
Current status of pre- and retropectoral breast reconstructions worldwide: a narrative review
Introduction
Advancements in breast cancer treatment and increased life expectancies have shifted the focus of care from survival alone towards a demand for increased quality of life and satisfying aesthetic results (1). Reconstruction is an integral part of breast cancer therapy and immediate reconstruction of the breast has become a standard of care, facilitated by conjoined efforts of technological and surgical innovation.
Consequently, the popularity of sub-pectoral placement of implants has declined in favor of a pre-pectoral placement and there seem to be more advantages than disadvantages to this choice.
Muscle sparing approach is clearly a simpler technical procedure and perhaps a first choice because later muscle support is still a backup plan, if necessary. The currently trending prepectoral plane is not new; in fact, it was the original plane for implant placement (2).
This is a narrative review that addresses milestones of the past leading up to current practice of prepectoral breast reconstruction (PBR) and subpectoral breast reconstruction (SBR) and potential future directions, in the scope of existing literature. We present this article in accordance with the Narrative Review reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-24-13/rc).
Materials and methods
A literature search in PubMed on 21 October 2023 using the search strings “prepectoral” or “subpectoral” and “breast reconstruction” generated 687 articles. Of these, English and Scandinavian language full-text articles with abstracts were systematically reviewed by the first author. Articles based on case reports or surgical methods were excluded, as were commentary articles. Articles from the reference lists and the authors’ own reference libraries, as well as the authors’ clinical experience, also form part of the evidence base.
Know and respect the past
The development of modern surgery was greatly influenced by advances in the industrial revolution up to the First World War. In 1889, independently, Johannes Esser from The Netherlands and Carl Manchot from France published, in their native language, the importance of vascular perforators and axial pattern of blood flow that became the foundation of flap surgery and eventually, nipple sparing mastectomy (NSM) (3).
The silicone breast implant, attributed to Cronin and Gerow in 1961, paved the way for the future of silicone breast implant reconstruction (4). The most logical placement for cosmetic augmentation of a breast was sub-glandular and for the first attempted breast reconstruction the implant was placed subdermal (2). Contour deformities and capsular contraction caused by thin mastectomy skin, as well as inferior quality implants, called for more protection with muscle, thicker envelope, and better implant technology.
In 1982, Radovan described tissue expansion and the concept was adapted to the armamentarium (5). The upper and medial pole of the implant supported by the pectoralis major muscle provided a necessary camouflage and improved the overall contour of the breast.
Total muscle coverage was considered a standard of care for implant-based breast reconstruction with tissue expanders until 2001 when Salzberg and Breuing independently began their innovative use of human acellular dermal matrix (ADM), to create a “pocket” for the implant and create a durable, dual plane defined space (6,7). At the same time prophylactic mastectomies were increasingly being considered for genetic predisposition for breast cancer (8,9). The dual plane “sling” solved the problem of a flat lower pole, and provided a pleasing breast contour that could be easily attained without additional effort with unmatched results in capable hands. The popularized two-stage breast reconstruction evolved into Salzberg’s “one and done” direct-to-implant (DIR) reconstruction, sparing the patient the burden of implant exchange (10,11).
ADM enabled DIR reconstruction on a global scale; however, its popularity exposed a problem, the breast animation deformity (BAD).
BAD
Animation of the pectoralis major muscle involvement in dual plane breast augmentations had been reported by Maxwell and Tornambe in 1988 and only sporadically mentioned until Spear et al. classified and minimized its aesthetic impact, two decades later in 2008 (12,13). Perhaps due to the minimal significance, at least in comparison to other challenges of breast implant reconstructions, BAD did not seem to be regarded as a problem in breast reconstruction according to the literature until Hammond et al. decided to publish a paper on how to fix this problem (14). Prophylactic mastectomies were increasingly being offered to younger patients with a genetic predisposition to develop breast cancer. New methods with unmatched results becoming a standard of care and more robust mastectomy flaps were provided. Reconstructions began to resemble that of an augmented breast. A transition from the sub-pectoral to a pre-pectoral pocket was furthermore enabled by the addition of autologous fat transfer or a secondary sheet of ADM if necessary.
