
Risk factors for increased drain output after endoscopic thyroidectomy via areola approach: a retrospective cohort study
Highlight box
Key findings
• We identified hyperthyroidism, operation time, and male gender as independent risk factors for increased drainage volumes (DV). These findings suggest that careful monitoring and management are crucial for patients with these risk factors, and postponing drain removal in patients with high DV in the early postoperative period may be warranted.
What is known and what is new?
• Endoscopic thyroidectomy (ET) offers superior cosmetic outcomes compared to traditional open thyroidectomy but is associated with higher postoperative DV and potential complications. Although ET via the areola approach (ETAA) has been used, the factors influencing DV after ETAA remain poorly understood.
What is the implication, and what should change now?
• This study enhances our understanding of the factors affecting DV after ETAA and highlights the need for tailored postoperative care strategies.
Introduction
In 1997, Hüsche successfully performed the first endoscopic thyroidectomy (ET) using a workable approach associated with favorable cosmetic results (1). ET is widely used in Chinese hospitals to treat thyroid goiter with good outcomes (2,3). However, ET may cause severe complications, including hematomas, because of the high vascularity of the thyroid gland (4). Further, ET produces a higher drainage volume (DV) than open thyroidectomy (OT). Therefore, inserting a drain during the subsequent procedure is essential to improve drainage in the previous period (5,6).
The need for suction drains in thyroid surgery is debatable (7-10). Although predictors of higher DV have been identified in patients who undergo thyroid lobectomy (11), little is known about the factors influencing DV after ET via the areola approach (ETAA). This study aimed to identify clinical risk factors for DV after ETAA. Further, these data can help physicians make informed decisions about the need for surgical drains in clinical practice. We present this article in accordance with STROBE reporting checklist (12) (available at https://gs.amegroups.com/article/view/10.21037/gs-24-360/rc).
Methods
Study participants
After applying the inclusion and exclusion criteria, 82 consecutive patients with thyroid disease who underwent ETAA at The First Affiliated Hospital of Jinan University from February to September 2016 under the supervision of an experienced surgeon were included in this retrospective cohort study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of The First Affiliated Hospital of Jinan University (approval No. KY-2023-197), and the requirement of individual consent for this retrospective analysis was waived. A medical team conducted all procedures according to the 2012 Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer (Chinese edition) (13).
Preoperative preparation and ETAA
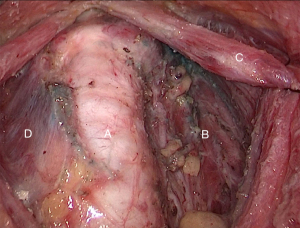
Preoperative preparation and ETAA were performed as described in our previous study, and a harmonic scalpel was used in all patients (14) (Full details of the procedures are described in Appendix 1). The surgical site was irrigated with sterile saline (200 mL, 100 mL at a time) and drained (Figure 1-3). Topical hemostatic agents were not used during the procedure because they might influence drainage output (15). A closed suction drain was placed in the surgical site before surgical closure (Figure 4,5). The most reliable approach involves the precise identification and dissection of blood vessels, followed by ligation or cauterization for vessel occlusion (16). During ETAA, our surgeon used meticulous techniques to minimize bleeding and achieve adequate hemostasis (14).




The laryngoscopy was performed before and after surgery to assess vocal cord mobility (17). Blood tests were performed to evaluate thyroid function, intact parathyroid hormone (IPTH) levels, serum Ca2+ levels, and coagulation function. Patients diagnosed with hyperthyroidism received antithyroid drugs for symptom control, followed by a three-week course of compound solution of iodine orally (14). The drain was removed within 24-h when the DV was less than 10 mL, as per the protocol used in The First Affiliated Hospital of Jinan University.
