
The prognostic value of lymph node dissection in patients with parathyroid carcinoma
Highlight box
Key findings
• Routine central lymph node dissection as part of initial surgery could not significantly improve cancer-specific survival (CSS) in parathyroid carcinoma (PC) patients.
What is known and what is new?
• Surgery is considered as the only potentially curative option for PC, and en bloc resection of parathyroid tumors with the ipsilateral thyroid, isthmus, and central lymph node compartment is suggested.
• The presence of large tumors and distant metastases were independent predictors of poor CSS in PC patients. Routine central lymph node dissection could not significantly improve CSS in PC patients, even for those with large tumors, lymph node metastasis, or distant disease.
What is the implication, and what should change now?
• Based on this study, the prognostic role of lymph node dissection has not been verified, further surgical treatment strategies for these patients should be modified.
Introduction
Parathyroid carcinoma (PC) is a relatively rare endocrine malignancy that affects a small percentage of patients with primary hyperparathyroidism (PHPT), ranging from 0.5% to 5% (1). Patients with PC often experience metabolic complications, including renal, bone, and cardiac diseases, which are caused by uncontrolled hypercalcemia. Unfortunately, diagnosing PC can be difficult, as there are no specific biomarkers or genetic signatures for this disease, making preoperative and intraoperative identification challenging. Additionally, PC shares similar clinical characteristics with parathyroid hyperplasia and adenoma, leading to potential misdiagnosis of PC as a benign lesion.
Surgery is considered as the only potentially curative option for PC, while the effect of chemotherapy and radiotherapy for this tumor is limited (2). According to previous studies and recommendations, en bloc resection of parathyroid tumors with the ipsilateral thyroid, isthmus, and central lymph node compartment is suggested, however, the optimal initial surgical extent is still a topic of debate (2,3). Particularly, the value of routine central lymph node dissection (LND) in patients with PC remains controversial owing to the paucity of clinical evidence. Some previous studies have discussed the prognostic value of LND for PC. Enomoto et al. and Lee et al. did not recommend LND for PC (4,5). In contrast, some other studies indicated lymph node status and LND were associated with survival (2,3,6-8). Given the conflicting roles of LND in survival, the infrequency of lymph node metastases in PC patients, and underlying complications related to LND, the effect of routine central LND for PC patients is still unclear (3,9).
Locoregional and distant recurrence are regarded as independent predictors of poor survival in PC patients, with survival worsening as the number of cervical recurrences increases (8,10). While a more extensive initial surgery, including central LND, theoretically could reduce recurrence and then improve survival, research outcomes have been inconsistent. Therefore, it is necessary to identify which groups of PC patients would benefit from central LND as a component of their initial surgery (11). To address this issue, a study was conducted using data from the Surveillance, Epidemiology and End Results (SEER)-18 registries to evaluate the effect of LND on cancer-specific survival (CSS) in PC patients who underwent surgery. In contrast to previous studies, the role of LND in CSS was also assessed in subgroups stratified by independent predictors of worse survival. We present this article in accordance with the STROBE reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-23-501/rc).
Methods
Data source and grouping
A study cohort analysis with data from Surveillance, Epidemiology, and End Results (SEER)-18 registries was retrospectively conducted. Permission to access the SEER Program from the National Cancer Institute, USA (NCI, USA) has been authorized. Informed consent and Institutional Review Board approval were waived because of the SEER’s use of unidentifiable patient information. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). PC patients were identified by the International Classification of Diseases for Oncology, Third Edition Codes (ICD-O-3): C75.0 and site code 59 from the SEER-18 database between 2004 and 2018. Patients included in the study had received surgical procedures, with diagnostic confirmation of positive histology, being actively followed up, and with a reporting source other than autopsy only/death certificate only. This extracted cohort (cohort 1) was used to describe the characteristics of PC patients. To explore the role of LND in CSS for PC patients, patients in cohort 1 without LND information, without tumor size, with less than 1 month of follow-up, with unknown death causes, and with missing information were excluded to create a filtered cohort (cohort 2) that was divided into two groups based on whether LND was performed or not. And then prognostic predictors associated with CSS were screened in cohort 2. Finally, the effect of LND on CSS was evaluated in subgroups stratified by prognostic predictors of CSS. The brief study flow chart is shown in Figure S1.
