraoperative parathyroid hormone.
The diagnosis of persistent pHPT was made in 4.6% (n=3/65) of the patients followed up. This included one patient who was already considered unhealed postoperatively due to an insufficient drop in PTH and persistent hypercalcaemia. Elevated values of both laboratory parameters were also confirmed in the first outpatient follow-up. During a further operation 5 months later, a fifth epithelial body was found on the left caudal side as an adenoma. The persistent diseases of the other two patients were detected during the outpatient follow-up examinations after 4 months. As the sonographic findings were unremarkable, no re-operations were performed. The calcium level had been successfully reduced by the last follow-up examination, 92 months after the diagnosis of persistent pHPT, through appropriate medication and follow-up checks.
Long-term follow-up
The second postoperative check took place at a median of 41 (IQR, 25–77) months. The median PTH was 43.50 (IQR, 28–66) pg/mL. Sixty-six-point-seven percent (n=30/45) had a normal PTH. PTH was decreased in 8.9% (n=4/45) and increased in 24.4% (n=11/45). A graphical representation of the change in PTH is summarized in Figure 2A. Correlation analysis showed that the PTH of the second control was significantly correlated with the PTH of the first control (r=0.36; P=0.04). A higher PTH in the first control leads to a higher PTH in the second control. The results of the regression analysis showed that this influence is robust compared to further PTH measurements. However, a correlation between the ioPTH and the PTH of the second control was not shown.
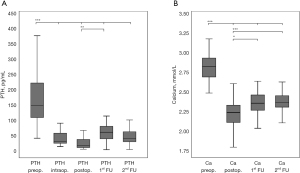
The median of the serum calcium was 2.36 (IQR, 2.30–2.49) mmol/L. Normal calcium values were found in 89.7% (n=52/58), decreased in 5.2% (n=3/58) and increased in 5.2% (n=3/58). Compared to serum calcium on postoperative day 1, it shows significantly higher values (P=0.009).
A graphical representation of calcium is summarized in Figure 2B.
Looking more closely at the long-term follow-up, 22% (n=13/59) emerged as the “remarkable” collective, characterized by the simultaneous presence of hypercalcaemia and PTH elevation or the isolated elevation of one of the two parameters.
In comparison, 78% (n=46/59) had normal laboratory parameters, the so-called “unremarkable” collective. The “remarkable” collective had significantly higher PTH levels than the “unremarkable” collective (P<0.001). Table 3 gives an overview of the variables included. A representation of the collectives based on the laboratory parameters of the first follow-up is shown in Figure 3A, that of the second follow-up in Figure 3B.
Table 3
| Parameters | “Remarkable” collective (n=46) | “Unremarkable” collective (n=13) | P value |
|---|---|---|---|
| Age at surgery (years) | 57.5 [48–68.25] | 61 [53–74] | 0.29 |
| Preop. PTH (pg/mL) | 140.5 [104–190.25] | 153.5 [129–350.25] | 0.09 |
| Preop. Ca (mmol/L) | 2.8 [2.68–2.87] | 2.68 [2.61–3.09] | 0.60 |
| Preop. creatinine (µmol/L) | 64.5 [54.2–74.8] | 86.85 [67.7–100.3] | 0.002 |
| ioPTH (pg/mL) | 26 [19.45–39.7] | 30.95 [24.1–46.5] | 0.11 |
| Postop. PTH (pg/mL) | 17.05 [8.69–26.95] | 17.4 [9.8–42] | 0.55 |
| Postop. Ca (mmol/L) | 2.23 [2.10–2.35] | 2.22 [2.06–2.26] | 0.51 |
| 1st FU: PTH (pg/mL) | 52.25 [30–71.65] | 79 [48.1–165] | 0.057 |
| 1st FU: Ca (mmol/L) | 2.33 [2.25–2.46] | 2.4 [2.26–2.44] | 0.91 |
| 2nd FU: PTH (pg/mL) | 32.5 [24–46] | 91 [67.35–99] | <0.001 |
| 2nd FU: Ca (mmol/L) | 2.36 [2.3–2.44] | 2.42 [2.32–2.68] | 0.18 |
Data are presented as median [interquartile range]. Preop., preoperative; postop., postoperative; PTH, parathyroid hormone; Ca, calcium; ioPTH, intraoperative parathyroid hormone; FU, follow-up.