Data sources
Data were collected using standardized forms, and a database was created. The primary outcome was DV after ETAA. DV was measured every 24-h for three consecutive days postoperatively and classified as small, medium, or large (Table 1). Data on gender, age, body mass index (BMI), presence or absence of hyperthyroidism, operation time, exposure (or non-exposure) of the recurrent laryngeal nerve (Figures 6-8), type of thyroidectomy, and pathological diagnosis were obtained retrospectively from hospital records. Operation time was defined as the time from the first incision to suture placement. Continuous variables were converted to categorical variables, and clinical factors were categorized as shown in Table 1.
Table 1
| Characteristics | Values |
|---|---|
| DV | |
| First 24-hour DV (mL) | 75.95 [20–158] |
| Less (<60 mL) | 32 (39.0) |
| Middle (60–90 mL) | 25 (30.5) |
| More (>90 mL) | 25 (30.5) |
| Second 24-hour DV (mL) | 47.65 [15–94] |
| Less (<30 mL) | 21 (25.6) |
| Middle (30–60 mL) | 40 (48.8) |
| More (>60 mL) | 21 (25.6) |
| Third 24-hour DV (mL) | 22.72 [0–58] |
| Less (<15 mL) | 20 (24.4) |
| Middle (15–30 mL) | 37 (45.1) |
| More (>30 mL) | 25 (30.5) |
| Gender | |
| Male | 18 (22.0) |
| Female | 64 (78.0) |
| Age (years) | 38 [18–66] |
| ≥18, <28 | 22 (26.8) |
| ≥28, <38 | 18 (22.0) |
| ≥38, <48 | 21 (25.6) |
| ≥48, <58 | 16 (19.5) |
| ≥58 | 5 (6.1) |
| BMI (kg/m2) | 22.10 [15–31.5] |
| <24 | 62 (75.6) |
| ≥24, <28 | 16 (19.5) |
| ≥28 | 4 (4.9) |
| Hyperthyroidism | |
| Yes | 19 (23.2) |
| No | 63 (76.8) |
| Operation time (minutes) | 151.60 [80–309] |
| ≤100 | 9 (11.0) |
| >100, ≤150 | 35 (42.7) |
| >150 | 38 (46.3) |
| RLN exposure | |
| No | 16 (19.5) |
| single side | 34 (41.5) |
| both sides | 32 (39.0) |
| Type of surgery | |
| Unilateral | 20 (24.4) |
| Bilateral | 50 (61.0) |
| PCLND | 12 (14.6) |
| Pathological diagnosis | |
| Benign | 49 (59.8) |
| Diffuse goiter | 17 (20.7) |
| Malignant | 16 (19.5) |
Data are presented as median [range] or n (%). DV, drainage volume; BMI, body mass index; RLN, recurrent laryngeal nerve; PCLND, prophylactic central cervical lymph node dissection.



Statistical analysis
After adjusting for potential confounders, univariate and ordinal logistic regression analyses evaluated the association between DV and clinical variables. The frequencies of categorical variables were compared using the Pearson Chi-squared test, and the factors influencing DV were identified by univariate analysis. Risk factors were identified by ordinal logistic regression analysis. All tests were two-sided, and the significance level was set at 0.05. Diagnostic data were plotted against predicted values, and estimated values and Pearson and deviance residuals were used to identify outliers and influential factors. All variables included in the regression analysis were used in the imputation process. Statistical analysis was performed using the Statistical Package for the Social Sciences version 25 (IBM Corp, Armonk, NY, USA).
Results
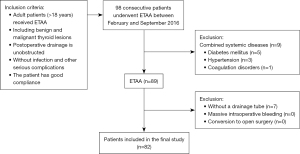
Ninety-eight consecutive patients underwent ETAA between February and September 2016 at The First Affiliated Hospital of Jinan University. Of these, 16 patients (nine had underlying diseases, and seven underwent surgery without drain placement) were excluded from the study (Figure 9). After applying the inclusion and exclusion criteria, 82 patients (18 men and 64 women) with complete data were included in the analysis. In addition, 74.4% were younger than 48 years, 24.4% were overweight or obese (BMI ≥24 kg/m2), and 23.2% had hyperthyroidism. No postoperative complications have been documented. None of our patients had a massive hemorrhage or required conversion to open surgery. The demographic and clinical characteristics of the cohort are shown in Table 1.