When surgery to change the implant from a sub- to pre-pectoral plane became more frequent a full ADM coverage/hammock became a popular solution. Consequently, a booming demand for human cadaver ADM arose in the US and porcine ADM in Europe.
SBR
The authors of this review have individually reported on the safety and reliability of DIR reconstruction both in a dual plane, as well as a prepectoral hammock without the muscle with full and partial ADM coverage and shown comparative results with low complications for the need for excellent selection of proper patient (11,15,16).
Although the safety of NSM/DIR reconstruction with ADM has been established by large samples with long-erm results, multicentered European studies, designed to verify the safety of ADM, were unable to replicate the results showing much higher rates of reconstructive failure in comparison and concluded that two-stage reconstruction was safer than the “one-step” (11,15-19).
PBR
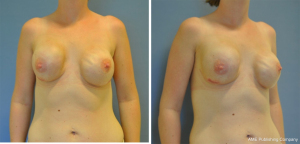
If sufficient soft tissue is left on the mastectomy skin flap the prepectoral plane is an apparent excellent choice for implant placement. The implant needs to be supported against the anterior chest wall to create a breast mound (Figure 1). Weight and size of the implant and varying quality of the supporting fibrous tissue affects the results of the reconstruction.

Heavy implants, lacking support, pull on the skin and often cause bottoming out with rippling of the superior pole (Figure 2). They can even cause pressure necrosis of the skin if they impair blood supply (Figure 3).
Early rippling and visible implant margin after prepectoral reconstruction occurs due to thin skin flap and poor support of the breast while late rippling occurs along with decreasing soft tissue support.
Soft tissue support of the implant is important to keep it in place. The main purpose of the ADM or synthetic mesh was to stabilize the implant at the level of the breast footprint, keeping it from moving laterally and inferiorly or compressing the vascularity of the mastectomy skin (20). Support is especially important for shaped implants as their displacement will cause unsightly asymmetry. A lack of upper pole support, provided by the pectoralis muscle or total ADM coverage, allows the implants to rotate or even “flip over”, bottom up, during events such as motion sports, and they are not easily “flipped back” without surgery (Figure 3).
When shaped implants started failing our expectations and anaplastic large cell lymphoma became evident, they were commonly exchanged for round smooth devices that consequently became a first choice in subsequent reconstructions when it was noticed that the results were no less attractive than the anatomical shape (Figures 1,3,4).

The present
As postulated, we have seen a rise in PBRs and publication in their favor (21). The PubMed index search revealed a single report in 2015 followed by 17 indexed publications in 2017 and over 200 to this date. Many recent reviews and meta-analyses that compare PBR and SBR conclude on the safety of both procedures with comparable complication profile (22-28). Evidently there is a clear difference in terms of animation and postoperative pain and increased patient satisfaction based on Breast Q results was deemed in favor of PBR. The overall complications, such as skin flap necrosis, infections, seroma, and hematoma appear to be similar for both PBR and SBR (22,23,26). This indicates that neither the reconstructive plane nor involvement of the muscle affects complications known to be related to the mastectomy procedure and quality of the skin flap provided, further establishing the importance of the mastectomy.
A reported lower rate of capsular contracture in the PBR group, although only in relatively short term unrandomized follow-up studies, might correlate to the increased use of biologics that has been found favorable at the same time as it contradicts the claim that a subpectoral placement reduces capsular contraction, and debunks that myth (22,26). There are known capsular formations despite the use of ADMs, and they occur, not surprisingly, more frequently after complications, like hematoma, infection, and seroma (29).
The validity of existing reports and studies praising the influence of biologics and implant surface technology in improved capsular contracture rates must be questioned while they are only based on weak evidence at best, small samples, short-term follow-ups and apparent conflicts of interest. We await long-term, multicentered, prospective trials to confirm such benefits. Combination of factors play a role and large volume, and long-term results are promising if they can be replicated (11).