Variables and definitions
The demographic variable (age, sex, race, and year of diagnosis), clinicopathological data (tumor size, tumor grade, tumor stage, treatment strategies, and lymph node status), and survival data (survival status and survival time) were extracted from the SEER database. The tumor size was determined by “Collaborative Stage (CS) tumor size [2004–2015]” and “Tumor Size Summary (2016+)”. Tumor grade was only available for cases after 2017 and was recorded as grade I (well differentiated), II (moderately differentiated), III (poorly differentiated), and IV (undifferentiated). Tumor stage was based on “Combined Summary Stage (2004+)”, which was recorded as localized (lesions confined entirely to the parathyroid gland), regional (lesions infiltrating the thyroid, recurrent laryngeal nerve, trachea, esophagus, and surrounding tissues and organs without distant metastasis), distant (metastasis to other organs or distant lymph node), and unknown/unstaged (data not available). The surgical approach was defined following the Surgery Codes All Other Sites (https://seer.cancer.gov/archive/manuals/2018/AppendixC/Surgery_Codes_Other_Sites_2018.pdf). Code 60 represented radical surgery, which was defined as the resection of the primary parathyroid lesions, ipsilateral thyroid, and central neck dissection. Code 20 (local tumor resection), 30 (simple/partial tumor resection), 40 (total surgical removal of primary site), 50 (debulking), and 90 (surgery, NOS) were defined as others. Due to inconsistent view regarding LND as an initial surgical component, the decision on whether to perform LND or not may follow the discretion of the surgeons and the patients, the preoperative comprehensive assessments, or even the intraoperative findings. Lymph node status was categorized into positive, negative, and unknown following regional nodes positive (1988+). Survival status (alive or dead) was determined according to Vital Status Recode. CSS time was defined as the time from diagnosis to death attributed to PC or its distant metastasis. In this study, CSS was chosen as the primary endpoint instead of overall survival (OS) because PC is known to be a slow-growing cancer, and using OS as the primary endpoint may be influenced by factors such as the patient’s lifespan and current health conditions. By focusing on CSS, we can better evaluate the effectiveness of treatments independent of these confounding factors.
The continuous variables of age and tumor size were converted to binary variables based on the optimal cutoff values associated with CSS, which were calculated by the X-tile software (available at: https://medicine.yale.edu/lab/rimm/research/software/). The year of diagnosis was converted into three sets (2004–2008, 2009–2013, and 2014–2018).
Statistical analyses
Data were expressed as the mean ± standard deviation or the median with range for quantitative data, and as number plus percentage for categorical variables. Parameters of patients with LND and without LND were compared using Chi-square test, Fisher exact test, Mann-Whitney U test, and log-rank test. Univariate and multivariate Cox proportional hazards regression models were used to identify independent risk factors associated with CSS. Given the potential differences of patient baseline characteristics and the selection bias of LND treatment in the retrospective analysis of its role in prognosis, a propensity score matching (PSM) cohort was generated by R software studio (R version 4. 2. 2) using 1:1–1:2 nearest-neighbor algorithm with a caliper width of 0.2 to control for confounding variables. The covariates used for the PSM included age, sex, race, year of diagnosis, tumor size, tumor grade, tumor stage, primary surgical types, and radiotherapy. After the PSM process, we compared the variables between the two matched groups to ensure that the matching procedure achieved balance in the distribution of the selected covariates. Nevertheless, there might still be residual confounding due to unmatched variables after the PSM procedure. To address the concern of residual confounding, the variables and survival data of LND-treated patients who were included in the PSM cohort and those who were not included were also compared. All statistical analyses were performed using SPSS 26.0 for Windows (SPSS), and the rejection level for the null hypothesis was set at P value <0.05.
Results
Patients’ baseline characteristics
As is illustrated in Figure S1, a total of 338 patients clearly diagnosed with PC were enrolled as cohort 1 following the inclusion and exclusion criteria. The mean age was 57.3 years old (166 women and 172 men). Caucasian (71.0%) were the predominant race followed by African American (20.7%) and others/unknown (8.3%). A balanced prevalence (about 30%) was observed in the PC patients among the three 5-year intervals. Tumor size was available in 233 patients, and it ranged from 1.0 to 100.0 mm, with a median of 28.0 mm. The 5- and 10-year CSS were 94.4% and 89.7% respectively. The other treatment and survival information is summarized in Table 1.
