A WeChat-based nursing intervention program improves the postoperative rehabilitation of breast cancer patients: results from a randomized controlled trial
Highlight box
Key findings
• This study found that a WeChat-based multimodal nursing program (WCBMNP) reduced the fear of cancer recurrence (FCR) and significantly increased the health-related quality of life (HRQoL) of women with breast cancer (BC) postoperatively.
What is known, and what is new?
• WeChat use had been previously reported to be useful for healthcare intervention, whereby it could complement regional nursing resources and serve a larger population despite geographical restrictions.
• Our study showed the effectiveness of a WCBMNP in decreasing FCR and increasing the HRQoL of BC patients postoperatively.
What is the implication, and what should change now?
• The WCBMNP has potential advantages for BC women. It could be implemented as part of these patients’ postoperative protocol to improve their care.
Introduction
Breast cancer (BC) is the most prevalent malignancy among women worldwide, and the second leading cause of cancer mortality in women (1), The primary approach for early-stage BC involves surgery with additional therapies, such as endocrine therapy, radiotherapy, and chemotherapy (2-4). Unfortunately, these treatments have adverse effects, including pain, fatigue, and sleep disturbances (5), which significantly affect the health-related quality of life (HRQoL) of patients postoperatively (6).
BC survivors commonly experience uncertainty, anxiety, and the fear of cancer recurrence (FCR) (7-9). Psychological issues, particularly the FCR, are important unmet needs among ambulatory BC patients, affecting over half of BC patients (10). The FCR is prevalent among BC patients and has been shown to be correlated with diminished HRQoL (11-13).
Numerous initiatives to improve physical health, psychological state, and spiritual well-being, etc. have been implemented to improve the HRQoL of women with BC (14-16). Despite achieving some satisfactory results, there is a lack of programs that adopt a holistic methodology that integrates physical, psychological, and social rehabilitation in the postoperative phase (17-20). Leveraging on the extensive accessibility of the mobile internet and the widespread adoption of WeChat, a no-cost communication platform widely embraced by Chinese adults (21), a WeChat-based multimodal nursing program (WCBMNP) has emerged as an appropriative intervention to improve nursing care and to serve a larger population despite geographical restrictions (22). This trial sought to examine the potential advantages of a WCBMNP in women with BC postoperatively. We present this article in accordance with the CONSORT reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-24-40/rc).
Methods
Participants
BC patients were recruited using the method of convenience sampling. This randomized clinical trial was conducted at the Xinhua Hospital Affiliated with Shanghai Jiaotong University School of Medicine, and the participants provided informed consent. To be eligible for inclusion in this study, the patients had to meet the following inclusion criteria: (I) patient with primary diagnosis of histologically confirmed BC; (II) age ≥18 but <55 years; (III) patient received breast surgery within the last 12 months; (IV) patients are in remission; and (V) patient who are able to complete an electronic patient-reported outcome measure via WeChat. Patients were excluded from the study if they met any of the following exclusion criteria: (I) had other active, severe physical illness, and/or a current or prior history of cancers other than BC; (II) were unable to comprehend Chinese; and/or (III) were engaged in ongoing follow-up, or were being treated by psychiatrists, or other mental health professionals. Post-surgery, all the patients received patient-controlled analgesia. This is a two-parallel study, and allocation ratio is about 1:1. The study protocol was approved by the Institutional Review Board of the Xinhua Hospital Affiliated with Shanghai Jiaotong University School of Medicine (No. XHEC-D-2023-203). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Intervention cohort
Patients in the intervention cohort received the WCBMNP in addition to routine nursing care (23) (details of the intervention are shown in Table 1). The intervention was administered throughout the hospitalization period and up to 6 months post-surgery. Rigorous measures were implemented to prevent inter-cohort contamination. Patients were physically segregated in distinct sections of the BC department, and any form of interaction between the cohorts was strictly prohibited. Patients in each cohort were also cared for by designated staff, with no overlap of the staff for each cohort.
