Thyroid cancer with tracheal invasion: a pathological estimation
Introduction
Occasionally, extrathyroidal thyroid cancers engross the trachea (1). Widely invasive extrathyroidal thyroid cancer invading the aerodigestive tract including larynx, trachea, hypopharynx, and/or esophagus occurs in 1–8% of patients with thyroid cancer (2). De facto, the trachea is the most common site of invasion with an incidence of 35–60% among the patients with tumor invasion, followed by the larynx and the esophagus (3,4).
Extrathyroidal thyroid cancer invading the laryngotracheal system represents a gradual mechanism of infiltration of the tracheal wall layers from the outer to the inner parts of the trachea (1-7).
Tracheal invasion may complicate with hemoptysis or dyspnea and patients often die of hemorrhage or airway obstruction (8). Tracheal infiltration is associated with impaired tumor-free survival and increased disease-specific mortality (9,10).
Advances in surgical techniques have allowed tracheal reconstruction surgery and radical surgery with extended tracheal resection for advanced thyroid cancers, which at the same time preserves vocal cord function (1-3,11-15).
We report here a case of extrathyroidal thyroid cancer involving the trachea treated by tracheal resection. The patient remains alive and well, without vocal dysfunction, 9 years after surgery. We describe the clinical, radiological and pathologic findings of the patient and briefly review the relevant literature. A case series review from 2000 through 2015 is along presented.
Case presentation
A 65-year-old man presented with hemoptysis, cough, neck discomfort for 2 months. Subsequent physical examination showed a large fixed on the deep planes left thyroid mass, 5.0 cm × 3.0 cm on palpation. He had past 20 years history of multinodular goiter, no history of childhood radiation exposure or family history of endocrine abnormalities. There were no remarkable other clinical findings. He reported no symptoms of nervousness, weight loss, palpitation, or fatigue.
Further workup included ultrasonography (US) that confirmed a thyroid nodule, 5.0 cm × 3.0 cm × 2.5 cm. On the left side of the gland with US characteristics associated with an increased risk of cancer. There was no cervical suspected lymphadenopathy for metastasis. Estimated gland volume was 52 cm3. Fine-needle aspiration biopsy performed on the thyroid mass confirmed papillary thyroid carcinoma (PTC). There were no abnormal laboratory findings.
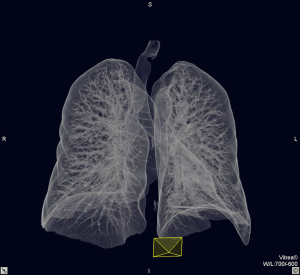
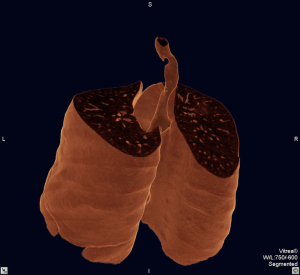
Computed tomography (CT) scan and fiberoptic assessment confirmed the invasiveness of the thyroid mass. Cervical and chest CT images demonstrated a thyroid mass on the left-posterior wall of the trachea (Figure 1). 3D reconstructions revealed a tracheal shift to the right side caused by pressure which involved the region distal to the second ring (Figures 2,3). The tumor did invade the surface of the trachea for 2.0 cm (Figure 4). No distant metastases were noted.


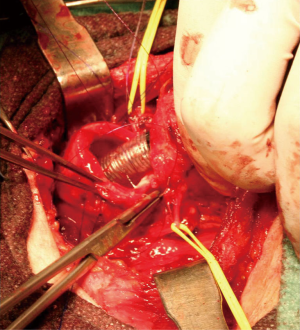
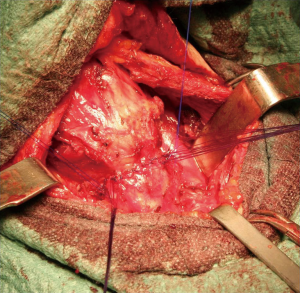
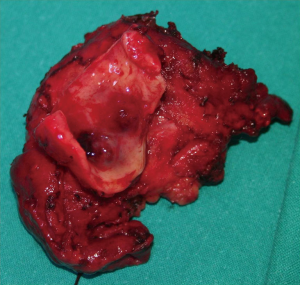
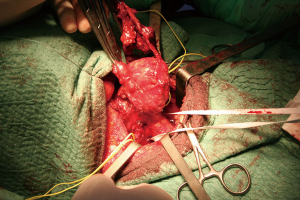
The vocal cords appeared normal at preoperative laryngeal examination. Intraluminal extension was confirmed by endoscopy. Endoscopy showed a semi-circumferential stenosis mass with a slightly irregular and congested surface at 18 cm from the incisor teeth, without evidence of ulceration. Intraluminal biopsy confirmed PTC. Esophagogastroscopy was normal. Based on the above findings, the case was classified as T4N0M0. Complete medical evaluation of physical condition was performed as well. Radical operation was intended (Figures 5,6,7). Bilaterally the recurrent laryngeal nerves were monitored and preserved. The trachea was resected including three rings together with cancer (Figure 8). Cervical lymph node dissection was not performed. No macroscopic residual cancer could be found on intraoperative frozen sections of the trachea. The end-to-end tracheal anastomosis was covered with musculocutaneous flap. Final histological findings of resected tumor specimens revealed well-differentiated PTC. The tumor mass could be detected macroscopically, in the resected specimen (Figure 8).