Univariate analysis
The results of the Pearson Chi-squared test showed that hyperthyroidism (P=0.03) and operation time (P=0.001) were significantly correlated with DV in the first 24-h postoperatively (Table 2). Furthermore, there was a significant association between gender (P=0.03), hyperthyroidism (P=0.03), operation time (P=0.02), and the first 24-h DV (P<0.001) with the second 24-h DV. The first 24-h DV (P=0.005) and second 24-h DV (P<0.001) were significantly linked with the third 24-h DV.
Table 2
| Factors | First 24-hour drainage volume | Second 24-hour drainage volume | Third 24-hour drainage volume | |||||
|---|---|---|---|---|---|---|---|---|
| χ2 | P | χ2 | P | χ2 | P | |||
| Gender | 4.604 | 0.10 | 6.823 | 0.03* | 4.144 | 0.13 | ||
| Age | 0.742 | 0.39 | 0.749 | 0.39 | 2.940 | 0.09 | ||
| BMI | 2.104 | 0.15 | 3.784 | 0.052 | 0.241 | 0.62 | ||
| Hyperthyroidism | 7.408 | 0.03* | 6.995 | 0.03* | 3.476 | 0.18 | ||
| Operation time | 11.936 | 0.001* | 5.249 | 0.02* | 2.808 | 0.09 | ||
| Type of surgery | 7.918 | 0.10 | 6.843 | 0.14 | 4.723 | 0.32 | ||
| RLN exposure | 4.101 | 0.39 | 3.775 | 0.44 | 1.655 | 0.80 | ||
| Pathological diagnosis | 9.250 | 0.16 | 8.301 | 0.22 | 9.297 | 0.054 | ||
| First 24-hour drainage volume | – | – | 16.549 | <0.001* | 7.711 | 0.005* | ||
| Second 24-hour drainage volume | – | – | – | – | 23.115 | <0.001* | ||
*, P value <0.05, with statistical significance. ETAA, endoscopic thyroidectomy via areola approach; BMI, body mass index; RLN, recurrent laryngeal nerve.
Model diagnostic checking
We further make a model diagnostic to assess the reliability of the ordinal logistic regression analysis. Model fitting showed that some clinical factors were significantly associated with DV at different time points (*P<0.001; *P<0.05 indicates statistically significant) (Table 3). Pearson (†P=0.98, 0.47, 0.93; †P>0.05 indicates that the model fits better or the hypothesis is valid) and Deviance Chi-squared test (†P=0.94, 0.25, 0.86) results indicated that the multinomial regression model exhibited a superior fit and demonstrated high reliability (†P>0.05). According to the general model (†P=0.95, 0.43, 0.82), it leads to the failure of rejecting the null hypothesis that the parallel lines assumption holds or that the coefficients do not differ across thresholds for the outcome variable (†P>0.05). Therefore, the ordinal regression model was appropriate for this dataset.
Table 3
| Test item | Model/method | P value | ||
|---|---|---|---|---|
| First 24-hour drainage volume | Second 24-hour drainage volume | Third 24-hour drainage volume | ||
| Model fitting information* | Final | <0.001 | <0.001 | <0.001 |
| Goodness-of-fit† | Pearson | 0.98 | 0.47 | 0.93 |
| Deviance | 0.94 | 0.25 | 0.86 | |
| Test of parallel line† | General | 0.95 | 0.43 | 0.82 |
*, P<0.05 model is statistically significant; †, P>0.05 indicates that the model fits better or the hypothesis is valid. ETAA, endoscopic thyroidectomy via areola approach.