Table 1
| Stages | Physical rehabilitation | Psychological rehabilitation | Social rehabilitation | Implementation in WeChat platform |
|---|---|---|---|---|
| Stage I: from hospital admission to the time of surgery | Provision of individualized information†,‡: illness condition; planned surgery and adjuvant therapy; diet, rest, and activity | Relaxation training†,‡: e.g., muscle relaxation, music listening, meditation (face-to-face and video frequency) | Adaptation to patient role†,‡: cooperating with the treatment; doing self-care activities under permission | Web-MNP group: |
| Surgical side upper limb exercise training†,‡: finger → wrist → elbow → shoulder → upper limb (face-to-face and video frequency) | Feeling expression (face-to-face): writing (e.g., diary); communicating with relatives, significant others, or peers | Social training†,‡: keeping original social relationship; avoiding self-isolation; establishing good relationship with professional staff and peers | Establishing WeChat platform | |
| Stage II: 0–24 weeks following surgery | Provide individualized information†,‡: post-surgery complications; adverse effects of adjuvant therapy; complications regarding peripherally inserted central catheter or implantable venous access port | Performing need-oriented psychological counseling | Role transformation†,‡: progressively completing the role transformation from patient to the original family/social role; performing original family/social role well | Recruiting the patient with permission |
| Self-surveillance and recurrence prevention after hospital discharge†,‡ | Family/spouse (guided by professional staff face-to-face): understanding feelings and meeting demands of the patient; accompanying the patient as much as possible | From hospital admission to 6 months following surgery, continuously | ||
| Developing and updating patient-oriented plan of diet, rest, and activity†,‡ | Peers (guided by professional staff face-to-face): sharing negative psychological state coping experiences | Professional staff: | ||
| Coping with fatigue and poor sleep†,‡: keeping physical activity under permission, relaxation training (e.g., muscle relaxation, listening to music, meditation) | Daily delivery of the BC rehabilitation information (5 p.m.–7 p.m.) | |||
| Pain relieving†,‡: medication and non-medication (e.g., muscle relaxation training, listening to music) | Assessing and responding to the rehabilitation problems submitted by the patients as soon as possible | |||
| Patients: | ||||
| Submitting rehabilitation problems | ||||
| Sharing rehabilitation experiences |
†, dissemination of pertinent information (e.g., employing textual content, images, audio, or video formats) on the WeChat platform aligned with the face-to-face intervention; ‡, need-oriented patient-professional staff or patient-peer communication in WeChat platform during the intervention period based on face-to-face intervention. BC, breast cancer.
Control cohort
The patients allocated to the control cohort received a standard nursing intervention, which included standard health education protocols, vital sign monitoring, postoperative complication surveillance, and postoperative drainage-tube management.
Evaluation metrics
The patients were assessed at 2, 8, and 24 weeks post-surgery in the study period (weeks 0–24). Our primary endpoint was Japanese version of the Concerns About Recurrence Scale (CARS-J) and secondary endpoint was FACT-B. FCR was assessed using the fear scores of the CARS-J (24). Fear scores ranged from 4 to 24, with a higher score indicating an increased FCR. This scale was also used as a screening tool to evaluate FCR.
The Chinese Functional Assessment of Cancer Therapy-Breast (FACT-B, version 4.0), which has been verified previously among BC patients in mainland China (25), was used to gather HRQoL information. The evaluation covered social/family, functional, emotional, and physical well-being, and included a “BC-specific subscale for additional concerns”. The FACT-B comprises 36 items, and the patients were asked to rate each item on a five-point Likert scale, on which 0= not at all, 1= a little bit, 2= somewhat, 3= quite a bit, and 4= very much. Potential total scores ranged from 0 to 144, and a higher score indicated improved HRQoL (26); Cronbach’s α in this study was 0.82.
The Nursing Rating Scale (NRS) is a succinct numerical adaptation of the visual analog scale, wherein individuals evaluate the intensity of a particular sensation on a continuum ranging from 0 to 10 (27). Widely used as a straightforward tool for evaluating feelings in clinical nursing settings (28), the NRS was employed in this study to evaluate patients’ fatigue, sleep, and pain; 0 represented no pain/fatigue, or high sleep quality, while 10 represented severe pain/fatigue, or bad sleep quality.
Statistical analysis
The data were examined using SPSS software (version 23.1, IBM Corp., Armonk, NY, USA). To assess the baseline characteristic differences between the cohorts, multiple statistical tests (e.g., Fisher’s exact test, the chi-square test, and the independent t-test) were performed. A P value ≤0.05 was considered statistically significant.
Sample size
We calculated that group sample sizes of 110 patients (55 in group 1; 55 in group 2) would provide 80% power to reject the null hypothesis of equal means when the mean difference is 7 [108–101] with standard deviations of 13 for group 1 and 13 for group 2 at a two-sided alpha of 0.05. Given an anticipated dropout rate of 12%, total sample size required is 125 (62 in intervention group 1; 63 in control group 2).