Marks et al. surveyed the status on PBR and SBR among members of the American Society of Plastic Surgeons (ASPS), showing increased use of PBR with nearly 50% of its responders preferring the method all the time or nearly all the time (30). It further showed the technical preference of use of human ADM in 92.6% although they still prefer two stages in most instance (30.2% compared to 8.6% DIR reconstruction). We are not aware of any similar European study although preference varies according to the level of training and experience of the surgeon involved in the reconstruction.
The following are the leading factors of how to choose the placement plane:
- Mastectomy: first and foremost, the quality of the mastectomy flap. A reconstruction starts with the mastectomy. Anatomical aspects are clear, and dissection should create a definition between the anterior superficial fascia and parietal glandular fascia surrounding the corpus mammae, sparing the subdermal plexus and areolar fat to allow for a well-perfused skin flap, and consequently, prime a successful reconstruction.
- Radiation: radiation causes ischemia and scarring of the pectoralis major muscle. Fortunately, radiation therapy is becoming better adjusted due to uncertain survival benefits and harmful late effects; evidence largely supports that less is more (31). This will undoubtedly lead to lesser fractions of radiation and radiation related complications and better reconstructive options in the future. Radiation seems to cause a lesser problem in PBR due to lesser affection on the pectoralis major muscle. This might be an argument to use PBR when radiation is planned, although its oncological safety is still unclear in terms of potential micro-metastasis on top of the muscle. Pre-mastectomy radiation in prepectoral reconstruction comes at a significantly higher rate of seroma and implant loss compared to no radiation and postmastectomy radiation and should warrant special attention or be avoided (32,33).
- Surgical mesh and ADMs: the supporting internal bra fixes the implant at the footprint of the breast (20). While non-biologics offer only support of the implant, ADMs are held to create an additional biological barrier between the skin and implant that can protect the implant from direct exposure if the skin breaks down. Such a biologic capsule creates a potential space for autologous fat grafting. Fat grafting seems facilitated up against a firm ADM capsule and recent report suggests a mechanism how ADM or biologics might promote fat graft survival due to their fascia like impact that enables vascularization of the grafted fat (34).
- Pectoralis muscle: Dyrberg et al. were the first to show the reduced incidence of BAD in a comparative series of prepectoral vs. subpectoral NSM/DIR reconstruction (35). Later confirmed by prospective randomized controlled trial by the same group (36).
- Pain: immediate postoperative pain is significantly reduced without involvement of the pectoralis muscle, as shown by Caputo et al. and confirmed by Dyrberg et al. Pain is not an issue long term and there is no measurable difference after 3 months, although they did not evaluate the burden of expansion that is not a painless procedure (36,37).
- Autologous fat graft (AFG): adipocytes adhere to the same rules as transfer of any living tissue (38). To survive and do their intended job, quantities and quality need to be precisely established and placed to secure survival. Restoration of vascularity is a key, and the volume effect of expanding fat cells is largely secondary while the immediate effect of the procedure is due to release of scar tissue and contractions. Any skilled surgeon will understand that AFG is a welcome addition to our armamentarium while it comes with great limitations, especially long term and should be treated as any other remedy where less is, likely, more (39).
- Implant technology: surprisingly little has changed in implant technology over the years. US surgeons were set back, two decades, behind Europe in 1992 when Food and Drug Administration (FDA) decided to ban silicone implants. The ban was lifted 14 years later and has not reoccurred despite major scandals in European production. The FDA decision made European surgeons leading figures in the use of silicone breast implants. Sponsored by the industry, breast meetings of major European cities became a trending success.
- Patient intrinsic factors: our team reported the importance of intrinsic patient factors for successful ADM reconstruction in 2011 showing a 33% increased risk of reconstructive failure in smokers vs. 4% in non-smokers (15). We later emphasized how to pre-shape the large and ptotic breast prior to DIR reconstruction to avoid imminent reconstructive failure (40,41). The goal to keep complications under 4% has been successfully attained by adhering to careful selection of the patients in terms of intrinsic factors and topographic anatomy.