Ordinal logistic regression analysis
The results of ordinal logistic regression analysis showed a significant association of hyperthyroidism [odds ratio (OR) exp (B) =2.97; P=0.049] and operation time [≤100 min (OR =0.11; P=0.02) and >100, ≤150 min (OR =0.39; P=0.049)] with DV in the first 24-h (Table 4), indicating that hyperthyroidism and longer operation time were associated with a higher risk of having larger DV. Furthermore, there was a significant association between the male gender (OR =0.23; P=0.02) and hyperthyroidism (OR =3.56; P=0.04), with the second 24-h DV and a significant association between the second 24-h DV [<30 mL (OR =0.04; P<0.001) and 30–60 mL (OR =0.22; P=0.01)] and third 24-h DV.
Table 4
| Factors | B | S.E. | Wald | OR | 95% CI | P | |
|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||||
| First 24-hour drainage volume | |||||||
| Hyperthyroidism | 1.09 | 0.56 | 3.87 | 2.97 | 1.00 | 8.85 | 0.049* |
| Operation time | |||||||
| ≤100 minutes | −2.18 | 0.90 | 5.86 | 0.11 | 0.02 | 00.66 | 0.02* |
| >100, ≤150 minutes | −0.94 | 0.48 | 3.89 | 0.39 | 0.15 | 0.99 | 0.049* |
| >150 minutes | – | – | – | 1.00 | – | – | – |
| Second 24-hour drainage volume | |||||||
| Male gender | −1.46 | 0.61 | 5.65 | 0.23 | 0.07 | 0.77 | 0.02* |
| Hyperthyroidism | 1.27 | 0.61 | 4.29 | 3.56 | 1.07 | 11.82 | 0.04* |
| Operation time | |||||||
| ≤100 minutes | −0.42 | 0.80 | 0.27 | 0.66 | 0.14 | 3.16 | 0.60 |
| >100, ≤150 minutes | −0.54 | 0.50 | 1.19 | 0.58 | 0.22 | 1.54 | 0.28 |
| >150 minutes | – | – | – | 1.00 | – | – | – |
| First 24-hour drainage volume | |||||||
| <60 mL | −1.59 | 0.64 | 6.17 | 0.20 | 0.06 | 0.71 | 0.053 |
| 60–90 mL | −0.98 | 0.59 | 2.74 | 0.38 | 0.12 | 1.20 | 0.10 |
| >90mL | – | – | – | 1.00 | – | – | – |
| Third 24-hour drainage volume | |||||||
| First 24-hour drainage volume | |||||||
| <60 mL | −0.47 | 0.59 | 0.63 | 0.62 | 0.19 | 1.99 | 0.43 |
| 60–90 mL | 0.16 | 0.58 | 0.08 | 1.17 | 0.38 | 3.67 | 0.78 |
| >90 mL | – | – | – | 1.00 | – | – | – |
| Second 24-hour drainage volume | |||||||
| <30 mL | −3.16 | 0.78 | 16.64 | 0.04 | 0.01 | 0.19 | <0.001* |
| 30–60 mL | −1.50 | 0.59 | 6.54 | 0.22 | 0.07 | 0.70 | 0.01* |
| >60 mL | – | – | – | 1.00 | – | – | – |
*, P value <0.05, with statistical significance. ETAA, endoscopic thyroidectomy via areola approach; B, regression coefficient; S.E., standard error; OR, odds ratio = exp (B); CI, confidence interval for OR [exp (B)].
