The effect of hypotonic pharmacologic lipodissolution on abdominal free flap perfusion: a case report
Highlight box
Key findings
• In a patient who underwent transverse rectus abdominis musculocutaneous (TRAM) flap surgery after hypotonic pharmacologic lipodissolution (HPL), intraoperative indocyanine green (ICG) imaging showed compromised skin-side perfusion, but deep layer perfusion was stable.
What is known and what is new?
• While studies on the safety and complications of TRAM flap reconstruction after liposuction exist, there is inadequate research specifically focusing on TRAM flap reconstruction after injection procedures.
• In nipple sparing mastectomy cases where minimal skin flap preservation is necessary, a history of HPL may have limited impact on TRAM flap reconstruction. However, in skin sparing mastectomy cases with substantial skin flap preservation needs, meticulous evaluation through techniques like preoperative computed tomography angiography and intraoperative ICG imaging is crucial to minimize the risk of fat necrosis.
What is the implication, and what should change now?
• During preoperative consultations, it would be beneficial to thoroughly investigate not only liposuction and previous abdominal operation history but also procedures that patients consider “simple” in order to enhance flap survivability and patient satisfaction.
Introduction
Since its introduction by Hoefflin in 1999, hypotonic pharmacologic lipodissolution (HPL) has been gradually expanding and gaining popularity (1). HPL is a commonly utilized treatment for abdominal fat reduction, particularly among Asian individuals. In addition to that, various ingredients such as phosphatidylcholine, deoxycholate, L-carnitine, aminophylline, collagenase, among others, are being used in injection lipolysis for body sculpting in areas such as the abdomen, flanks, and thighs (2). Despite the increasing popularity of body contouring through injection procedures, there is a lack of sufficient research on transverse rectus abdominis musculocutaneous (TRAM) flap reconstruction following injection treatments. While studies on the safety and complications of TRAM flap reconstruction after liposuction exist (3-6), there is inadequate research specifically focusing on TRAM flap reconstruction after injection procedures. Also, research on the combination of HPL and TRAM flap elevation, specifically in the context of nipple sparing mastectomy (NSM), remains limited. This case report presents a patient who underwent NSM with free TRAM flap reconstruction, emphasizing the need for thorough evaluation and caution in TRAM flap reconstruction in patients with a history of HPL. We present this case in accordance with the CARE reporting checklist (7) (available at https://gs.amegroups.com/article/view/10.21037/gs-23-445/rc).
Case presentation
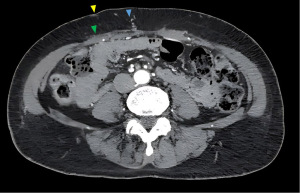
A 54-year-old woman with a history of HPL treatment in November 2022 presented with a diagnosis of right breast cancer, necessitating NSM for oncologic management. In the case of this patient, although her breast size was not substantial, considering the high likelihood of postoperative radiation therapy, complications such as capsular contracture associated with implant insertion were anticipated. Therefore, during the decision-making process, both direct-to-implant insertion and autologous tissue-based reconstruction were considered, and the patient opted for autologous tissue-based reconstruction. In the preoperative computed tomography (CT) angiography, perforators were visualized, but there were partial findings of depression, scar tissue, and abnormal subcutaneous perforator kinking (Figure 1). Considering the possibility of compromised vascularity, the decision was made to proceed with TRAM flap instead of deep inferior epigastric perforator (DIEP) flap reconstruction. The patient was adequately informed about the possibility of flap necrosis and provided informed consent before undergoing autologous tissue-based reconstruction.
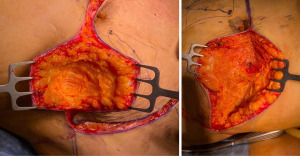
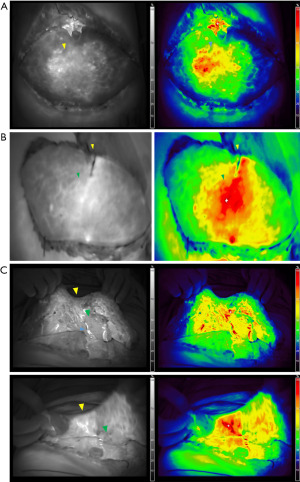
On April 4, 2023, the patient underwent NSM with immediate breast reconstruction using a free TRAM flap. Intraoperative indocyanine green (ICG) fluoroscopy was performed after TRAM flap elevation to assess flap perfusion. Scar tissue was observed in the subcutaneous fat during flap elevation (Figure 2). The ICG images showed a speckled pattern of perfusion on the skin side of the flap, which has not been previously observed by the senior author with experience in over 500 TRAM flap elevations (Figure 3A). For patients with no prior abdominal procedures, ICG fluoroscopy during TRAM flap elevation confirms well-established skin perfusion on the flap’s medial side, similar to the illustration in the figure (Figure 3B). Moreover, the speckled pattern similar to the patient’s case is exceptionally rare. Fortunately, ICG imaging of the underside and the lateral sides of the flap (Figure 3C) did not exhibit decreased perfusion. Flap perfusion was checked again after de-epithelialization, where sufficient dermal bleeding was observed along with well perfused deep dermis on the ICG, indicating the presence of subdermal plexus perfusion (Figure 4). This observation provided further evidence of adequate blood flow within the subdermal plexus, which is critical for ensuring proper healing and viability of the flap.

The patient was discharged on postoperative day 7 without any complications requiring emergency surgery, such as hematoma or flap necrosis. At our institution, a protocol is in place to conduct ultrasound examinations immediately in the outpatient setting for nodules that are palpable and exceed 1 cm in size. Following surgery, evaluations for fat necrosis involve physical examinations at regular intervals, specifically at 2 weeks, 4 weeks, 8 weeks, and 3 months, in the outpatient setting. During the first 3 months of follow-up, no palpable lesions suggestive of fat necrosis were detected in the patient’s breast, and additional investigations such as ultrasound were not performed.