Table 1
| Variables | Values (n=338) |
|---|---|
| Age (years) | 57.3±14.7 |
| Sex | |
| Female | 166 (49.1) |
| Male | 172 (50.9) |
| Race | |
| White | 240 (71.0) |
| African American | 70 (20.7) |
| Others/unknown | 28 (8.3) |
| Year of diagnosis | |
| 2004–2008 | 116 (34.3) |
| 2009–2013 | 116 (34.3) |
| 2014–2018 | 106 (31.4) |
| Tumor size (mm) (n=233) | 28.0 (1.0–100.0) |
| Grade | |
| Grade I | 29 (8.6) |
| Grade II | 7 (2.1) |
| Grade III | 2 (0.6) |
| Grade IV | 1 (0.3) |
| Unknown/blank | 299 (88.5) |
| Stage | |
| Localized | 211 (62.4) |
| Regional | 102 (30.2) |
| Distant | 15 (4.4) |
| Unknown | 10 (3.0) |
| Primary surgery | |
| Radical surgery | 136 (40.2) |
| Others | 202 (59.8) |
| Lymph node dissection | |
| Yes | 105 (31.1) |
| No | 213 (63.0) |
| Others | 20 (5.9) |
| Lymph node status | |
| Positive | 12 (3.6) |
| Negative | 93 (27.5) |
| Unknown | 233 (68.9) |
| Radiotherapy | |
| Yes | 40 (11.8) |
| Others | 298 (88.2) |
| Follow-up time (months) | 64.0 (0–179.0) |
| Survival status | |
| Alive | 259 (76.6) |
| Dead from PC | 23 (6.8) |
| Dead from other causes | 56 (16.6) |
| CSS, % | |
| 5-year survival | 94.4 |
| 10-year survival | 89.7 |
Data are expressed as mean ± standard deviation, number (percentage), or median (range). PC, parathyroid carcinoma; CSS, cancer-specific survival.
Comparisons of patients with LND and without LND and prognostic predictors of CSS
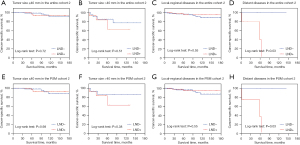
As summarized in Table 2, a total of 215 patients clearly diagnosed with PC (cohort 2) were selected to evaluate the impact of LND on the prognosis of PC. The X-tile program identified two optimal age sets (≤66 and >66 years old) and two tumor size sets (≤40 and >40 mm), as shown in Figure S2A-S2D. Of the 215 patients, 69 received LND, while the remaining 146 did not. Except the radiotherapy, there were no significant differences in terms of age, sex, race, year of diagnosis, tumor size, grade, stage, primary surgery between the LND and non-LND groups. Eight (5.5%) in the non-LND group and 5 (7.2%) patients in the LND group died from PC. The survival time [75.5 (1.0–179.0) vs. 60.0 (2.0–177.0) months, P=0.11], 5-year CSS, and 10-year CSS (96.8%/89.7% vs. 91.4%/88.4%, P=0.43) were comparable between these two groups, and no significant differences were identified in terms of CSS curves between the groups (Figure 1A). Moreover, survival analyses also indicated no significant differences in survival status, survival time and CSS between non-LND and LND groups in the PSM cohort, and the CSS curves also displayed no significant differences between these two groups (Figure 1B). Additionally, to mitigate the potential impact of residual confounding arising from unmatched variables after the PSM procedure, the characteristics and survival data of LND-treated patients included in and excluded from the PSM cohort were compared, and the results showed they were comparable (Table S1 and Figure S3). Overall, these results indicated that LND could hardly improve CSS in patients with PC.
Table 2
| Variables | The entire cohort 2 | The PSM cohort 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All (n=215) | LND – (n=146) | LND + (n=69) | P value | All (n=167) | LND – (n=104) | LND + (n=63) | P value | ||
| Age (years) | 0.56 | 0.89 | |||||||
| ≤66 | 163 (75.8) | 109 (74.7) | 54 (78.3) | 125 (74.9) | 77 (74.0) | 48 (76.2) | |||
| >66 | 52 (24.2) | 37 (25.3) | 15 (21.7) | 42 (25.1) | 27 (26.0) | 15 (23.8) | |||
| Sex | 0.62 | >0.99 | |||||||
| Female | 105 (48.8) | 73 (50.0) | 32 (46.4) | 77 (46.1) | 48 (46.2) | 29 (46.0) | |||