Randomization and implementation
Director of this trial and surgeon were used computer randomize sheet to reroll patients into two cohorts. Trials were using single blind mechanism for patients after assignment to interventions.
Results
Study design
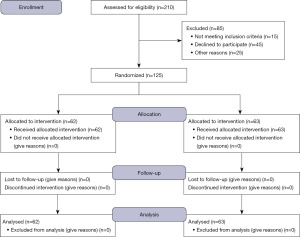
From June 2021 to July 2022, 210 participants were assessed for eligibility. All the participants were women. Of these patients, 85 participants were excluded (Figure 1). The remaining 125 patients were randomly allocated to either the intervention or the control cohort.
Mean age of the intervention cohort was 41 [27–53] years old, and mean age of the control cohort was 43 [25–54] years old. There were no statistically significant differences between the two cohorts in terms of their demographics and pathological characteristics (Table 2).
Table 2
| Variables | Intervention cohort (n=62) | Control cohort (n=63) | P value |
|---|---|---|---|
| Age (years) | 0.126 | ||
| ≤45 | 32 | 30 | |
| >45 | 30 | 33 | |
| Educated | 0.848 | ||
| Junior middle school and below | 5 | 7 | |
| Senior middle school | 32 | 37 | |
| Undergraduate | 25 | 19 | |
| Marital status | 0.884 | ||
| Married | 19 | 16 | |
| Never married/separated/divorced/widowed | 43 | 47 | |
| Employment | 0.584 | ||
| Unemployed | 21 | 18 | |
| Employed | 41 | 45 | |
| Tumor stage | 0.312 | ||
| <III | 32 | 27 | |
| ≥III | 30 | 36 | |
| Income (RMB/month) | 0.551 | ||
| <3,000 | 12 | 9 | |
| 3,000–7,000 | 25 | 28 | |
| >7,000 | 25 | 26 | |
| Breast surgery | 0.843 | ||
| Modified radical mastectomy | 19 | 23 | |
| Total mastectomy | 12 | 17 | |
| Breast conserving surgery | 31 | 23 | |
| Axillary surgery type | 0.525 | ||
| Sentinel lymph node biopsy | 23 | 28 | |
| Axillary lymph node dissection | 39 | 35 | |
| Radiotherapy | 0.486 | ||
| Yes | 17 | 19 | |
| No | 45 | 44 | |
| Neo-adjuvant chemotherapy | 0.814 | ||
| Yes | 23 | 20 | |
| No | 39 | 43 | |
| Adjuvant chemotherapy | 0.709 | ||
| Yes | 32 | 30 | |
| No | 30 | 33 |
The WCBMNP improved the HRQoL of BC patients postoperatively
Analysis of the scores using FACT-B showed the dynamic evolution of physical well-being with a pronounced effect over time (P<0.05) (Table 3). Social/family and functional well-being demonstrated the interplay of time, cohort, and cohort-time interaction effects. Emotional well-being manifested time effects (P<0.05) and cohort-time interaction effects (P<0.05). The “BC-specific subscale for additional concerns” reflected the influence of cohort effects (P<0.05) and time (P<0.05) effects. The overall FACT-B scores were affected by cohort (P<0.05), time (P<0.05), and the interaction of cohort-time (P<0.05). These suggested that WCBMNP improved the HRQoL of BC patients postoperatively.
