
Revisiting meta-analysis: surgical approaches for papillary thyroid carcinoma of isthmus
First, we are very grateful to Dr. Dai and Dr. Feng for their questions and suggestions, which were helpful to our study (1). When we set up a topic of this study, we set up the inclusion and exclusion criteria (2). There is no doubt that strict inclusion and exclusion criteria are important for meta-analysis, and the quality of the included studies determines the rigor of the meta-analysis. However, due to the small amount of original literature having published on surgical modality selection for papillary thyroid carcinoma of isthmus (PTCI), we included all of the retrieved study in our data analysis, which led to the questions about our article raised by Dr. Dai and Dr. Feng.
Therefore, according to the suggestions made by Dai et al., references [22] and [23] did not meet the inclusion criteria that we established when we set up the study, which was our overlook. We re-searched for articles on papillary carcinoma of the thyroid isthmus and found a new study published by Dr. Dan and colleagues in August 2023 (3). After careful review, we found that this study met our inclusion criteria. Therefore, we hereby include this study in our analysis with updated findings as follows.
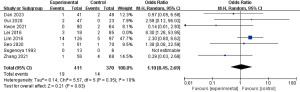
Meta-analysis for tumor recurrence rate
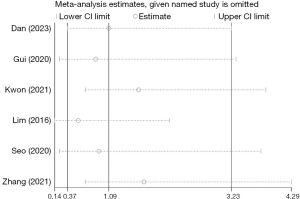
The results of the study after the inclusion of Dan et al. 2023 showed that the overall tumor recurrence rate was the same as that obtained in the previous studies, i.e., there was no statistically significant difference in tumor recurrence rate between the two groups (3). A total of 781 individuals were included, with 19 tumor recurrences in the less than total thyroidectomy group and 14 tumor recurrences in the total thyroidectomy group [OR =1.10 (95% CI: 0.45, 2.69); P=0.35, and I2=10%], which showed a low degree of heterogeneity (Figure 1). It was imported into Stata 17, Influence Analysis, metan-based (metaninf) board, and the random effects model, M-H method was selected to analyze the OR values, and the results were validated by deleting one article at a time, as shown in Figure 2, which showed that the 95% CI crossed the null line after deleting any article.
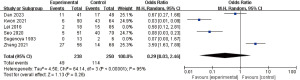
Incidence rate
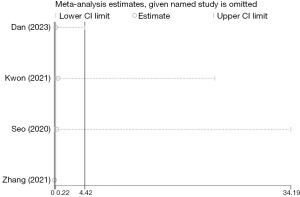
Regarding the incidence of postoperative complications between the two groups, Dan et al.’s study (3) proposed that the difference in the incidence of temporary postoperative hypocalcemia between the two groups was statistically significant (P=0.032), but the difference in the incidence of permanent postoperative hypocalcemia, hoarseness, and choking on drinking water was not statistically significant. The studies describing the presence of postoperative complications included a total of 488 people, 49 cases of postoperative complications in the less-than-total thyroidectomy group and 114 cases in the total thyroidectomy group. The results of the meta-analysis of the overall complication rate showed that there was no statistically significant difference in the overall postoperative complication rate between the two groups, with OR =0.29 (95% CI: 0.03, 2.46), P=0.26, and I2=95%, which was highly heterogeneous (Figure 3). There was significant heterogeneity in the studies (P<0.00001, I2=95%). The results of the sensitivity analysis showed that none of the included studies affected the overall results, so the overall results can be considered stable and reliable (Figure 4).
There is a controversy about whether prophylactic central lymph node dissection should be performed for papillary carcinoma of the thyroid isthmus without preoperative lymph node metastasis, and the studies we included did not describe the lymph node dissection of the two groups in detail, and thus relevant subgroup analyses could not be performed. In the future, we expect more high-quality randomized controlled trials to supplement the evidence and thus guide the surgical treatment strategy for papillary carcinoma of the thyroid isthmus and bring better prognosis to patients.
Finally, thanks again to Dr. Dai and Dr. Feng for their questions, which have undoubtedly promoted greater rigor in our research.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gland Surgery. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-24-39/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dai Y, Feng Q. Papillary thyroid carcinoma of isthmus: total thyroidectomy or isthmusectomy? Gland Surg 2024;13:465-66. [Crossref]
- Gong H, Jiang Y, Su A. Total thyroidectomy versus less-than-total thyroidectomy for papillary thyroid carcinoma of isthmus: a systematic review and meta-analysis. Gland Surg 2023;12:1525-40. [Crossref] [PubMed]
- Dan J, Tan J, Guo Y, et al. Isthmusectomy for papillarythyroid carcinoma in the isthmus: The less the better. Asian J Surg 2024;47:367-72. [Crossref] [PubMed]