| Male | 110 (51.2) | 73 (50.0) | 37 (53.6) | 90 (53.9) | 56 (53.8) | 34 (54.0) | |||
| Race | 0.24 | 0.98 | |||||||
| White | 156 (72.6) | 101 (69.2) | 55 (79.7) | 129 (77.2) | 80 (76.9) | 49 (77.8) | |||
| African American | 37 (17.2) | 29 (19.9) | 8 (11.6) | 22 (13.2) | 14 (13.5) | 8 (12.7) | |||
| Others | 22 (10.2) | 16 (11.0) | 6 (8.7) | 16 (9.6) | 10 (9.6) | 6 (9.5) | |||
| Year of diagnosis | 0.17 | 0.89 | |||||||
| 2004–2008 | 74 (34.4) | 55 (37.7) | 19 (27.5) | 51 (30.5) | 32 (30.8) | 19 (30.2) | |||
| 2009–2013 | 74 (34.4) | 51 (34.9) | 23 (33.3) | 56 (33.5) | 36 (34.6) | 20 (31.7) | |||
| 2014–2018 | 67 (31.2) | 40 (27.4) | 27 (39.1) | 60 (35.9) | 36 (34.6) | 24 (38.1) | |||
| Tumor size (mm) | 0.28 | 0.36 | |||||||
| ≤40 | 177 (82.3) | 123 (84.2) | 54 (78.3) | 137 (82.0) | 88 (84.6) | 49 (77.8) | |||
| >40 | 38 (17.7) | 23 (15.8) | 15 (21.7) | 30 (18.0) | 16 (15.4) | 14 (22.2) | |||
| Grade | 0.10 | 0.87 | |||||||
| Grade I | 19 (8.8) | 15 (10.3) | 4 (5.8) | 11 (6.6) | 7 (6.7) | 4 (6.3) | |||
| Grade II–IV | 8 (3.7) | 3 (2.1) | 5 (7.2) | 4 (2.4) | 2 (1.9) | 2 (3.2) | |||
| Unknown/blank | 188 (87.4) | 128 (87.7) | 60 (87.0) | 152 (91.0) | 95 (91.3) | 57 (90.5) | |||
| Stage | 0.39 | 0.75 | |||||||
| Localized | 140 (65.1) | 98 (67.1) | 42 (60.9) | 106 (63.5) | 67 (64.4) | 39 (61.9) | |||
| Regional | 65 (30.2) | 43 (29.5) | 22 (31.9) | 53 (31.7) | 33 (31.7) | 20 (31.7) | |||
| Distant | 10 (4.7) | 5 (3.4) | 5 (7.2) | 8 (4.8) | 4 (3.8) | 4 (6.3) | |||
| Primary surgery | 0.85 | 0.99 | |||||||
| Radical surgery | 86 (40.0) | 59 (40.4) | 27 (39.1) | 65 (38.9) | 41 (39.4) | 24 (38.1) | |||
| Others | 129 (60.0) | 87 (59.6) | 42 (60.9) | 102 (61.1) | 63 (60.6) | 39 (61.9) | |||
| Lymph node status | – | – | |||||||
| Positive | – | – | 6 (8.7) | – | – | 6 (9.5) | |||
| Negative | – | – | 56 (81.2) | – | – | 50 (79.4) | |||
| Unknown | – | – | 7 (10.1) | – | – | 7 (11.1) | |||
| Radiotherapy | 0.04 | 0.45 | |||||||
| Yes | 31 (14.4) | 16 (11.0) | 15 (21.7) | 26 (15.6) | 14 (13.5) | 12 (19.0) | |||
| Others | 184 (85.6) | 130 (89.0) | 54 (78.3) | 141 (84.4) | 90 (86.5) | 51 (81.0) | |||
| Survival status | 0.87 | 0.34 | |||||||
| Alive | 177 (82.3) | 121 (82.9) | 56 (81.2) | 141 (84.4) | 91 (87.5) | 50 (79.4) | |||
| Dead from PC | 13 (6.0) | 8 (5.5) | 5 (7.2) | 11 (6.6) | 6 (5.8) | 5 (7.9) | |||
| Dead from other causes | 25 (11.6) | 17 (11.6) | 8 (11.6) | 15 (9.0) | 7 (6.7) | 8 (12.7) | |||
| Survival time (months) | 65.0 (1.0–179.0) |
75.5 (1.0–179.0) |
60.0 (2.0–177.0) |
0.11 | 63.0 (2.0–178.0) |
65.5 (1.0–178.0) |
60.0 (2.0–177.0) |
0.25 | |
| CSS (log-rank test), % | 0.43 | 0.45 | |||||||
| 5-year survival | 95.2 | 96.8 | 91.4 | 96.5 | 96.5 | 90.6 | |||
| 10-year survival | 89.0 | 89.7 | 88.4 | 89.7 | 87.8 | 87.4 | |||
Data are expressed as number (percentage) or median (range). LND, lymph node dissection; PSM, propensity score matching; PC, parathyroid carcinoma; CSS, cancer-specific survival.

Since LND was not associated with improved CSS, we next explored the predictors of CSS in the entire cohort 2 and the PSM cohort 2. As shown in Table 3, univariate and multivariate Cox proportional hazards regression analyses indicated that tumor size larger than 40 mm, and distant metastasis were significantly associated with poor CSS both in the entire cohort 2 (tumor size >40 mm, HR =5.703, 95% CI: 1.824–17.826, P=0.003; distant metastasis, HR =7.304, 95% CI: 1. 672–31.903, P=0.008) and the PSM cohort 2 (tumor size >40 mm, HR =3.901, 95% CI: 1.141–13.341, P=0.03; distant metastasis, HR =9.322, 95% CI: 2.041–42.569, P=0.004).