Table 3
| Cohort | Baseline | 2 weeks after surgery | 8 weeks after surgery | 24 weeks after surgery | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Score | Score | Change from baseline (95% CI) |
Score | Change from baseline (95% CI) |
Score | Change from baseline (95% CI) |
||||
| PWB† | ||||||||||
| Intervention | 24.90±2.73 | 22.05±1.26 | −2.77 (−4.23, −1.54) | 21.93±0.69 | −3.73 (−8.56, −3.55) | 22.37±2.17 | –1.28 (–8.73, –0.12) | |||
| Control | 24.39±2.79 | 21.57±2.57 | −2.44 (−5.63, −2.13) | 22.47±0.46 | −4.89 (−7.34, −2.98) | 23.77±1.02 | –1.68 (–2.68, –0.78) | |||
| MD (95% CI) | −0.71 (−1.83, 0.56) | 0.55 (−0.83, 2.13) | 0.71 (−2.03, 3.51) | −0.87 (−1.99, 1.59) | ||||||
| SWB‡ | ||||||||||
| Intervention | 22.08±2.34 | 21.87±1.23 | −2.47 (−5.45, −2.19) | 20.29±0.62 | −2.96 (−7.43, −0.84) | 22.89±2.64 | 0.15 (−0.14, 3.24) | |||
| Control | 21.83±3.41 | 19.08±2.46 | −1.21 (−3.57, −0.44) | 18.98±0.14 | −2.82 (−9.34, −0.73) | 19.11±1.34 | −2.71 (−7.62, −0.63) | |||
| MD (95% CI) | 1.55 (0.45, 3.61) | 1.89 (1.03, 3.92) | 6.11 (2.81, 10.33) | |||||||
| EWB§ | ||||||||||
| Intervention | 15.89±4.51 | 17.36±2.31 | 2.58 (1.22, 6.16) | 21.75±2.75 | 5.97 (1.56, 8.16) | 20.86±2.52 | 4.15 (2.53, 7.34) | |||
| Control | 16.73±4.72 | 18.05±1.98 | 1.82 (0.59, 5.51) | 19.67±0.62 | 2.79 (1.15, 9.72) | 19.94±1.62 | 2.93 (0.35, 9.18) | |||
| MD (95% CI) | −1.97 (−3.11, 0.09) | −1.16 (−2.85, 0.53) | 1.76 (1.23, 5.17) | 1.71 (–1.04, 5.91) | ||||||
| FWB¶ | ||||||||||
| Intervention | 21.06±2.52 | 17.84±1.61 | −3.69 (−6.23, −1.98) | 23.36±2.94 | −1.97 (−6.56, −0.57) | 22.57±2.52 | 2.91 (0.96, 3.72) | |||
| Control | 20.14±1.23 | 12.25±2.81 | −3.57 (−7.23, −1.41) | 18.32±1.53 | −2.93 (−5.23, −1.99) | 17.03±1.34 | −1.72 (−2.51, 0.15) | |||
| MD (95% CI) | 1.85 (−0.11, 4.01) | 3.72 (2.85, 8.66) | 2.73 (1.65, 6.31) | 3.74 (2.01, 19.05) | ||||||
| BCSǁ | ||||||||||
| Intervention | 32.21±0.65 | 29.57±2.69 | −2.69 (−5.23, −2.23) | 28.12±0.92 | −4.39 (−8.45, −2.31) | 29.31±2.85 | −3.24 (−7.38, −1.12) | |||
| Control | 32.78±0.54 | 22.33±2.43 | −2.28 (−6.31, −1.46) | 26.44±2.47 | −3.02 (−7.35, −1.78) | 26.82±2.79 | −2.83 (−5.3, −1.19) | |||
| MD (95% CI) | 1.67 (−0.32, 3.69) | 2.42 (0.89, 6.91) | 6.91 (2.52, 14.64) | 9.22 (7.09, 12.06) | ||||||
| Total score# | ||||||||||
| Intervention | 116.14±12.01 | 108.69±13.58 | −12.6 (−16.36, −2.08) | 115.45±13.77 | −3.34 (−7.45, 0.58) | 118.00±10.55 | 4.82 (−3.33, 8.38) | |||
| Control | 115.87±13.21 | 93.28±13.01 | −11.67 (−19.42, −2.57) | 105.88±12.06 | −15.34 (−19.42, −1.63) | 106.67±12.4 | −6.84 (−12.05, 0.94) | |||
| MD (95% CI) | 2.57 (−2.18, 5.92) | 9.42 (5.09, 16.74) | 8.83 (3.62, 16.65) | 12.51 (6.83, 19.62) | ||||||
Data are presented as mean ± SD, unless otherwise stated. †, PWB model: (cohort) F=1.03; P=0.563; (time) F=6.15, P<0.001; (cohort × time interaction) F=1.03, P=0.342; ‡, SWB model: (cohort) F=10.09; P< 0.001; (time) F=11.82, P<0.001; (cohort × time interaction) F=5.49, P=0.015; §, EWB model: (cohort) F=0.82; P=0.632; (time) F=9.99, P<0.001; (cohort × time interaction) F=5.46, P=0.001; ¶, FWB model: (cohort) F=5.32; P<0.001; (time) F=9.62, P<0.001; (cohort × time interaction) F=11.78, P=0.006; ǁ, BCS model: (cohort) F=5.66; P<0.001; (time) F=9.65, P<0.001; (cohort × time interaction) F=0.83, P=0.283; #, total score model: (cohort) F=6.35; P<0.001; (time) F=6.66, P<0.001; (cohort × time interaction) F=8.88, P=0.007. A linear mixed model was used to analyze the in-cohort variations and between-cohort variations of FACT-B scores. Baseline measurements of the FACT-B total and five subscales’ scores were incorporated as covariates, with cohort, time, and cohort × time interaction as fixed effects, and patients as random effects. FACT-B, Functional Assessment of Cancer Therapy-Breast; CI, confidence interval; PWB, physical well-being; MD, mean difference; SWB, social/family well-being; EWB, emotional well-being; FWB, functional well-being; BCS, BC-specific subscale for additional concerns; BC, breast cancer; SD, standard deviation.