There is a significant chance of rippling, increasing over time, and this is also the case after prepectoral plane shifting for BAD, although there appears to be lesser chance for capsular contraction with poor connective tissue quality and larger for bottoming out. The tissue quality needs to be determined, and support, chosen accordingly. Heavy implants pull their weight, literally.
Safran et al. addressed the aesthetic limitations of the prepectoral plane and showed in a series of 334 breasts the occurrence of capsular contracture grade 3–4 in 8.1%, rippling 7.8% (major rippling 2.7% and minor 5.1%) and flipping and displacement 2.7% (1.2% and 1.5%) (42).
This indicates that there are still plenty of opportunities for corrective procedures and future innovations in this field.
Future perspectives
It is safe to say that we are in a “pre-pectoral era”, for the time being, and it is important to remember, when the pendulum swings back, the wise words of Sir Harold Gillies; “I never always do anything” and keep adjusting to the future.
Total muscle coverage has mostly fallen out of favor: expansion of the muscle can be a painful and often unnecessary procedure. It makes no sense to the authors of this paper to preserve the skin envelope and let it scar down, only to expand it again at a later stage then to include the underlying muscle in a reconstruction. When ADM became available it was used for secondary implant reconstructions as well, we found out that it was hardly ever necessary and better preserved for complicated cases and corrections. Critics who describe the ADM procedure as a wrong choice or “profit-driven push for a decades/old proven poor result, prone to early complications” have been proven both right and wrong, there are indications that ADM has been a game changer (30).
The pectoralis major muscle still has a place in the dual plane: King et al. recently published an algorithm, based on the senior authors experience and literature references, to guide on surgical plane selection for implant-based breast reconstruction (43). If patients have poor skin quality and are lacking subcutaneous fat, the implant might become visible, and one might choose a dual plane. Soft tissue support of the implant is also important to avoid displacement, bottoming out and “flipping” (17,20). The muscle offers additional protection and warmth to the implant that can become rather uncomfortably cold in colder climates and water when bathing. Upper pole support of the muscle should be considered in these situations.
Economics
Where diagnostic related groups determine hospital economics, management might be reluctant to see the benefits of one operation instead of two. “Why make it a single operation if you can bill for two?” The “one and done” procedure was therefore continued in two stages with an expander placement at many hospitals in the US while inspired European surgeons went directly to permanent silicone implant when possible and often with variable success furthering a continuing debate on almost every step of the procedure. This, one vs. two stages, confusion most likely contributed to a growing literature suggesting the increased safety of two-stage immediate reconstruction, disregarding selection criteria based on intrinsic factors and topographic anatomy as mentioned above. There are too many confounders and inconsistencies to make a clear assumption based on the existing studies and the meta-analysis echo that. Papers have emerged showing equally satisfactory results, at least short-term, using different biologic or non-biologic sheets and nets and even when they disagree on the importance of the net, they all emphasize the quality of the mastectomy skin flap and patients’ intrinsic factors (44).
Conflicting interests
Publications on the use of ADM have been found to be strongly affected by conflict of interest in papers published in British and American journals showing 92.7% of papers with first and or senior author being compensated, and they are more likely to report positive outcomes (45).
The medical supply industry tends to seek cooperation with profiled surgeons who show good results and promote those who use their brands. This is a major influence and bias at the same time. It is therefore important to remind aspiring surgeons with academic interest to avoid conflicts of interest that could discredit their chance to publish reliable scientific results.
The future role of ADM and biologics in breast reconstruction will continue to be questioned considering their high costs and strong research affiliation, driving surgeons to test alternative products and, rightfully, questioning existing literature. Innovation requires some form of academic disobedience and youthful rebellion is a healthy sign of evolution. After all it is what has brought us to where we are today.