Discussion
Surgical drains increase postoperative pain and hospital length of stay and do not decrease reoperation rates, hematomas, and seroma formation in patients undergoing OT (18). ETAA is a new surgical technique that is constantly being improved. The need for using surgical drains in OT is controversial, and more evidence to support its effectiveness in ETAA is needed (19-22). Drainage is recommended for thyroid surgery patients with extensive dead space (23). Further, drains should be used cautiously after ETAA because this technique requires broader flap separation and may increase bleeding compared to OT. Notwithstanding, using an indwelling tube allows for detecting bleeding and estimating blood loss during surgery. A survey conducted among 35 surgeons across ten units revealed significant heterogeneity in indications for drain insertion and decisions on removal (24), underscoring the need to develop objective methods to improve decision-making. In early practice, we used drainage tubes in most ETAA cases, and the decision not to use drains was made on a case-by-case basis. Moreover, clinical risk factors for DV after ETAA were unknown in previous studies. In this study, our findings suggest that drains should be used cautiously in male patients and patients with hyperthyroidism and in cases involving longer operation times.
ETAA was safe and effective for treating hyperthyroidism in our cohort, and none of the patients with hyperthyroidism who underwent ETAA had severe postoperative complications. Hyperthyroidism is characterized by enlarged thyroid glands with high vascularity and poor hemostasis. Although hyperthyroidism is treated successfully using ET, there is disagreement on the best surgical treatment approach (25,26). To resolve this controversy, we previously performed a meta-analysis comparing ET and OT for hyperthyroidism. ET was associated with better patient satisfaction and less blood loss, albeit operation time increased. Nonetheless, the rates of adverse events and complications were similar between the two procedures (27). The efficacy of OT for hyperthyroidism is 92%, but it necessitates a cervical collar incision that resembles an anterior neck scar associated with self-harm (28). Thus, OT is not advisable to patients who value aesthetics, and ETAA with concealed incisions is a novel treatment for thyroid disorders.
A meta-analysis showed that hyperthyroidism was a significant risk factor for hematoma after thyroidectomy (29). Consistent with this result, we found that hyperthyroidism was a risk factor for higher DV within 48-h after ETAA. Furthermore, the results showed that drain placement and removal might be necessary for patients with hyperthyroidism. The ordinal logistic regression analysis revealed a significant association between the second 24-h and third 24-h DV following ETAA, indicating that patients with higher DV during the second 24-h period are at an increased risk of having larger DV on the third 24-h period. Therefore, drains are safer to be removed from patients with lower DV (second 24-h period <30 mL).
Operation time was significantly positively correlated with DV in the first 24-h after ETAA, consistent with a previous study in patients with OT (11). Moreover, 66% of patients with operation time longer than 150 min are hyperthyroidism or malignant tumors and have more DV. Thus, DV may be associated with the surgical extent, BMI, thyroid gland size, and other factors influencing the operative time (30). However, surgical experience and reduced operative time minimize these effects (31).
The findings showed that men had a higher DV in the second 24-h period than women, consistent with a previous study in patients with OT (11). Although the reasons for this sex difference are unclear, we have previously demonstrated that ETAA procedures in male patients are characterized by longer operation times, higher blood loss, and greater complexity than in female patients (32). Furthermore, there are sex differences in humoral immunity and responses to trauma (33,34), and the efficiency of skeletal muscle regeneration is higher in women than men (35). Wound healing is a complex process influenced by extracellular matrix molecules, inflammatory mediators, and different cell types, including fibroblasts, keratinocytes, and leukocytes (36). Furthermore, this process is accompanied by the exudation of blood or interstitial fluid, which can be drained.
Limitations
There are limitations in this study. First, the study had a retrospective single-center design and a small sample size. Second, the effects of tumor size and weight were not assessed. Therefore, we intend to incorporate it into future research endeavors, and more extensive multicenter prospective trials are needed to validate our results. Third, the study did not include patients with other diseases or complications; no massive hemorrhage and conversion to open surgery. Thus, the effects of comorbidities on the surgical outcome warrant further investigation, and the comprehensive assessment of the safety and efficacy of different drainage outputs after surgery necessitates a more extended follow-up period.