Conversely, pain, fatigue, and sleep, evaluated using the NRS did not exhibit any significant cohort effects (P>0.05). Both pain and fatigue displayed time effects (P<0.05), while only pain showed a cohort-time interaction effect (P<0.05) (Table 4).
Table 4
| Cohort | Baseline | 2 weeks after surgery | 8 weeks after surgery | 24 weeks after surgery | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Score | Score | Change from baseline (95% CI) |
Score | Change from baseline (95% CI) |
Score | Change from baseline (95% CI) |
||||
| Pain† | ||||||||||
| Intervention | 1.88±1.91 | 1.72±1.76 | −0.02 (−1.05, 0.85) | 1.87±1.85 | −0.12 (−1.06, 1.24) | 1.81±1.78 | −0.56 (−1.75, 0.89) | |||
| Control | 1.33±1.56 | 2.86±2.12 | 1.69 (0.89, 3.19) | 2.97±1.31 | 1.78 (0.24, 2.35) | 2.37±1.85 | 1.23 (0.15, 1.97) | |||
| MD (95% CI) | 0.53 (−0.35, 1.78) |
−0.92 (−1.77, −0.02) |
−0.67 (−1.71, −0.19) |
−0.89 (−1.92, 0.34) |
||||||
| Fatigue‡ | ||||||||||
| Intervention | 1.56±1.55 | 2.36±1.46 | 0.93 (−0.08, 1.92) | 2.39±1.57 | 0.69 (−1.42, 1.92) | 2.19±1.31 | 0.84 (−0.32, 2.33) | |||
| Control | 1.75±1.76 | 1.97±2.39 | −0.15 (−0.89, 0.92) | 2.48±1.77 | 0.97 (−0.15, 1.74) | 2.81±1.94 | 0.91 (0.18, 2.15) | |||
| MD (95% CI) | −0.34 (−1.67, 0.87) |
0.67 (−0.22, 1.97) |
−0.23 (−1.84, 0.93) |
−0.78 (−1.93, 0.68) |
||||||
| Sleep§ | ||||||||||
| Intervention | 3.76±1.47 | 2.99±2.32 | −0.78 (−1.83, 0.93) | 2.78±2.67 | −0.83 (−1.52, 0.58) |
2.46±2.69 | –0.93 (–1.72, 0.73) | |||
| Control | 3.82±1.59 | 3.96±2.29 | 0.67 (−0.92, 1.95) | 3.93±2.65 | 0.13 (–0.90, 0.74) | 2.75±2.52 | –0.56 (–1.84, 0.94) | |||
| MD (95% CI) | −0.01 (−2.32, 0.87) |
−0.55 (−1.92, 0.94) |
−0.85 (−3.01, 0.91) |
−0.75 (−1.62, 0.86) |
||||||
Data are presented as mean ± SD, unless otherwise stated. †, pain model: (cohort) F=4.69, P=0.05; (time) F=3.02, P=0.01; (cohort time interaction) F=4.19, P=0.005; ‡, fatigue model: (cohort) F=0.03, P=0.67; (time) F=4.78, P=0.03; (cohort × time interaction) F=1.03, P=0.64; §, sleep model: (cohort) F=1.67, P=0.35; (time) F=1.73, P=0.43; (cohort × time interaction) F=0.68, P=0.85. A linear mixed model was employed to examine changes in the cohorts and make comparisons between the cohorts in terms of their pain, fatigue, and sleep scores measured using the NRS. Baseline measurements of pain, fatigue, and sleep scores were used as covariates, with cohort, time, and cohort × time interplay as fixed effects, while the subject was treated as a random effect. CI, confidence interval; MD, mean difference; SD, standard deviation; NRS, Nursing Rating Scale.