Table 3
| Variables | The entire cohort 2 | The PSM cohort 2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate Cox regression analyses | Multivariate Cox regression analyses | Univariate Cox regression analyses | Multivariate Cox regression analyses | ||||||||
| HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | HR (95% CI) | P value | ||||
| Age (years) | 0.08 | 0.15 | |||||||||
| ≤66 | Reference | Reference | |||||||||
| >66 | 2.649 (0.861–8.146) | 2.458 (0.714–8.466) | |||||||||
| Sex | 0.76 | 0.51 | |||||||||
| Female | Reference | Reference | |||||||||
| Male | 0.848 (0.285–2.523) | 0.672 (0.205–2.205) | |||||||||
| Race | 0.15 | 0.39 | |||||||||
| White | Reference | Reference | |||||||||
| African American | 0.975 (0.207–4.600) | 0.97 | 1.490 (0.308–7.196) | 0.62 | |||||||
| Others | 3.588 (0.947–13.594) | 0.06 | 2.938 (0.607–14.206) | 0.18 | |||||||
| Year of diagnosis | 0.83 | 0.81 | |||||||||
| 2004–2008 | Reference | Reference | |||||||||
| 2009–2013 | 0.799 (0.223–2.859) | 0.73 | 1.109 (0.277–4.436) | 0.88 | |||||||
| 2014–2018 | 1.376 (0.227–8.362) | 0.72 | 1.881 (0.265–13.361) | 0.52 | |||||||
| Tumor size (mm) | 0.001 | 0.003 | 0.01 | 0.03 | |||||||
| ≤40 | Reference | Reference | Reference | Reference | |||||||
| >40 | 6.854 (2.296–20.462) | 5.703 (1.824–17.826) | 4.516 (1.376–14.825) | 3.901 (1.141–13.341) | |||||||
| Stage | 0.003 | 0.03 | 0.004 | 0.02 | |||||||
| Local | Reference | Reference | Reference | Reference | |||||||
| Regional | 2.344 (0.677–8.107) | 0.17 | 2.475 (0.705–8.682) | 0.15 | 2.130 (0.532–8.522) | 0.28 | 2.364 (0.584–9.571) | 0.22 | |||
| Distant | 12.300 (2.896–52.244) | 0.001 | 7.304 (1.672–31.903) | 0.008 | 12.185(2.701 –54.970) | 0.001 | 9.322 (2.041 –42.569) | 0.004 | |||
| Primary surgery | 0.98 | 0.91 | |||||||||
| Radical surgery | Reference | Reference | |||||||||
| Others | 0.988 (0.323–3.022) | 1.067 (0.312–3.647) | |||||||||
| Radiotherapy | 0.10 | 0.07 | |||||||||
| Yes | Reference | Reference | |||||||||
| Others | 2.675 (0.823–8.691) | 3.012 (0.881–10.299) | |||||||||
| Lymph node dissection | 0.43 | 0.46 | |||||||||
| Yes | Reference | Reference | |||||||||
| No | 0.640 (0.209–1.962) | 0.640 (0.195–2.103) | |||||||||
CSS, cancer-specific survival; PSM, propensity score matching; HR, hazard ratio; CI, confidence interval.
Prognostic role of LND in subgroup analyses
Now that large tumor size and distant metastasis are independent predictors of poor CSS in PC patients, we wondered whether patients with these aggressive features would benefit from LND. Therefore, the effect of LND on CSS was further assessed in subgroups stratified by tumor size and tumor stage in the entire cohort 2 and the PSM cohort 2 (Table 4 and Figure 2A-2H). The results showed that CSS was not significantly improved in PC patients stratified by tumor size (>40 mm) both in the entire cohort 2 (HR =1.704, 95% CI: 0.339–8.573, P=0.51) and in the PSM cohort 2 (HR =2.201, 95% CI: 0.366–13.220, P=0.38). Unexpectedly, LND appeared to increase the mortality risk in PC patients with distant metastasis (HR =11.950, 95% CI: 1.717–121.900, P=0.03 both in the entire cohort 2 and the PSM cohort 2).
Table 4
| Stratified variables | The entire cohort 2 | The PSM cohort 2 | |||
|---|---|---|---|---|---|
| HR (95% CI) for LND | P value | HR (95% CI) for LND | P value | ||
| Tumor size | |||||
| ≤40 mm | 1.387 (0.228–8.454) | 0.72 | 0.978 (0.180–5.323) | 0.98 | |
| >40 mm | 1.704 (0.339–8.573) | 0.51 | 2.201 (0.366–13.220) | 0.38 | |
| Stage | |||||
| Local-regional | 0.660 (0.166–2.616) | 0.55 | 0.648 (0.151–2.780) | 0.55 | |
| Distant | 11.950 (1.717–121.900) | 0.03 | 11.950 (1.717–121.900) | 0.03 | |
LND, lymph node dissection; PSM, propensity score matching; HR, hazard ratio; CI, confidence interval.