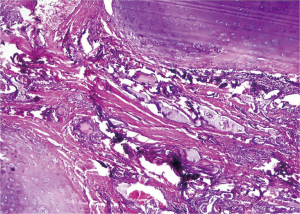
Histopathological examination confirmed invasion of a PTC into part of the resected trachea (pT4NXM0), stage IV according to pathological staging of Shin et al. (18). Figure 9 shows the pathological detail of tumor infiltration into the trachea. The detail shows that the tumor infiltration concerns not the cartilaginous rings but cartilaginous spaces in between (Figure 9). The gaps between the rings of cartilage, usually filled by the trachealis muscle, smooth muscle, fibroelastic tissue, connective tissue (the annular ligaments of trachea) are cautioned by tumor cells infiltration. The manner of invasion of PTC cells was by blunt dissection along blood vessels and collagen fibers oriented perpendicularly to the tracheal lumen in between cartilaginous rings. While, the tracheal rings appear non-infiltrated in all histological sections (Figure 9). The edge of the tracheal specimen was confirmed free from cancer.
Post-operative recovery was uneventful. The patient recovered satisfactorily without laryngeal dysfunction on the 9th postoperative day. Postoperative bronchoscopy revealed a white-coated part in the tracheal mucosa but no stenosis. The patient was then referred to receive complementary 131I treatment. The patient has been given hormone substitution. The patient remains alive and well 9 years after surgery without any evidence of recurrence or complaints.
Discussion
The trachea is composed of 15 to 20 incomplete C-shaped tracheal rings or tracheal cartilages, that reinforce the front and sides of the trachea to protect and maintain the airway (18-20). Each ring is of hyaline cartilage (20). The cartilages (around 4 mm deep and 1 mm thick) are placed horizontally above each other, separated by narrow intervals (20). The outer surfaces are directed vertically and the inner surfaces are convex due to the cartilages being thicker in the middle than at the margins (20). The first tracheal ring is broader than the rest, and often divided at one end; it is connected by the cricotracheal ligament with the lower border of the cricoid cartilage, and is sometimes blended with the next cartilage down (18). The last cartilage is thick and broad in the middle, due to its lower border being prolonged into a triangular hook-shaped (uncinate) process, which curves downward and backward between the two bronchi. It ends on each side in an imperfect ring, which encloses the commencement of the bronchus (20). The rings are generally highly elastic but they may calcify with age.
The trachealis muscle connects the ends of the incomplete rings and contracts during coughing, reducing the size of the lumen of the trachea to increase the rate of air flow (19). Circular horizontal bands of fibrous tissue called the annular ligaments of trachea join the tracheal rings together. The cartilaginous rings are incomplete to allow the trachea to collapse slightly so that food can pass down the esophagus. A flap-like epiglottis closes the opening to the larynx during swallowing to prevent swallowed matter from entering the trachea (19).
We have depicted in this case that the peculiarity of invasion of well differentiated PTC cells is perpendicularly oriented to the tracheal lumen, in between cartilaginous rings, along blood vessels and collagen fibers. Tracheal rings appear non-infiltrated in the histological sections of well differentiated PTC infiltrating the trachea (Figure 9). Similar description of inter-cartilage PTC infiltration into the trachea was first provided by Shin et al. in 1993 (18). Table 1 summarizes seven cases of thyroid carcinoma with tracheal invasion treated from 2000 through 2015. Interestingly, our pathological revision support the estimation by Shin et al., though that cartilage rings infiltration occur in poorly differentiated thyroid cancers with exiguous prognosis and severe symptoms as respiratory distress (18).