The WCBMNP reduced the FCR of BC patients postoperatively
Regarding FCR, the patients in the intervention cohort exhibited a statistically significant improvement in their CARS-J scores at 8 and 24 weeks, compared to the control cohort (Table 5, Figure 2). This hence demonstrated that WCBMNP reduced the FCR of BC patients postoperatively. However, within the intervention cohort, there were no significant differences in the outcomes observed at 8 and 24 weeks in terms of the CARS-J (see Figure 2 and Table 6).
Table 5
| Variables | Intervention cohort vs. control cohort | ||
|---|---|---|---|
| Adjusted difference | 95% CI | P | |
| CARS-J: 2 weeks | −0.87 | −1.58 to 0.59 | 0.463 |
| CARS-J: 8 weeks | −0.73 | −1.25 to −0.34 | <0.01 |
| CARS-J: 24 weeks | −0.99 | −2.14 to −0.51 | <0.01 |
CARS-J, Japanese version of the Concerns About Recurrence Scale; CI, confidence interval.
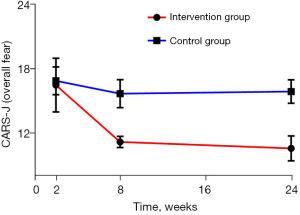
Table 6
| Variables | Differences in least square | ||
|---|---|---|---|
| Adjusted difference | 95% CI | P | |
| CARS-J: 2 vs. 8 weeks | −0.79 | −1.31 to −0.27 | <0.01 |
| CARS-J: 8 vs. 24 weeks | −0.94 | −1.04 to 0.291 | 0.532 |
| CARS-J: 2 vs. 24 weeks | −0.82 | −1.83 to −0.28 | <0.01 |
CARS-J, Japanese version of the Concerns About Recurrence Scale; CI, confidence interval.
Discussion
This study showed the benefits of a WCBMNP on women with BC postoperatively, notably resulting in an increase in HRQoL and a decrease in FCR. Hence, WCBMNP could be implemented as a potential tool to improve the care for the post-surgery rehabilitation of BC patients.
Patients in both the intervention and control cohorts showed significant decreases in their FACT-B total scores 2 weeks post-surgery compared to the baseline, which indicated a substantial decrease in HRQoL in the immediate postoperative phase. This finding was also concordant with the findings in earlier studies (29-31). However, patients in the intervention cohort had notably increased FACT-B total scores in comparison to those in the control cohort at various study time intervals, which suggested that the WCBMNP could have a positive effect of increasing patients’ HRQoL. At the 8- and 24-week follow-up periods, the intervention cohort’s average FACT-B scores became similar to that at the baseline, which indicated that the patients exhibited a swift return to their preoperative health status as early as 8 weeks post-surgery. Conversely, the control cohort’s average FACT-B scores consistently lagged significantly behind both the control cohort’s baseline score and the intervention cohort’s score during the later period of 24 weeks follow-up. The control cohort’s health status only resembled their status at the baseline at the 6-month post-surgery mark; however, the control cohort’s total FACT-B score remained significantly lower than that of the intervention cohort at the same juncture. This affirmed our hypothesis regarding the positive effect of the WCBMNP on patients’ HRQoL at the three assessed time points, underscoring its effectiveness in enhancing HRQoL for BC patients postoperatively.
In relation to the FACT-B subscales, the changes in the social/family and functional well-being domains mirrored those of the overall score, which suggested that the WCBMNP facilitated substantial improvements during the postoperative follow-up period. In comparison to the baseline, both cohorts exhibited significantly reduced scores for the “BC-specific subscale for additional concerns” at the 6-month follow-up, which suggested that the persistent BC-specific concerns may be attributable to the adverse effects of the adjuvant therapies or the relatively brief follow-up duration. The intervention cohort exhibited a markedly elevated score on this subscale compared to that of the control cohort.
In contrast, no cohort effects were evident in terms of patients’ physical and emotional well-being. Nonetheless, the intervention cohort exhibited a discernible upward trajectory in these two subscales during the follow-up period, suggesting that the WCBMNP conferred a potential advantage in these two aspects. Despite this positive trend, the post-surgical physical well-being score of the intervention cohort remained significantly lower than the baseline score, mirroring the observations in the “BC-specific subscale for additional concerns” at the 6-month post-surgery juncture. This emphasized the need to pay increased attention to patients’ physical health during the early stages of rehabilitation. Future investigations should consider a prolonged intervention and follow-up period, such as 12 months, so that a more comprehensive understanding can be gained.