Preoperative creatinine in the long-term course
The median preoperative creatinine was 66.2 (IQR, 54.6–82.3) µmol/L. In addition to the already mentioned significant difference in long-term PTH levels between the “remarkable” and the “unremarkable” collective, there was also a significant difference in the preoperative creatinine (P=0.002) (Table 2). Furthermore, there was a significant positive correlation between preoperative creatinine and PTH at the first follow-up (R2=0.288; P<0.001) (Figure 4A), as well as with PTH at the second follow-up (R2=0.366; P<0.001) (Figure 4B). A creatinine ≥75 µmol/L resulted in significantly higher PTH values at the first (P=0.045) and the second follow-up (P=0.02) than a creatinine value <75 µmol/L. When comparing these two groups, there was a significant difference in ioPTH (P=0.03).

Discussion
Key findings
Long-term observations after parathyroidectomy in pHPT have gained considerable importance in recent years with regard to postoperatively elevated laboratory parameters. In addition, postoperative transient PTH elevations may be difficult to distinguish from persistent pHPT, leading to controversial discussions and uncertainty in the management strategy of pHPT (13).
The present study analyzed the laboratory chemistry dynamics after parathyroidectomy over a median period of 41 months. In particular, the findings on PTH increases in the early postoperative period and the importance of perioperative laboratory parameters for the long-term course are discussed.
In the short-term follow-up of the current cohort, PTH levels were found be elevated in 34% of patients, and in 24.4% of patients in the long-term follow-up.
Strengths and limitations
The underlying study design was conducted with an acceptable follow-up rate of 62%. It allowed retrospective postoperative outpatient follow-up for up to 12.1 years.
However, there are undoubtedly limitations to this method, which severely restricted the collection of data. Incomplete questionnaires and a possible lack of comparability between different examiners and different laboratories must be mentioned. However, as there were no differences between the total and follow-up collectives, it can be assumed that the follow-up collective is a representative sample of the population considered here.
Comparison with similar research
Compared to previously published studies, normocalcemic PTH elevation in the early postoperative period occurs in 3–46% of cases (13) and is a well-recognized phenomenon that has been the subject of numerous investigations into its causes and implications for parathyroid surgery. While some authors consider postoperative PTH elevation to be a predictor of recurrence (14,19), the majority consider it to be a transient laboratory change that normalizes over time (15,20,21) or fluctuates (14,19). High preoperative PTH levels (14,19,22) and high PTH levels on postoperative day 1 (19) have been suggested as causes of postoperative PTH elevation. Vitamin D deficiency leading to a compensatory increase in PTH has also been suggested as a possible cause (23). Correlations with a high ioPTH (16) and a low ioPTH drop (24) are also discussed.
Many studies have investigated the role of perioperative PTH and calcium concentrations in long-term outcomes. Looking at the laboratory parameters at long-term follow-up compared with the levels at baseline in in this study, there were no differences. Therefore, at this point it can be assumed that preoperative calcium or PTH concentrations do not act as predictors of long-term outcome.
Mallick et al. came to the same conclusion in a retrospective long-term follow-up of 77 months (12). In contrast, Cron et al. concluded that a preoperative PTH of <99 pg/mL PTH and patients with a calcium concentration >11.2 mg/dL had a significantly worse outcome than patients with higher PTH concentrations or lower calcium concentrations. He studied a group of 2,239 patients in a retrospective study (25).
Preoperative creatinine was examined as another possible preoperative predictor. Studies had shown significantly higher preoperative creatinine levels in patients with postoperative PTH elevation compared to patients without PTH elevation (16-18).
Explanations of findings
There was no clear pre-, intra- or postoperative association for the described PTH increases in the present cohort. Possible vitamin D deficiency could not be assessed due to insufficient data. Preoperative calcium and PTH, as well as PTH on the postoperative day 1, did not differ between patients with and without postoperative PTH increases. It should be noted that seven patients in the follow-up group were followed very closely over several years compared to the rest of the group. These patients were found to have fluctuating elevated and normal PTH levels. A similar observation was also described by Nordenström et al. In his study concept of annual controls over 5 years, this “variable group” was clearly significant at over 40% (14). In the current study population, these patients had predominantly elevated laboratory values at the time of long-term follow-up and were therefore included in the “remarkable” group.