Finally, to explain the role of LND in patients without lymph node metastasis, we compared the CSS between patients with postoperatively confirmed positive LN and patients with postoperatively confirmed negative LN in subgroups. And The findings indicated that regardless of the lymph node status, LND did not confer any improvement in CSS (Figure S4).
Discussion
Due to the rare incidence of PC, there are some critical issues that have not been well addressed, such as preoperative diagnosis, optimal operative approach, and follow-up strategies of this disease. The current recommended operative procedure for PC patients involves an en bloc resection of the parathyroid lesions with ipsilateral thyroid lobe, isthmus, and the ipsilateral central lymph node compartment, however, the significance regarding the cervical LND during the initial PC surgery is still in dispute. The reported lymph node metastasis rate ranged from 0% to 42.8% (4,5). While some previous studies found that positive lymph nodes were associated with worse survival, others did not confirm this finding (8,12). Furthermore, the American Association of Endocrine Surgeon guidelines does not recommend routine LND for PC patients, but the supporting evidence for this recommendation is limited and insufficient (13). Given the inconclusive role of LND in survival prognosis and the potential morbidities, such as recurrent laryngeal nerve palsy and permanent hypoparathyroidism from LND, a dilemma for PC patients is the necessity of performing LND during the initial surgery.
In the present study, we performed a population-based study using the SEER 18 database to explore the prognostic role of LND in PC patients. The results showed that the 5- and 10-year CSS was 94.4% and 89.7% respectively, which is in line with outcomes from previous studies and confirms that PC is generally indolent. However, local relapse involving regional lymph nodes or initial surgical site is not uncommon after surgery, ranging from 33% to 63% (10). Furthermore, locoregional recurrence is one of independent predictors of poor survival. Thus, some authors indicated lymph node metastasis was associated with poor survival and LND should be considered during the initial surgical procedures because it was reported to prolong disease-free survival (7,8,14,15). Conversely, some studies based on SEER database failed to verify the relationship between lymph node status or LND and prognosis of patients with PC (4,16). Someone may argue that the absence of complete data about lymph node status in a large number of cases from the SEER registry confounded the results. In order to overcome this bias, we did not focus on lymph node status of PC patients in this study, but in another sense, we regarded LND as a grouping factor. Even so, our result found no associations between LND and long-term survival. Therefore, further studies are warranted to explore the implications and appropriate application of LND in patients with PC.
On the other hand, some authors indicated that more advanced disease (such as large tumor size, high-risk Schulte staging, and CDC73 abnormalities) represented a greater incidence of lymph node metastasis in PC patients, which was a risk factor of disease recurrence after surgery and thus worsened survival (9,17). So, we furtherly wonder whether there is a subset of PC patients (e.g., patients with advanced disease) who may benefit from the prognostic value of a central LND as a component of their initial surgery. To address this issue, we firstly explored the prognostic factors associated with survival in PC patients. Univariate and multivariate analyses confirmed that large tumor size and distant disease were independent risk factors of poor survival in PC patients. Previous studies also supported our results. Zhang K, Ullah A, Tao M, Sun XM and some other authors concluded large tumor size affected the prognosis of PC (18-21). Nevertheless, the cutoff values of tumor size to predict mortality risk varied among studies, which can be attributable to different definitions of cutoff values and different sample sizes of studies. In the current study, using X-tile program, tumor size over 40 mm was identified as the optimal cutoff predicting survival. Expectedly, distant spread has been uniformly considered a key factor affecting the prognosis of PC (16,17,20,22). In this study, the involvement of distant organs and lymph nodes in PC patients carried a 7.3–9.3 times risk of death compared with local disease. Other prognostic factors reported in prior studies such as older age, Caucasian race, male sex, and marital status were not confirmed in this study (19,20). Coincidentally, both tumor size and disease progression were included in the mainstream staging system for PC patients proposed by Shaha and Shah (23). Therefore, we secondly evaluated whether patients with advanced disease could benefit more from LND during the initial surgery in terms of long-term survival. Unexpectedly, subgroup analyses stratified by tumor size indicated that LND had no effect on long-term survival. Although no benefit of LND was identified in the subgroup with large tumor size, the case number of the subgroup may be too small to produce meaningful statistical results. Additionally, LND can even increase mortality risk in patients with distant disease. We speculated that this finding may be due to the situation that distant disease of PC promoted the surgeon to perform more radical surgery (such as LND), which tended to worsen the already poor survival of these patients. Finally, we evaluated the role of LND in patients with postoperatively confirmed positive LN versus those with negative LN. And the results showed that no matter what the lymph node status was, LND failed to improve the CSS, thereby further reinforcing our conclusion.