Conclusions
When biologics replaced the muscle in breast reconstruction, they helped create a result far beyond expectations, allowing surgeons to reexplore the prepectoral plane and leave the muscle behind. Reappraising the importance of breast anatomy and preservation of flap vascularity. This is in brief, the evolution of the pre-/sub-pectoral debate. Unless the reader understands the many variables that make up a successful procedure, they will keep debating each of them based on gut instincts alone.
A synchronized team of breast surgeon and plastic surgeon who work well together to create not only a viable but also a robust mastectomy skin flap paves the path to a successful DIR reconstruction. Such a relationship seems imperative, above all, for success.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Tine Engberg Damsgaard, C. Andrew Salzberg and Jørn Bo Thomsen) for the series “Hot Topics in Breast Reconstruction Worldwide” published in Gland Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://gs.amegroups.org/article/view/10.21037/gs-24-13/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-24-13/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-24-13/coif). The series “Hot Topics in Breast Reconstruction Worldwide” was commissioned by the editorial office without any funding or sponsorship. C.A.S. served as the unpaid guest editor of the series and serves as an unpaid editorial board member of Gland Surgery from September 2022 to August 2024. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article and accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Blucher AS, Mills GB, Tsang YH. Precision oncology for breast cancer through clinical trials. Clin Exp Metastasis 2022;39:71-8. [Crossref] [PubMed]
- Snyderman RK, Guthrie RH. Reconstruction of the female breast following radical mastectomy. Plast Reconstr Surg 1971;47:565-7. [Crossref] [PubMed]
- Spear SL, Hannan CM, Willey SC, et al. Nipple-sparing mastectomy. Plast Reconstr Surg 2009;123:1665-73. [Crossref] [PubMed]
- Cronin TD, Gerow FJ. Augmentation mammaplasty: a new “natural feel” prosthesis. In: Transactions of the Third International Congress of Plastic and Reconstructive Surgery. Amsterdam: Excerpta Medica; 1963.
- Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg 1982;69:195-208. [Crossref] [PubMed]
- Salzberg CA. Nonexpansive immediate breast reconstruction using human acellular tissue matrix graft (AlloDerm). Ann Plast Surg 2006;57:1-5. [Crossref] [PubMed]
- Breuing KH, Warren SM. Immediate bilateral breast reconstruction with implants and inferolateral AlloDerm slings. Ann Plast Surg 2005;55:232-9. [Crossref] [PubMed]
- Spear SL, Carter ME, Schwarz K. Prophylactic mastectomy: indications, options, and reconstructive alternatives. Plast Reconstr Surg 2005;115:891-909. [Crossref] [PubMed]
- Ashikari RH, Ashikari AY, Kelemen PR, et al. Subcutaneous mastectomy and immediate reconstruction for prevention of breast cancer for high-risk patients. Breast Cancer 2008;15:185-91. [Crossref] [PubMed]
- Salzberg CA. Focus on technique: one-stage implant-based breast reconstruction. Plast Reconstr Surg 2012;130:95S-103S. [Crossref] [PubMed]
- Salzberg CA, Ashikari AY, Berry C, et al. Acellular Dermal Matrix-Assisted Direct-to-Implant Breast Reconstruction and Capsular Contracture: A 13-Year Experience. Plast Reconstr Surg 2016;138:329-37. [Crossref] [PubMed]
- Maxwell GP, Tornambe R. Management of mammary subpectoral implant distortion. Clin Plast Surg 1988;15:601-11. [Crossref] [PubMed]