Conclusions
Hyperthyroidism, longer operation time, and male gender were independent risk factors for high DV after ETAA. Therefore, patients with these risk factors should be closely monitored intraoperatively to maintain hemostasis. Additionally, the DV in the second 24-h period after ETAA was an independent risk factor for DV in the third 24-h period, suggesting that drain removal should be postponed in patients with a large DV (>30 mL) in the second 24-h period.
Acknowledgments
Funding: This study was supported by a grant from
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-24-360/rc
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-24-360/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-24-360/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-24-360/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hüscher CS, Chiodini S, Napolitano C, et al. Endoscopic right thyroid lobectomy. Surg Endosc 1997;11:877. [Crossref] [PubMed]
- Zhang W, Jiang DZ, Liu S, et al. Current status of endoscopic thyroid surgery in China. Surg Laparosc Endosc Percutan Tech 2011;21:67-71. [Crossref] [PubMed]
- Ng WT. Endoscopic thyroidectomy in China. Surg Endosc 2009;23:1675-7. [Crossref] [PubMed]
- Chen E, Cai Y, Li Q, et al. Risk factors target in patients with post-thyroidectomy bleeding. Int J Clin Exp Med 2014;7:1837-44.
- Woo SH, Kim JP, Park JJ, et al. Comparison of natural drainage group and negative drainage groups after total thyroidectomy: prospective randomized controlled study. Yonsei Med J 2013;54:204-8. [Crossref] [PubMed]
- Zhang Q. The non-randomized clinical study of open thyroidectomy in differentiated thyroid carcinoma compare with endoscopic surgery. China: Jinan University; 2008.
- Shaha AR, Jaffe BM. Selective use of drains in thyroid surgery. J Surg Oncol 1993;52:241-3. [Crossref] [PubMed]
- Schoretsanitis G, Melissas J, Sanidas E, et al. Does draining the neck affect morbidity following thyroid surgery? Am Surg 1998;64:778-80.
- Morrissey AT, Chau J, Yunker WK, et al. Comparison of drain versus no drain thyroidectomy: randomized prospective clinical trial. J Otolaryngol Head Neck Surg 2008;37:43-7.
- Mekel M, Stephen AE, Gaz RD, et al. Surgical drains can be safely avoided in lateral neck dissections for papillary thyroid cancer. Am J Surg 2010;199:485-90. [Crossref] [PubMed]
- Chen CY, Chiu YL, Rajbhandari S, et al. Predictive factors of increased surgical drain output after thyroid lobectomy: a retrospective study. Gland Surg 2019;8:542-9. [Crossref] [PubMed]
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495-9. [Crossref] [PubMed]
- Endocrinology Branch of Chinese Medical Association, Surgery Branch of Chinese Medical Association, Head and Neck Tumour Committee of Chinese Anti-Cancer Association, et al. Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer (Chinese edition). Chinese Journal of Endocrinology and Metabolism 2012;39:1249-72.
- Wang C, Feng Z, Li J, et al. Endoscopic thyroidectomy via areola approach: summary of 1,250 cases in a single institution. Surg Endosc 2015;29:192-201. [Crossref] [PubMed]
- Docimo G, Filograna Pignatelli M, Ferrandes S, et al. Role of Absorbable Polysaccharide Hemostatic Powder in the Prevention of Bleeding and Wound Events after Thyroid Surgery. J Clin Med 2023;12:5684. [Crossref] [PubMed]
- Khadra H, Bakeer M, Hauch A, et al. Hemostatic agent use in thyroid surgery: a meta-analysis. Gland Surg 2018;7:S34-41. [Crossref] [PubMed]
- Fu J, Zhao Y, Sun H, et al. The feasibility of laryngeal nerve protection during thyroidectomy using sternocleidomastoid intermuscular approach with intraoperative neuromonitoring: a case series and step-by-step description of surgical procedure. Gland Surg 2022;11:1665-72. [Crossref] [PubMed]
- Portinari M, Carcoforo P. The application of drains in thyroid surgery. Gland Surg 2017;6:563-73. [Crossref] [PubMed]
- Tabaqchali MA, Hanson JM, Proud G. Drains for thyroidectomy/parathyroidectomy: fact or fiction? Ann R Coll Surg Engl 1999;81:302-5.