Generally, the survival of PC is relatively good, surgical treatment is often focused on persistent disease and recurrence risk, and long-term survival is mainly dependent on hyperparathyroidism-related complications instead of tumor burden. Therefore, the results based on this study should be interpreted prudently. Although no benefits can be detected in this study, LND during initial surgery might slow down disease progression, reduce recurrence, relieve symptoms, and then improve survival. Thus, LND should be considered in PC patients, weighing the pros and cons of LND-related complications and its prognostic value.
Some strengths of this study should be highlighted. The optimal tumor size cutoff values were determined by the X-tile program rather than predefined method. PSM was used to balance baseline characteristics, which can reduce the influence of confounding factors and selection bias. LND-treated patients included in and excluded from the PSM cohort were compared, and found to be comparable, which further strengthens the credibility of our conclusions. The role of LND in the long-term survival was evaluated in subgroups stratified by prognostic factors. However, a few inevitable limitations based on SEER database should also be acknowledged. This study relies on SEER database for an extended period [2004–2018], and PC diagnostic criteria have changed over time, which might confound the diagnostic results. However, we think it can be accepted that if the cases met the diagnostic criteria at the time. Some important variables that might influence the prognosis of PC were not recorded, such as parathyroid hormone (PTH) and calcium levels, gene expression profiles, and recurrence data. Diagnostic coding errors may be present, because the SEER database lacks a centralized review of pathological data by experienced pathologists. And preoperative diagnosis of PC can be challenging due to its nonspecific biomarkers or genetic signature. However, it should be emphasized that one of the inclusion criteria of PC patients in this study is patients with diagnostic confirmation of positive histology. Therefore, this kind of study can be regarded as a post hoc analysis research. Furthermore, this study is not a diagnostic study, and we only need to include patients who are finally identified as parathyroid cancer for survival analysis, so post hoc analysis is not a bad alternative research strategy in this study. Codes for surgical types were not specific neither. Incomplete data such as lymph node status, tumor grade and tumor stage decreased the number of patients for analysis. Another concern is unclear how many PCs underwent a completion surgery after a postoperative diagnosis. The issue cannot be well addressed at present based on SEER database, because this information was not recorded. To avoid this bias to some extent, we used postoperative positive histology as the inclusion criterion. So, patients were also classified as LND group even if they had a positive postoperative diagnosis and then underwent a completion surgery and LND. Furthermore, although PSM was performed to minimize bias, it is essential to acknowledge that the results of this study might still be influenced by unknown potential systemic treatments received by patients, such as chemotherapy, radiotherapy, and calcimimetic agents. It is important to highlight that this study exclusively enrolled patients who underwent surgery as it is the primary mode of therapy for the condition under investigation. Chemotherapy and radiotherapy are generally ineffective in the treatment of PC patients, and calcimimetic agents are usually allowed to manage patients who are unsuitable for surgical treatment (2,24). Consequently, given the study’s focus on surgical patients and the limited scope of available systemic treatments for this specific condition, it is not feasible to assess the impact of potential systemic treatments on the prognosis of PC patients within the scope of this study. This aspect remains an important topic for further investigation and should be addressed in future studies with a broader patient population and different treatment modalities. Despite these limitations, given the rare incidence of this carcinoma, SEER database still compiles a larger number of PC patients for a robust statistical analysis than studies from any single institution.
Conclusions
To sum up, this study showed that PC patients had a relatively favorable CSS. LND did not improve CSS, even in patients with aggressive tumor characteristics such as large tumor size, advanced tumor stage and lymph node metastasis. Given the limitations of SEER database, further large-scale prospective studies are warranted to confirm the effect of LND on the prognosis of PC patients.