- Spear SL, Schwartz J, Dayan JH, et al. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg 2009;33:44-8. [Crossref] [PubMed]
- Hammond DC, Schmitt WP, O'Connor EA. Treatment of breast animation deformity in implant-based reconstruction with pocket change to the subcutaneous position. Plast Reconstr Surg 2015;135:1540-4. [Crossref] [PubMed]
- Gunnarsson GL, Børsen-Koch M, Arffmann S, et al. Successful breast reconstruction using acellular dermal matrix can be recommended in healthy non-smoking patients. Dan Med J 2013;60:A4751. [PubMed]
- Heidemann LN, Gunnarsson GL, Salzberg CA, et al. Complications following Nipple-Sparing Mastectomy and Immediate Acellular Dermal Matrix Implant-based Breast Reconstruction-A Systematic Review and Meta-analysis. Plast Reconstr Surg Glob Open 2018;6:e1625. [Crossref] [PubMed]
- Colwell AS, Taylor EM. Recent Advances in Implant-Based Breast Reconstruction. Plast Reconstr Surg 2020;145:421e-432e. [Crossref] [PubMed]
- Dikmans RE, Negenborn VL, Bouman MB, et al. Two-stage implant-based breast reconstruction compared with immediate one-stage implant-based breast reconstruction augmented with an acellular dermal matrix: an open-label, phase 4, multicentre, randomised, controlled trial. Lancet Oncol 2017;18:251-8. [Crossref] [PubMed]
- Potter S, Conroy EJ, Cutress RI, et al. Short-term safety outcomes of mastectomy and immediate implant-based breast reconstruction with and without mesh (iBRA): a multicentre, prospective cohort study. Lancet Oncol 2019;20:254-66. [Crossref] [PubMed]
- Gunnarsson GL, Thomsen JB. Prepectoral Hammock and Direct-to-implant Breast Reconstruction in 10 Minutes: A Focus on Technique. Plast Reconstr Surg Glob Open 2018;6:e1931. [Crossref] [PubMed]
- Gunnarsson GL, Heidemann LN, Bille C, et al. Nipple sparing mastectomy and the evolving direct to implant breast reconstruction. Gland Surg 2018;7:267-72. [Crossref] [PubMed]
- Kim YH, Yang YJ, Lee DW, et al. Prevention of Postoperative Complications by Prepectoral versus Subpectoral Breast Reconstruction: A Systematic Review and Meta-Analysis. Plast Reconstr Surg 2024;153:10e-24e. [PubMed]
- Ching AH, Lim K, Sze PW, et al. Quality of life, pain of prepectoral and subpectoral implant-based breast reconstruction with a discussion on cost: A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg 2022;75:2550-60. [Crossref] [PubMed]
- Li L, Su Y, Xiu B, et al. Comparison of prepectoral and subpectoral breast reconstruction after mastectomies: A systematic review and meta analysis. Eur J Surg Oncol 2019;45:1542-50. [Crossref] [PubMed]
- Mégevand V, Scampa M, McEvoy H, et al. Comparison of Outcomes Following Prepectoral and Subpectoral Implants for Breast Reconstruction: Systematic Review and Meta-Analysis. Cancers (Basel) 2022;14:4223. [Crossref] [PubMed]
- Ostapenko E, Nixdorf L, Devyatko Y, et al. Prepectoral Versus Subpectoral Implant-Based Breast Reconstruction: A Systemic Review and Meta-analysis. Ann Surg Oncol 2023;30:126-36. [Crossref] [PubMed]
- Zhu L, Liu C. Postoperative Complications Following Prepectoral Versus Partial Subpectoral Implant-Based Breast Reconstruction Using ADM: A Systematic Review and Meta-analysis. Aesthetic Plast Surg 2023;47:1260-73. [Crossref] [PubMed]
- Liu J, Hou J, Li Z, et al. Efficacy of Acellular Dermal Matrix in Capsular Contracture of Implant-Based Breast Reconstruction: A Single-Arm Meta-analysis. Aesthetic Plast Surg 2020;44:735-42. [Crossref] [PubMed]
- Kearney AM, Yan Y, Bricker JT, et al. Acellular Dermal Matrix-Associated Contracture: A Clinical and Histologic Analysis of Patients Undergoing Prosthetic Breast Reconstruction. Plast Reconstr Surg 2021;148:968-77. [Crossref] [PubMed]