The study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB #B-2308-846-701). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In the field of abdominal fat contouring, procedures such as abdominoplasty and liposuction have been widely used. However, in recent years, various methods such as injection lipolysis, cryolipolysis, and radiofrequency-assisted contouring have gained popularity. Particularly, lipolysis injections have been extensively used in Asian countries for fat reduction in various body areas. While FDA-approved Kybella has clearly disclosed its ingredients, numerous clinics employ different products with undisclosed substances for abdominal fat reduction. Research on the impact of these products on abdominal subcutaneous perfusion is limited. The patient, being well aware that hypotonic pharmacologic dissolution had been performed, led to the meticulous review of a preoperative CT angiography to identify the most suitable perforators for TRAM flap elevation.
Due to the lack of detailed information regarding the prior hyponotic pharmacologic dissolution, including the specific composition of drugs, injection location, and depth, it is challenging to precisely evaluate the impact of the injection. However, based on CT angiography and intraoperative observations, we observed skin retraction, scarring, deterioration of Scarpa’s fascia, and kinking of some perforators. Fortunately, in our case, utilizing the TRAM technique with multiple perforators and continuous flap monitoring throughout the procedure, we did not encounter any acute complications related to flap perfusion.
Additionally, intraoperatively, multiple ICG scans were performed to identify areas of decreased perfusion within the flap. Adequate perfusion was confirmed following de-epithelialization, and the flap was completely inset. Although this case did not require skin due to nipple sparing mastectomy, in cases of skin sparing mastectomy where skin is needed, decreased skin perfusion may increase the risk of complications, such as skin necrosis and wound dehiscence. When considering the detergent effect of phosphatidylcholine, which can cause non-specific cell lysis, it is important to note that it can induce more scarring and be slightly more destructive compared to HPL using osmotic pressure. Taking these factors into account, it is recommended that a more detailed preoperative evaluation is conducted for injection lipolysis procedures other than HPL (8).
The findings from this case report emphasize the importance of individualized assessment and careful evaluation of flap perfusion in patients with a history of HPL undergoing TRAM flap reconstruction. In NSM cases where minimal skin flap preservation is necessary, a history of HPL may have limited impact on TRAM flap reconstruction. However, in skin-sparing mastectomy cases with substantial skin flap preservation needs, meticulous evaluation through techniques like preoperative CT angiography and intraoperative ICG imaging is crucial to minimize the risk of fat necrosis. Unlike nipple-sparing mastectomy, in the skin-sparing mastectomy performed at our institution, there are instances where more than 10×10 cm of skin is resected, necessitating a sufficient abdominal skin envelope to match the size of the contralateral breast.
Accordingly, during preoperative consultations, it would be beneficial to thoroughly investigate not only liposuction and previous abdominal operation history but also procedures that patients consider “simple” in order to enhance flap survivability and patient satisfaction.
Conclusions
This case report highlights the successful NSM with free TRAM flap reconstruction in a patient with a history of HPL. The compromised skin-side perfusion observed in the ICG fluoroscopic images necessitates cautious evaluation and consideration of alternative surgical approaches in cases with significant skin flap preservation requirements. The confirmation of satisfactory deep layer perfusion and subdermal plexus perfusion during de-epithelialization supports the feasibility of TRAM flap reconstruction in cases with minimal skin flap preservation needs.
Further research is needed to explore the implications of HPL on TRAM flap viability and optimize surgical outcomes in patients with a history of HPL undergoing TRAM flap reconstruction.
In the current landscape of increasing options for minimally invasive treatments for abdominal body contouring, there is a need for thorough preoperative evaluations in these areas. This case is considered significant as it demonstrates the potential impact of various procedures, including HPL and lipolysis injections, on abdominal vascularity, emphasizing the importance of detailed preoperative assessment.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-23-445/rc
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-23-445/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-23-445/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB #B-2308-846-701). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hoefflin SM. Hypotonic Pharmacological Lipo-Dissolution (HPL): A Preliminary Report and Study Model. Semin Plast Surg 1999;13:67-84.
- Mahmud K, Crutchfield CE. Lipodissolve for body sculpting: safety, effectiveness, and patient satisfaction. J Clin Aesthet Dermatol 2012;5:16-9.
- Bond ES, Soteropulos CE, Poore SO. The Impact of Abdominal Liposuction on Abdominally Based Autologous Breast Reconstruction: A Systematic Review. Arch Plast Surg 2022;49:324-31. [Crossref] [PubMed]
- Karanas YL, Santoro TD, Da Lio AL, et al. Free TRAM flap breast reconstruction after abdominal liposuction. Plast Reconstr Surg 2003;112:1851-4. [Crossref] [PubMed]
- Papas Y, Bou-Merhi J, Odobescu A, et al. Partial DIEP flap loss in a patient with history of abdominal liposuction. Ann Chir Plast Esthet 2021;66:257-60. [Crossref] [PubMed]
- Kim J, Park JKH, Heo CY. Successful umbilicus salvage following concurrent infraumbilical single-port myomectomy and free transverse rectus abdominis myocutaneous flap elevation: a case report. Arch Aesthetic Plast Surg 2021;27:139-42.
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Rotunda AM, Suzuki H, Moy RL, et al. Detergent effects of sodium deoxycholate are a major feature of an injectable phosphatidylcholine formulation used for localized fat dissolution. Dermatol Surg 2004;30:1001-8. [Crossref] [PubMed]