- Hurtado-López LM, López-Romero S, Rizzo-Fuentes C, et al. Selective use of drains in thyroid surgery. Head Neck 2001;23:189-93. [Crossref] [PubMed]
- Chen GX, Li C, Zhang H. Drainage During Endoscopic Thyroidectomy. JSLS 2019;23:e2018.00060.
- Chen Y, Wang C, Bai B, et al. Drainage Tube Placement May Not Be Necessary During Endoscopic Thyroidectomy Bilateral Areola Approach: A Preliminary Report. Front Surg 2022;9:860130. [Crossref] [PubMed]
- Deveci U, Altintoprak F, Sertan Kapakli M, et al. Is the use of a drain for thyroid surgery realistic? A prospective randomized interventional study. J Thyroid Res 2013;2013:285768. [Crossref] [PubMed]
- Keane E, Fitzgerald CW, Smyth DA, et al. Drain Usage in Head and Neck Surgery: A National Survey of Thirty-five Surgeons across Ten Units. Ir Med J 2018;111:839.
- Sasaki A, Nitta H, Otsuka K, et al. Endoscopic subtotal thyroidectomy: the procedure of choice for Graves' disease? World J Surg 2009;33:67-71. [Crossref] [PubMed]
- Vaysberg M, Steward DL. Minimally invasive video-assisted thyroidectomy. Laryngoscope 2008;118:786-9. [Crossref] [PubMed]
- Zhang Y, Dong Z, Li J, et al. Comparison of endoscopic and conventional open thyroidectomy for Graves' disease: A meta-analysis. Int J Surg 2017;40:52-9. [Crossref] [PubMed]
- Palit TK, Miller CC 3rd, Miltenburg DM. The efficacy of thyroidectomy for Graves' disease: A meta-analysis. J Surg Res 2000;90:161-5. [Crossref] [PubMed]
- Quimby AE, Wells ST, Hearn M, et al. Is there a group of patients at greater risk for hematoma following thyroidectomy? A systematic review and meta-analysis. Laryngoscope 2017;127:1483-90. [Crossref] [PubMed]
- Sun H, Liu Z, Gao H, et al. Predictive factors for prolonged operative time of robotic thyroidectomy via bilateral axillo-breast approach: Analysis of 359 cases of differentiated thyroid cancer. Asian J Surg 2022;45:105-9. [Crossref] [PubMed]
- Lira RB, Ramos AT, Nogueira RMR, et al. Transoral thyroidectomy (TOETVA): Complications, surgical time and learning curve. Oral Oncol 2020;110:104871. [Crossref] [PubMed]
- Feng Z, Li J, Wang C. The difficulties and the countermeasures of endoscopic thyroidectomy via areola approach for male patients. Journal of Laparoscopic Surgery 2014;19:271-4.
- Choudhry MA, Bland KI, Chaudry IH. Gender and susceptibility to sepsis following trauma. Endocr Metab Immune Disord Drug Targets 2006;6:127-35. [Crossref] [PubMed]
- Shaashua L, Sominsky L, Levi B, et al. In vivo suppression of plasma IL-12 levels by acute and chronic stress paradigms: potential mediating mechanisms and sex differences. Brain Behav Immun 2012;26:996-1005. [Crossref] [PubMed]
- Deasy BM, Lu A, Tebbets JC, et al. A role for cell sex in stem cell-mediated skeletal muscle regeneration: female cells have higher muscle regeneration efficiency. J Cell Biol 2007;177:73-86. [Crossref] [PubMed]
- Rezvani Ghomi E, Khalili S, Nouri Khorasani S, et al. Wound dressings: Current advances and future directions. J Appl Polym Sci 2019;136:47738.