Acknowledgments
Funding: This study was funded by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-23-501/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-501/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-23-501/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent and Institutional Review Board approval were waived because of the SEER’s use of unidentifiable patient information. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rodrigo JP, Hernandez-Prera JC, Randolph GW, et al. Parathyroid cancer: An update. Cancer Treat Rev 2020;86:102012. [Crossref] [PubMed]
- Wei CH, Harari A. Parathyroid carcinoma: update and guidelines for management. Curr Treat Options Oncol 2012;13:11-23. [Crossref] [PubMed]
- Schulte KM, Talat N, Miell J, et al. Lymph node involvement and surgical approach in parathyroid cancer. World J Surg 2010;34:2611-20. [Crossref] [PubMed]
- Lee PK, Jarosek SL, Virnig BA, et al. Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer 2007;109:1736-41. [Crossref] [PubMed]
- Enomoto K, Uchino S, Ito A, et al. The surgical strategy and the molecular analysis of patients with parathyroid cancer. World J Surg 2010;34:2604-10. [Crossref] [PubMed]
- Sadler C, Gow KW, Beierle EA, et al. Parathyroid carcinoma in more than 1,000 patients: A population-level analysis. Surgery 2014;156:1622-9; discussion 1629-30. [Crossref] [PubMed]
- Schaapveld M, Jorna FH, Aben KK, et al. Incidence and prognosis of parathyroid gland carcinoma: a population-based study in The Netherlands estimating the preoperative diagnosis. Am J Surg 2011;202:590-7. [Crossref] [PubMed]
- Harari A, Waring A, Fernandez-Ranvier G, et al. Parathyroid carcinoma: a 43-year outcome and survival analysis. J Clin Endocrinol Metab 2011;96:3679-86. [Crossref] [PubMed]
- Hsu KT, Sippel RS, Chen H, et al. Is central lymph node dissection necessary for parathyroid carcinoma? Surgery 2014;156:1336-41; discussion 1341. [Crossref] [PubMed]
- Villar-del-Moral J, Jiménez-García A, Salvador-Egea P, et al. Prognostic factors and staging systems in parathyroid cancer: a multicenter cohort study. Surgery 2014;156:1132-44. [Crossref] [PubMed]
- Randle RW, Schneider DF, Lymph node dissection versus no lymph node dissection for parathyroid cancer. In: Angelos P, Grogan RH. editors. Difficult Decisions in Endocrine Surgery. Switzerland: Springer; 2018:193-208.
- Lenschow C, Schrägle S, Kircher S, et al. Clinical Presentation, Treatment, and Outcome of Parathyroid Carcinoma: Results of the NEKAR Retrospective International Multicenter Study. Ann Surg 2022;275:e479-87. [Crossref] [PubMed]
- Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg 2016;151:959-68. [Crossref] [PubMed]
- Koea JB, Shaw JH. Parathyroid cancer: biology and management. Surg Oncol 1999;8:155-65. [Crossref] [PubMed]
- Iihara M, Okamoto T, Suzuki R, et al. Functional parathyroid carcinoma: Long-term treatment outcome and risk factor analysis. Surgery 2007;142:936-43; discussion 943.e1. [Crossref] [PubMed]
- Qian B, Qian Y, Hu L, et al. Prognostic Analysis for Patients With Parathyroid Carcinoma: A Population-Based Study. Front Neurosci 2022;16:784599. [Crossref] [PubMed]
- Hu Y, Cui M, Chang X, et al. Patterns and Predictors of Cervical Lymph Node Metastasis in Parathyroid Carcinoma. Cancers (Basel) 2022;14:4004. [Crossref] [PubMed]
- Zhang K, Su A, Wang X, et al. Non-Linear Correlation Between Tumor Size and Survival Outcomes for Parathyroid Carcinoma: A SEER Population-Based Cohort Study. Front Endocrinol (Lausanne) 2022;13:882579. [Crossref] [PubMed]
- Ullah A, Khan J, Waheed A, et al. Parathyroid Carcinoma: Incidence, Survival Analysis, and Management: A Study from the SEER Database and Insights into Future Therapeutic Perspectives. Cancers (Basel) 2022;14:1426. [Crossref] [PubMed]
- Tao M, Luo S, Wang X, et al. A Nomogram Predicting the Overall Survival and Cancer-Specific Survival in Patients with Parathyroid Cancer: A Retrospective Study. Front Endocrinol (Lausanne) 2022;13:850457. [Crossref] [PubMed]
- Sun XM, Pang F, Zhuang SM, et al. Tumor size rather than the thyroid invasion affects the prognosis of parathyroid carcinoma without lymph node or distant metastasis. Eur Arch Otorhinolaryngol 2022;279:4587-94. [Crossref] [PubMed]
- Lo WM, Good ML, Nilubol N, et al. Tumor Size and Presence of Metastatic Disease at Diagnosis are Associated with Disease-Specific Survival in Parathyroid Carcinoma. Ann Surg Oncol 2018;25:2535-40. [Crossref] [PubMed]
- Shaha AR, Shah JP. Parathyroid carcinoma: a diagnostic and therapeutic challenge. Cancer 1999;86:378-80. [Crossref] [PubMed]
- Medas F, Erdas E, Loi G, et al. Controversies in the management of parathyroid carcinoma: A case series and review of the literature. Int J Surg 2016;28:S94-8. [Crossref] [PubMed]