Full table
A broader, multi-institutional pathological review is needed to confirm these observations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Before collection of any clinical, pathological, radiological data from patients, written informed consent was obtained.
References
- Brauckhoff M. Classification of aerodigestive tract invasion from thyroid cancer. Langenbecks Arch Surg 2014;399:209-16. [Crossref] [PubMed]
- Brauckhoff M, Dralle H. Extrathyroidal thyroid cancer: results of tracheal shaving and tracheal resection. Chirurg 2011;82:134-40. [Crossref] [PubMed]
- Brauckhoff M, Dralle H. Cervicovisceral resection in invasive thyroid tumors. Chirurg 2009;80:88-98. [Crossref] [PubMed]
- Machens A, Hinze R, Dralle H. Surgery on the cervicovisceral axis for invasive thyroid cancer. Langenbecks Arch Surg 2001;386:318-23. [Crossref] [PubMed]
- Machens A, Hinze R, Lautenschläger C, et al. Thyroid carcinoma invading the cervicovisceral axis: routes of invasion and clinical implications. Surgery 2001;129:23-8. [Crossref] [PubMed]
- Dralle H, Scheumann GF, Meyer HJ, et al. Cervical interventions on the airway and esophagus in infiltrating thyroid cancer. Chirurg 1992;63:282-90. [PubMed]
- Kim H, Jung HJ, Lee SY, et al. Prognostic factors of locally invasive well-differentiated thyroid carcinoma involving the trachea. Eur Arch Otorhinolaryngol 2016;273:1919-26. [Crossref] [PubMed]
- Su SY, Milas ZL, Bhatt N, et al. Well-differentiated thyroid cancer with aerodigestive tract invasion: Long-term control and functional outcomes. Head Neck 2016;38:72-8. [Crossref] [PubMed]
- Shindo ML, Caruana SM, Kandil E, et al. Management of invasive well-differentiated thyroid cancer: an American Head and Neck Society consensus statement. AHNS consensus statement. Head Neck 2014;36:1379-90. [PubMed]
- Lin S, Huang H, Liu X, et al. Treatments for complications of tracheal sleeve resection for papillary thyroid carcinoma with tracheal invasion. Eur J Surg Oncol 2014;40:176-81. [Crossref] [PubMed]
- Chernichenko N, Shaha AR. Role of tracheal resection in thyroid cancer. Curr Opin Oncol 2012;24:29-34. [Crossref] [PubMed]
- Seo YL, Yoon DY, Lim KJ, et al. Locally advanced thyroid cancer: can CT help in prediction of extrathyroidal invasion to adjacent structures? AJR Am J Roentgenol 2010;195:W240-4. [Crossref] [PubMed]
- Ji YB, Tae K, Lee YS, et al. Surgical management of tracheal invasion by differentiated thyroid cancer: how we do it. Clin Otolaryngol 2009;34:565-7. [Crossref] [PubMed]
- Yang CC, Lee CH, Wang LS, et al. Resectional treatment for thyroid cancer with tracheal invasion: a long-term follow-up study. Arch Surg 2000;135:704-7. [Crossref] [PubMed]
- Zannini P, Melloni G. Surgical management of thyroid cancer invading the trachea. Chest Surg Clin N Am 1996;6:777-90. [PubMed]
- Pappalardo V, La Rosa S, Imperatori A, et al. Neck and mediastinum CT scan showing thyroid tumor and tracheal stenosis. Asvide 2016;3:401. Available online: http://www.asvide.com/articles/1172
- Pappalardo V, La Rosa S, Imperatori A, et al. CT airways 3-D reconstruction showing tracheal stenosis. Asvide 2016;3:402. Available online: http://www.asvide.com/articles/1173
- Shin DH, Mark EJ, Suen HC, et al. Pathologic staging of papillary carcinoma of the thyroid with airway invasion based on the anatomic manner of extension to the trachea: a clinicopathologic study based on 22 patients who underwent thyroidectomy and airway resection. Hum Pathol 1993;24:866-70. [Crossref] [PubMed]
- Allen MS. Surgery of the Trachea. Korean J Thorac Cardiovasc Surg 2015;48:231-7. [Crossref] [PubMed]
- Drevet G, Conti M, Deslauriers J. Surgical anatomy of the tracheobronchial tree. J Thorac Dis 2016;8:S121-9. [PubMed]