Contrary to our secondary hypothesis, our findings failed to substantiate the proposition that the WCBMNP could alleviate sleep disorders, pain, and fatigue at the three-time points. The intervention cohort had lower sleep, pain, and fatigue scores than the control cohort at the 6-month post-surgery mark; however, these score disparities, in both the intervention cohort and between the intervention and control cohorts, were not statistically significant. This implies that, in the initial 6-month period post-surgery, the WCBMNP did not have a notable effect in mitigating sleep disorders, pain, and fatigue. Notably, patients in the control cohort exhibited significantly elevated pain and fatigue scores at 6 months post-surgery compared to the baseline, which shows the inadequacy of routine nursing care in ameliorating these adverse effects. Consequently, the effects of the WCBMNP on pain and fatigue warrant further exploration in future research with an extended follow-up period.
The present study showed the effectiveness of the WCBMNP in mitigating the FCR in BC survivors. Our findings revealed a statistically significant increase in the CARS-J scores of the patients in the intervention cohort at week 8 in comparison to the control cohort. However, one limitation of this study was that the potential effects of the WCBMNP on depression, as well as patients’ unmet psychological needs was not studied. Given that depression and unmet psychological needs frequently contribute to psychological distress in cancer patients, future research needs to be conducted to examine the effectiveness of smartphone-based psychological therapies in addressing various facets of distress.
Conclusions
In summary, our study showed the effectiveness of the WCBMNP in reducing FCR and significantly enhancing HRQoL in BC patients postoperatively. This intervention may be applied in the early stages of patients’ rehabilitation journeys.
Acknowledgments
Funding: This study was supported by funding from
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-24-40/rc
Trial Protocol: Available at https://gs.amegroups.com/article/view/10.21037/gs-24-40/tp
Data Sharing Statement: Available at https://gs.amegroups.com/article/view/10.21037/gs-24-40/dss
Peer Review File: Available at https://gs.amegroups.com/article/view/10.21037/gs-24-40/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-24-40/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was approved by the Institutional Review Board of the Xinhua Hospital Affiliated with Shanghai Jiaotong University School of Medicine (No. XHEC-D-2023-203). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The participants provided informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Donahue PMC, MacKenzie A, Filipovic A, et al. Advances in the prevention and treatment of breast cancer-related lymphedema. Breast Cancer Res Treat 2023;200:1-14. [Crossref] [PubMed]
- Nolan E, Lindeman GJ, Visvader JE. Deciphering breast cancer: from biology to the clinic. Cell 2023;186:1708-28. [Crossref] [PubMed]
- Hu W, Zheng W, Du J, et al. TIPE2 sensitizes breast cancer cells to paclitaxel by suppressing drug-induced autophagy and cancer stem cell properties. Hum Cell 2023;36:1485-500. [Crossref] [PubMed]
- Gordon NH, Siminoff LA. Measuring quality of life of long-term breast cancer survivors: the Long Term Quality of Life-Breast Cancer (LTQOL-BC) Scale. J Psychosoc Oncol 2010;28:589-609. [Crossref] [PubMed]
- Akechi T, Okuyama T, Endo C, et al. Patient's perceived need and psychological distress and/or quality of life in ambulatory breast cancer patients in Japan. Psychooncology 2011;20:497-505. [Crossref] [PubMed]
- Luigjes-Huizer YL, Tauber NM, Humphris G, et al. What is the prevalence of fear of cancer recurrence in cancer survivors and patients? A systematic review and individual participant data meta-analysis. Psychooncology 2022;31:879-92. [Crossref] [PubMed]
- Harrison JD, Young JM, Price MA, et al. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer 2009;17:1117-28. [Crossref] [PubMed]
- Koch L, Jansen L, Brenner H, et al. Fear of recurrence and disease progression in long-term (≥ 5 years) cancer survivors--a systematic review of quantitative studies. Psychooncology 2013;22:1-11. [Crossref] [PubMed]
- Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv 2013;7:300-22. [Crossref] [PubMed]
- Sharpe L, Curran L, Butow P, et al. Fear of cancer recurrence and death anxiety. Psychooncology 2018;27:2559-65. [Crossref] [PubMed]
- Butow P, Sharpe L, Thewes B, et al. Fear of Cancer Recurrence: A Practical Guide for Clinicians. Oncology (Williston Park) 2018;32:32-8.