- Marks JM, Farmer RL, Afifi AM. Current Trends in Prepectoral Breast Reconstruction: A Survey of American Society of Plastic Surgeons Members. Plast Reconstr Surg Glob Open 2020;8:e3060. [Crossref] [PubMed]
- Brownlee Z, Garg R, Listo M, et al. Late complications of radiation therapy for breast cancer: evolution in techniques and risk over time. Gland Surg 2018;7:371-8. [Crossref] [PubMed]
- Sinnott CJ, Pronovost MT, Persing SM, et al. The Impact of Premastectomy Versus Postmastectomy Radiation Therapy on Outcomes in Prepectoral Implant-Based Breast Reconstruction. Ann Plast Surg 2021;87:S21-7. [Crossref] [PubMed]
- Awadeen A, Fareed M, Elameen AM. The Impact of Postmastectomy Radiation Therapy on the Outcomes of Prepectoral Implant-Based Breast Reconstruction: A Systematic Review and Meta-Analysis. Aesthetic Plast Surg 2023;47:81-91. [Crossref] [PubMed]
- Bi X, Li B, Zou J, et al. Fascia Promotes Adipose Tissue Regeneration by Improving Early Macrophage Infiltration after Fat Grafting in a Mouse Model. Plast Reconstr Surg 2023;152:446e-457e. [PubMed]
- Dyrberg DL, Gunnarsson GL, Bille C, et al. A simple clinical assessment of breast animation deformity following direct-to-implant breast reconstruction. Arch Plast Surg 2019;46:535-43. [Crossref] [PubMed]
- Dyrberg DL, Bille C, Koudahl V, et al. Evaluation of Breast Animation Deformity following Pre- and Subpectoral Direct-to-Implant Breast Reconstruction: A Randomized Controlled Trial. Arch Plast Surg 2022;49:587-95. [Crossref] [PubMed]
- Caputo GG, Zingaretti N, Kiprianidis I, et al. Quality of Life and Early Functional Evaluation in Direct-to-Implant Breast Reconstruction After Mastectomy: A Comparative Study Between Prepectoral Versus Dual-Plane Reconstruction. Clin Breast Cancer 2021;21:344-51. [Crossref] [PubMed]
- Kristensen RN, Gunnarsson GL, Børsen-Koch M, et al. Fast and simple fat grafting of the breast. Gland Surg 2015;4:572-6. [PubMed]
- Gunnarsson GL, Thomsen JB. MWL and Post Bariatric Surgery Patients: The Role of Fat Grafting and Regenerative Surgery. In: Kalaaji A. editor. Plastic and Aesthetic Regenerative Surgery and Fat Grafting. Springer, Cham; 2022:1407-24.
- Gunnarsson GL, Thomsen JB. Reply: How to Preshape the Breast for a Successful Nipple-Sparing Mastectomy and Direct-to-Implant Breast Reconstruction in the Challenging Breast. Plast Reconstr Surg 2018;141:610e-611e. [Crossref] [PubMed]
- Gunnarsson GL, Bille C, Reitsma LC, et al. Prophylactic Nipple-Sparing Mastectomy and Direct-to-Implant Reconstruction of the Large and Ptotic Breast: Is Preshaping of the Challenging Breast a Key to Success? Plast Reconstr Surg 2017;140:449-54. [Crossref] [PubMed]
- Safran T, Al-Badarin F, Al-Halabi B, et al. Aesthetic Limitations in Direct-to-Implant Prepectoral Breast Reconstruction. Plast Reconstr Surg 2022;150:22e-31e. [Crossref] [PubMed]
- King CA, Masanam MK, Tousimis EA, et al. Literature review and guide for optimal position in implant-based breast reconstruction. Gland Surg 2023;12:1082-93. [Crossref] [PubMed]
- Nolan IT, Farajzadeh MM, Boyd CJ, et al. Do we need acellular dermal matrix in prepectoral breast reconstruction? A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg 2023;86:251-60. [Crossref] [PubMed]
- Lee ZH, Diep GK, Brydges HT, et al. Do Corporate Payments Influence Research Related to the Use of Acellular Dermal Matrices in Breast Surgery? Plast Reconstr Surg 2023;152:376e-384e. [Crossref] [PubMed]