However, due to incomplete strict control, a higher percentage of fluctuating parameters can also be expected in this population. This reflects the complexity of unstable PTH and the need for frequent postoperative follow-up on the basis of the local data situation, which shows that the “variable group” in the current collective had significantly higher PTH values in the long-term follow-up, it would also be conceivable that the postoperative PTH increases take a fluctuating rather than a reversible course. This would also in line with the assumptions of Solorzano et al. (19).
Regarding the creatinine as another possible preoperative predictor, there were no differences in creatinine between the patients with postoperative PTH elevation and those without PTH elevation at short-term follow-up. The same was described by Westerdahl et al. (26). However, a highly significant difference was observed between the “remarkable” and “unremarkable” collective of the long-term follow-up. Similar results are described in the study by Hedbäck et al. He reported a higher recurrence rate in patients with elevated creatinine levels, although none of the patients had renal insufficiency (27). Furthermore, the preoperative creatinine correlated highly significantly with the PTH of the first and second postoperative control. This has already been described by Lundgren et al. and Rianon et al. (17,28). In addition, preoperative creatinine concentrations above 75 µmol/L correlated with significantly higher PTH concentrations at both short- and long-term follow-up. In conclusion, these results suggest that preoperative creatinine concentration may be a predictor of the early postoperative course as well as for the long-term course after parathyroidectomy in pHPT.
Implications and actions needed
This study looked at laboratory chemistry correlations after parathyroidectomy. A better understanding of this may significantly improve the outcome and postoperative management. Further studies beyond purely laboratory chemistry processes are needed to determine clinical relevance.
Conclusions
The large number of studies that have already addressed the question of how the laboratory parameters behave in the postoperative course after parathyroidectomy in pHPT reflects the general high surgical and endocrinological interest. This study investigated whether there are any predictors of late recurrences. The results show that the preoperative creatinine concentration may be a predictor of both early postoperative and long-term outcomes after parathyroidectomy in pHPT. Further laboratory chemistry dynamics in this study highlight the importance of postoperative controls beyond a period of 6 months and demonstrate the relevance of postoperative long-term follow-up in the management strategy of pHPT.
Acknowledgments
The authors thank all the general practitioners and endocrinologists, at this point in particular Ansgar Gordalla and his team (Endocrinologist, Rostock, Germany), who supported this study greatly.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-24-116/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-24-116/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-24-116/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-24-116/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Approval has been granted by the Ethics Committee of the University of Rostock, Germany (No. A 2020-0062). Informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Trébouet E, Bannani S, Wargny M, et al. Mild sporadic primary hyperparathyroidism: high rate of multiglandular disease is associated with lower surgical cure rate. Langenbecks Arch Surg 2019;404:431-8. [Crossref] [PubMed]
- Tfelt-Hansen J, Brown EM. The calcium-sensing receptor in normal physiology and pathophysiology: a review. Crit Rev Clin Lab Sci 2005;42:35-70. [Crossref] [PubMed]
- Walker MD, Silverberg SJ. Primary hyperparathyroidism. Nat Rev Endocrinol 2018;14:115-25. [Crossref] [PubMed]
- Dent RI, James JH, Want CA, et al. Hyperparathyroidism: gastric acid secretion and gastrin. Ann Surg 1972;176:360-9. [Crossref] [PubMed]
- Walker MD, Bilezikian JP. Primary hyperparathyroidism: recent advances. Curr Opin Rheumatol 2018;30:427-39. [Crossref] [PubMed]
- Wallace LB, Parikh RT, Ross LV, et al. The phenotype of primary hyperparathyroidism with normal parathyroid hormone levels: how low can parathyroid hormone go? Surgery 2011;150:1102-12. [Crossref] [PubMed]
- Pappachan JM, Lahart IM, Viswanath AK, et al. Parathyroidectomy for adults with primary hyperparathyroidism. Cochrane Database Syst Rev 2023;3:CD013035. [Crossref] [PubMed]
- Kongsaree N, Thanyajaroen T, Dechates B, et al. Skeletal impact of parathyroidectomy on patients with primary hyperparathyroidism: a Systematic review and Meta-analysis. J Clin Endocrinol Metab 2024;dgae326. [Crossref] [PubMed]
- Nussbaum SR, Thompson AR, Hutcheson KA, et al. Intraoperative measurement of parathyroid hormone in the surgical management of hyperparathyroidism. Surgery 1988;104:1121-7.
- Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg 2016;151:959-68. [Crossref] [PubMed]
- Lou I, Balentine C, Clarkson S, et al. How long should we follow patients after apparently curative parathyroidectomy? Surgery 2017;161:54-61. [Crossref] [PubMed]
- Mallick R, Nicholson KJ, Yip L, et al. Factors associated with late recurrence after parathyroidectomy for primary hyperparathyroidism. Surgery 2020;167:160-5. [Crossref] [PubMed]
- de la Plaza Llamas R, Ramia Ángel JM, Arteaga Peralta V, et al. Elevated parathyroid hormone levels after successful parathyroidectomy for primary hyperparathyroidism: a clinical review. Eur Arch Otorhinolaryngol 2018;275:659-69. [Crossref] [PubMed]
- Nordenström E, Westerdahl J, Bergenfelz A. Long-term follow-up of patients with elevated PTH levels following successful exploration for primary hyperparathyroidism. World J Surg 2004;28:570-5. [Crossref] [PubMed]
- Goldfarb M, Gondek S, Irvin GL 3rd, et al. Normocalcemic parathormone elevation after successful parathyroidectomy: long-term analysis of parathormone variations over 10 years. Surgery 2011;150:1076-84. [Crossref] [PubMed]
- Lang BH, Wong IY, Wong KP, et al. Eucalcemic parathyroid hormone elevation after parathyroidectomy for primary sporadic hyperparathyroidism: risk factors, trend, and outcome. Ann Surg Oncol 2012;19:584-90. [Crossref] [PubMed]
- Rianon N, Alex G, Callender G, et al. Preoperative serum osteocalcin may predict postoperative elevated parathyroid hormone in patients with primary hyperparathyroidism. World J Surg 2012;36:1320-6. [Crossref] [PubMed]
- Denizot A, Pucini M, Chagnaud C, et al. Normocalcemia with elevated parathyroid hormone levels after surgical treatment of primary hyperparathyroidism. Am J Surg 2001;182:15-9. [Crossref] [PubMed]
- Solorzano CC, Mendez W, Lew JI, et al. Long-term outcome of patients with elevated parathyroid hormone levels after successful parathyroidectomy for sporadic primary hyperparathyroidism. Arch Surg 2008;143:659-63; discussion 663. [Crossref] [PubMed]
- Mittendorf EA, McHenry CR. Persistent parathyroid hormone elevation following curative parathyroidectomy for primary hyperparathyroidism. Arch Otolaryngol Head Neck Surg 2002;128:275-9. [Crossref] [PubMed]
- Carsello CB, Yen TW, Wang TS. Persistent elevation in serum parathyroid hormone levels in normocalcemic patients after parathyroidectomy: does it matter? Surgery 2012;152:575-81; discussion 581-3. [Crossref] [PubMed]
- Duke WS, Kim AS, Waller JL, et al. Persistently elevated parathyroid hormone after successful parathyroid surgery. Laryngoscope 2017;127:1720-3. [Crossref] [PubMed]
- Carty SE, Roberts MM, Virji MA, et al. Elevated serum parathormone level after "concise parathyroidectomy" for primary sporadic hyperparathyroidism. Surgery 2002;132:1086-92; discussion 1092-3. [Crossref] [PubMed]
- Mizrachi A, Gilat H, Bachar G, et al. Elevated parathyroid hormone levels after parathyroidectomy for primary hyperparathyroidism. Head Neck 2009;31:1456-60. [Crossref] [PubMed]
- Cron DC, Kapeles SR, Andraska EA, et al. Predictors of operative failure in parathyroidectomy for primary hyperparathyroidism. Am J Surg 2017;214:509-14. [Crossref] [PubMed]
- Westerdahl J, Valdemarsson S, Lindblom P, et al. Postoperative elevated serum levels of intact parathyroid hormone after surgery for parathyroid adenoma: sign of bone remineralization and decreased calcium absorption. World J Surg 2000;24:1323-9. [Crossref] [PubMed]
- Hedbäck G, Odén A. Recurrence of hyperparathyroidism; a long-term follow-up after surgery for primary hyperparathyroidism. Eur J Endocrinol 2003;148:413-21. [Crossref] [PubMed]
- Lundgren E, Rastad J, Ridefelt P, et al. Long-term effects of parathyroid operation on serum calcium and parathyroid hormone values in sporadic primary hyperparathyroidism. Surgery 1992;112:1123-9.