- Prins JB, Deuning-Smit E, Custers JAE. Interventions addressing fear of cancer recurrence: challenges and future perspectives. Curr Opin Oncol 2022;34:279-84. [Crossref] [PubMed]
- Hanprasertpong J, Geater A, Jiamset I, et al. Fear of cancer recurrence and its predictors among cervical cancer survivors. J Gynecol Oncol 2017;28:e72. [Crossref] [PubMed]
- Reich RR, Lengacher CA, Alinat CB, et al. Mindfulness-Based Stress Reduction in Post-treatment Breast Cancer Patients: Immediate and Sustained Effects Across Multiple Symptom Clusters. J Pain Symptom Manage 2017;53:85-95. [Crossref] [PubMed]
- Jafari N, Farajzadegan Z, Zamani A, et al. Spiritual therapy to improve the spiritual well-being of Iranian women with breast cancer: a randomized controlled trial. Evid Based Complement Alternat Med 2013;2013:353262. [Crossref] [PubMed]
- Testa A, Iannace C, Di Libero L. Strengths of early physical rehabilitation programs in surgical breast cancer patients: results of a randomized controlled study. Eur J Phys Rehabil Med 2014;50:275-84.
- Andersen KG, Duriaud HM, Jensen HE, et al. Predictive factors for the development of persistent pain after breast cancer surgery. Pain 2015;156:2413-22. [Crossref] [PubMed]
- Mejdahl MK, Mertz BG, Bidstrup PE, et al. Preoperative Distress Predicts Persistent Pain After Breast Cancer Treatment: A Prospective Cohort Study. J Natl Compr Canc Netw 2015;13:995-1003; quiz 1003. [Crossref] [PubMed]
- Bødtcher H, Bidstrup PE, Andersen I, et al. Fatigue trajectories during the first 8 months after breast cancer diagnosis. Qual Life Res 2015;24:2671-9. [Crossref] [PubMed]
- Karlsen RV, Frederiksen K, Larsen MB, et al. The impact of a breast cancer diagnosis on health-related quality of life. A prospective comparison among middle-aged to elderly women with and without breast cancer. Acta Oncol 2016;55:720-7. [Crossref] [PubMed]
- Li WW, Toh P. WeChat-Based Intervention for Chinese Immigrants With Hypertension: Development and Evaluation Study. Asian Pac Isl Nurs J 2023;7:e45769. [Crossref] [PubMed]
- Liang J, Liu JE, Mak YW, et al. Preliminary effects of a WeChat-based educational intervention on social participation among older adults in a community. Int J Older People Nurs 2023;18:e12573. [Crossref] [PubMed]
- Zhou K, Wang W, Zhao W, et al. Benefits of a WeChat-based multimodal nursing program on early rehabilitation in postoperative women with breast cancer: A clinical randomized controlled trial. Int J Nurs Stud 2020;106:103565. [Crossref] [PubMed]
- Momino K, Akechi T, Yamashita T, et al. Psychometric properties of the Japanese version of the Concerns About Recurrence Scale (CARS-J). Jpn J Clin Oncol 2014;44:456-62. [Crossref] [PubMed]
- Wan C, Zhang D, Yang Z, et al. Validation of the simplified Chinese version of the FACT-B for measuring quality of life for patients with breast cancer. Breast Cancer Res Treat 2007;106:413-8. [Crossref] [PubMed]
- Brady MJ, Cella DF, Mo F, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol 1997;15:974-86. [Crossref] [PubMed]
- Alghadir AH, Anwer S, Iqbal A, et al. Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J Pain Res 2018;11:851-6. [Crossref] [PubMed]
- Shafshak TS, Elnemr R. The Visual Analogue Scale Versus Numerical Rating Scale in Measuring Pain Severity and Predicting Disability in Low Back Pain. J Clin Rheumatol 2021;27:282-5. [Crossref] [PubMed]
- Mokhtari-Hessari P, Montazeri A. Health-related quality of life in breast cancer patients: review of reviews from 2008 to 2018. Health Qual Life Outcomes 2020;18:338. [Crossref] [PubMed]
- Dinapoli L, Colloca G, Di Capua B, et al. Psychological Aspects to Consider in Breast Cancer Diagnosis and Treatment. Curr Oncol Rep 2021;23:38. [Crossref] [PubMed]
- Lopes JV, Bergerot CD, Barbosa LR, et al. Impact of breast cancer and quality of life of women survivors. Rev Bras Enferm 2018;71:2916-21. [Crossref] [PubMed]